Treatment
Finger (IP Joint) Fusion
Interphalangeal (IP) joint arthrodesis (fusion) is a procedure where a finger joint is prepared and held in a defined position until it heals there. The end result is elimination of motion at that joint by making the two ends of the bone grow (fuse) together.
- Fusion is usually reserved for patients with severe, painful arthritis of the affected joint — in this case, either the fingers or thumb.
- It can also be used for patients with chronic joint instability, deformity, or other conditions affecting the function of the finger/thumb/joint.
Fusion robs the joint of motion in exchange for stability, improved alignment, and reduction in pain. Because the procedure typically cannot be reversed, it is performed only after careful consideration and involves shared decision-making between the patient and surgeon.
In patients with pain that seriously limits function or who have extreme deformity of the finger or thumb IP joint, arthrodesis (fusion) can greatly improve quality of life and reduce pain.
