Diseases & Conditions
Plantar Fasciitis and Bone Spurs
Plantar fasciitis (fashee-EYE-tiss) is one of the most common causes of pain on the bottom of the heel. Approximately 2 million patients are treated for this condition every year.
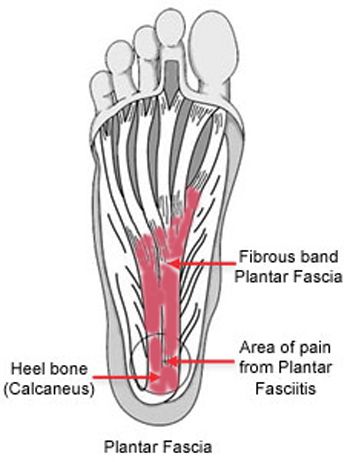
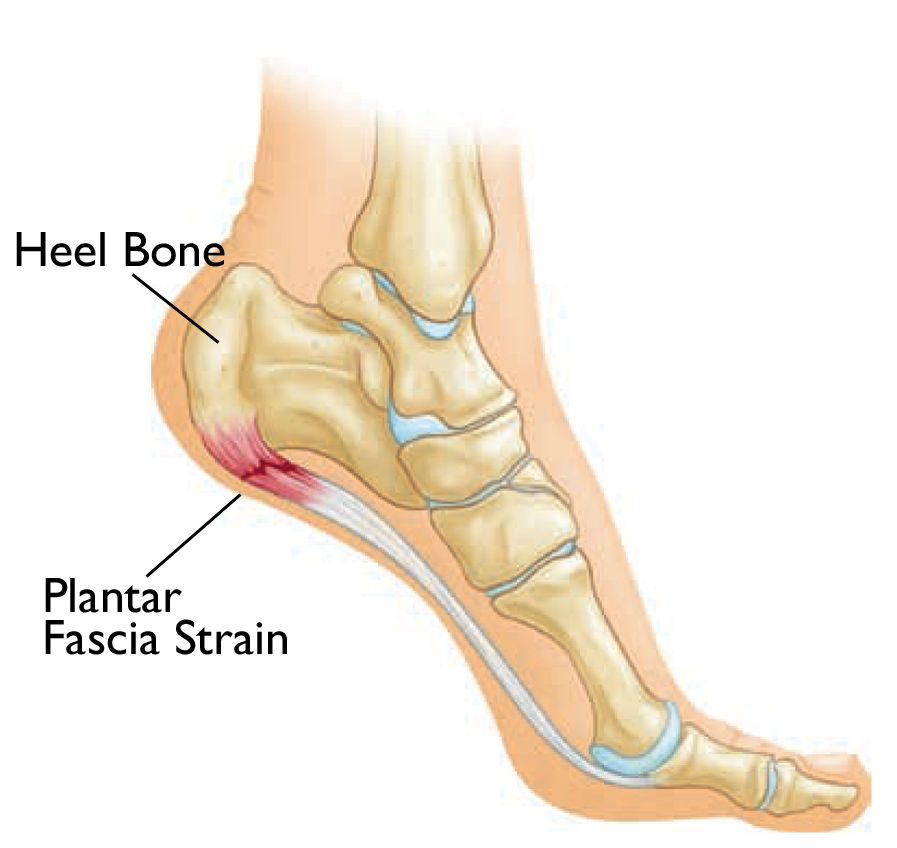
Plantar fasciitis occurs when the plantar fascia, a strong band of tissue that supports the arch of your foot, becomes irritated and inflamed.
Anatomy
The plantar fascia is a long, thin ligament that lies directly beneath the skin on the bottom of your foot. It connects the heel to the front of your foot and supports the arch of your foot.
Cause
The plantar fascia is designed to absorb the high stresses and strains we place on our feet when walking, running, and doing other activities like playing sports. But, sometimes, too much pressure damages or tears the tissues. The body's natural response to injury is inflammation, which results in the heel pain and stiffness of plantar fasciitis.
Risk Factors
In most cases, plantar fasciitis develops without a specific, identifiable reason. There are, however, many factors that can make you more prone to the condition:
- New or increased activity
- Repetitive high impact activity (running/dancing/sports)
- Prolonged standing on hard surfaces (especially among nurses, factory workers, and teachers)
- Anatomy (flat feet or a high arch)
- Tight calf muscles
- Obesity
- Age (plantar fasciitis is most common among people aged 40 to 60)
Symptoms
The most common symptoms of plantar fasciitis include:
- Pain on the bottom of the foot near the heel.
- Pain with the first few steps after getting out of bed in the morning, or after a long period of rest, such as after a long car ride. The pain goes away after a few minutes of walking
- Greater pain after (not during) exercise or activity.
Doctor Examination
After you describe your symptoms and discuss your concerns, your doctor will examine your foot. They will look for these signs:
- A high arch or flat foot
- An area of maximum tenderness on the bottom of your foot, just in front of your heel bone
- Limited dorsiflexion, or "up" motion, in your ankle
- The absence of symptoms from other conditions, such as insertional Achilles tendinitis, calcaneal (heel) stress fracture, or plantar nerve entrapment
Tests
Your doctor may order imaging tests to help make sure your heel pain is caused by plantar fasciitis and not another problem.
X-rays
X-rays provide clear images of bones. They are useful in ruling out other causes of heel pain, such as fractures or arthritis.
Heel spurs can be seen on an X-ray. A heel spur can be the result of longstanding (occurring for a long time) tension on the plantar fascia insertion (the spot on the heel bone where the plantar fascia attaches). However, most people who have bone spurs on their heels do not have heel pain. Since heel bone spurs are not the cause of plantar fasciitis, plantar fasciitis pain can be treated without removing the spur.
Other Imaging Tests
Other imaging tests, such as magnetic resonance imaging (MRI) and ultrasound, are not routinely used to diagnose plantar fasciitis. They are rarely ordered.
An MRI scan may be used if the heel pain is not relieved by initial treatment methods or if your doctor is concerned that a different problem is causing your heel pain.
Treatment
Nonsurgical Treatment
More than 90% of patients with plantar fasciitis will improve within 10 months of starting simple treatment methods.
Rest. Decreasing or even stopping the activities that make the pain worse is the first step in reducing the pain. You may need to stop athletic activities where your feet pound on hard surfaces (for example, running, dancing, or step aerobics). Your doctor may recommend that you use a walking boot and crutches for a short period of time to allow your foot to rest.
Changing your activity. Low impact exercise, such as cycling or swimming, puts less stress on your joints and feet than walking or running.
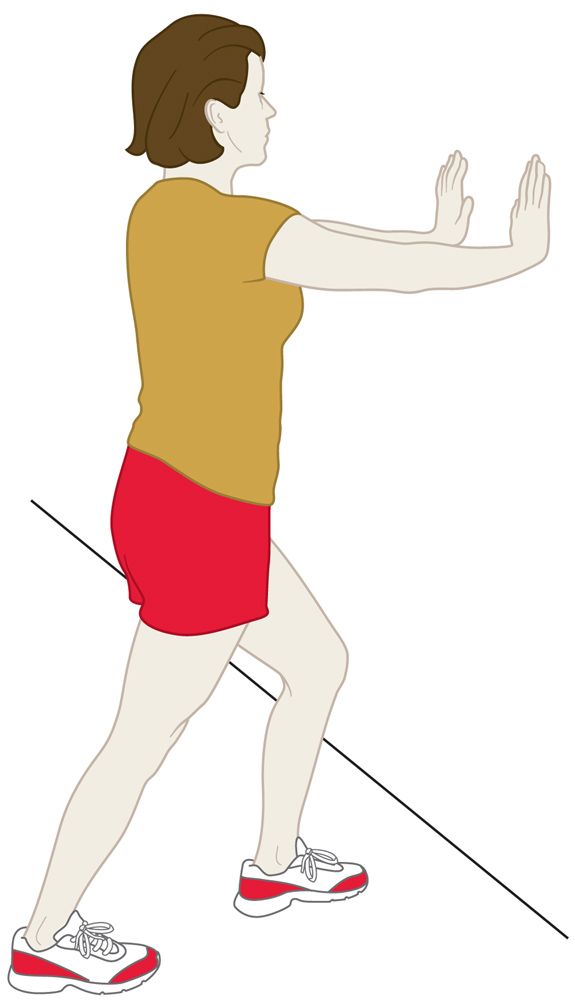
Stretching. Plantar fasciitis is aggravated by tight muscles in your feet and calves. Stretching your calves and plantar fascia is the most effective way to relieve the pain that comes with this condition.
- Calf stretch
Lean forward against a wall with one knee straight and the heel on the ground. Place the other leg in front, with the knee bent. To stretch the calf muscles and the heel cord, push your hips toward the wall in a controlled fashion. Hold the position for 10 seconds and relax. Repeat this exercise 20 times for each foot. A strong pull in the calf should be felt during the stretch. - Plantar fascia stretch
This stretch is performed in the seated position. Cross your affected foot over the knee of your other leg. Grasp the toes of your painful foot and slowly pull them toward you in a controlled fashion. If it is difficult to reach your foot, wrap a towel around your big toe to help pull your toes toward you. Place your other hand along the plantar fascia. The fascia should feel like a tight band along the bottom of your foot when stretched. Hold the stretch for 10 seconds. Repeat it 20 times for each foot. This exercise is best done in the morning before standing or walking.
Ice. Rolling your foot over a cold water bottle or ice for 20 minutes is effective. This can be done 3 to 4 times a day.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Medications such as ibuprofen or naproxen reduce pain and inflammation. Using the medication for more than 1 month should be reviewed with your primary care doctor.
Physical therapy. Your doctor may suggest that you work with a physical therapist on an exercise program that focuses on stretching your calf muscles and plantar fascia. In addition to exercises like the ones mentioned above, a physical therapy program may involve specialized ice treatments, massage, and other therapies to decrease inflammation around the plantar fascia.
Supportive shoes and orthotics. Shoes with thick soles and extra cushioning can reduce pain with standing and walking. As you step and your heel strikes the ground, a large amount of tension is placed on the fascia, which causes microtrauma (tiny tears in the tissue). A cushioned shoe or insert reduces this tension and the microtrauma that occurs with every step. Soft silicone heel pads are inexpensive and work by elevating (raising) and cushioning your heel. Pre-made or custom orthotics (shoe inserts) are also helpful.
Avoid shoes that do not provide support or are worn out. Make sure to replace your old athletic shoes before they wear out and no longer support your feet.
Night splints. Most people sleep with their feet pointed down. This relaxes the plantar fascia and is one of the reasons for morning heel pain. A night splint stretches the plantar fascia while you sleep. Although it can be difficult to get used to, a night splint is very effective at reducing heel pain from plantar fasciitis.
Other Treatments
Your doctor may recommend the following procedures if you still have symptoms after several months of nonsurgical treatments.
Casting. Wearing a cast for a short period of time can be very helpful in the treatment of plantar fasciitis because it keeps your foot from moving, which is a better environment for healing. Since a cast is custom-molded to your foot and cannot be removed, it is often a better option than wearing a boot.
Cortisone injections. Cortisone, a type of steroid, is a powerful anti-inflammatory medication. It can be injected into the plantar fascia to reduce inflammation and pain.
Your doctor may limit this treatment or avoid it altogether because steroid injections can weaken the plantar fascia and lead to a rupture (tear), which can lead to flattening of the foot and chronic pain.
Platelet-rich plasma (PRP) injections. PRP is obtained from your own blood and can be injected into the plantar fascia to promote healing. PRP injections do not have the same risk of leading to plantar fascia rupture. However, this treatment can be expensive, and more research is needed on the effectiveness of PRP injections.
Extracorporeal shockwave therapy (ESWT). During this procedure, high-energy shockwave impulses stimulate the healing process in damaged plantar fascia tissue. ESWT has not shown consistent results and, therefore, is not commonly performed.
ESWT is noninvasive, meaning it does not require a surgical incision. Because of the minimal (low) risk involved, ESWT is sometimes tried before surgery is considered.
Ultrasonic tissue repair. This is a minimally invasive treatment for patients with persistent (ongoing) plantar fasciitis. Ultrasound imaging is used to guide a probe toward the injured plantar fascia. The tip of the probe then vibrates to break up and remove damaged tissue.
Surgical Treatment
Because more than 90% of patients with plantar fasciitis recover with nonsurgical treatment, surgery is generally saved for people who have not seen improvement after 12 months of aggressive nonsurgical treatment.
Gastrocnemius recession. This is a surgical lengthening of the calf (gastrocnemius) muscles. Because tight calf muscles place increased stress on the plantar fascia, this procedure is useful for patients who still have difficulty flexing their feet, despite extensive efforts at calf stretching.
In gastrocnemius recession, one of the two muscles that make up the calf is lengthened to increase the motion of the ankle. The procedure can be performed with a traditional, open incision or with a smaller incision and an endoscope, an instrument that contains a small camera. Your doctor will discuss the procedure that best meets your needs.
Complication rates for gastrocnemius recession are low, but can include damage to the sural nerve and calf weakness.
Partial plantar fascia release. Often performed at the same time as a gastrocnemius recession, a partial plantar fascia release involves making an incision on the bottom or side of the heel. The surgeon identifies the plantar fascia insertion at the heel (the spot where the ligament attaches to the bone) and makes a partial cut to relieve tension in the tissue. If there is a large bone spur, it can also be removed.
Although the surgery can be performed endoscopically, it is more difficult than with an open incision. In addition, endoscopy has a higher risk of nerve damage than open surgery.
- Complications. The most common complications of release surgery include nerve damage and not fully relieving pain.
- Recovery. A short period of protected weightbearing is recommended after surgery to allow the incision to heal.
Most patients have good results with surgery. However, because surgery can result in chronic pain and dissatisfaction, it is recommended only after trying all nonsurgical treatments.
Contributed and/or Updated by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.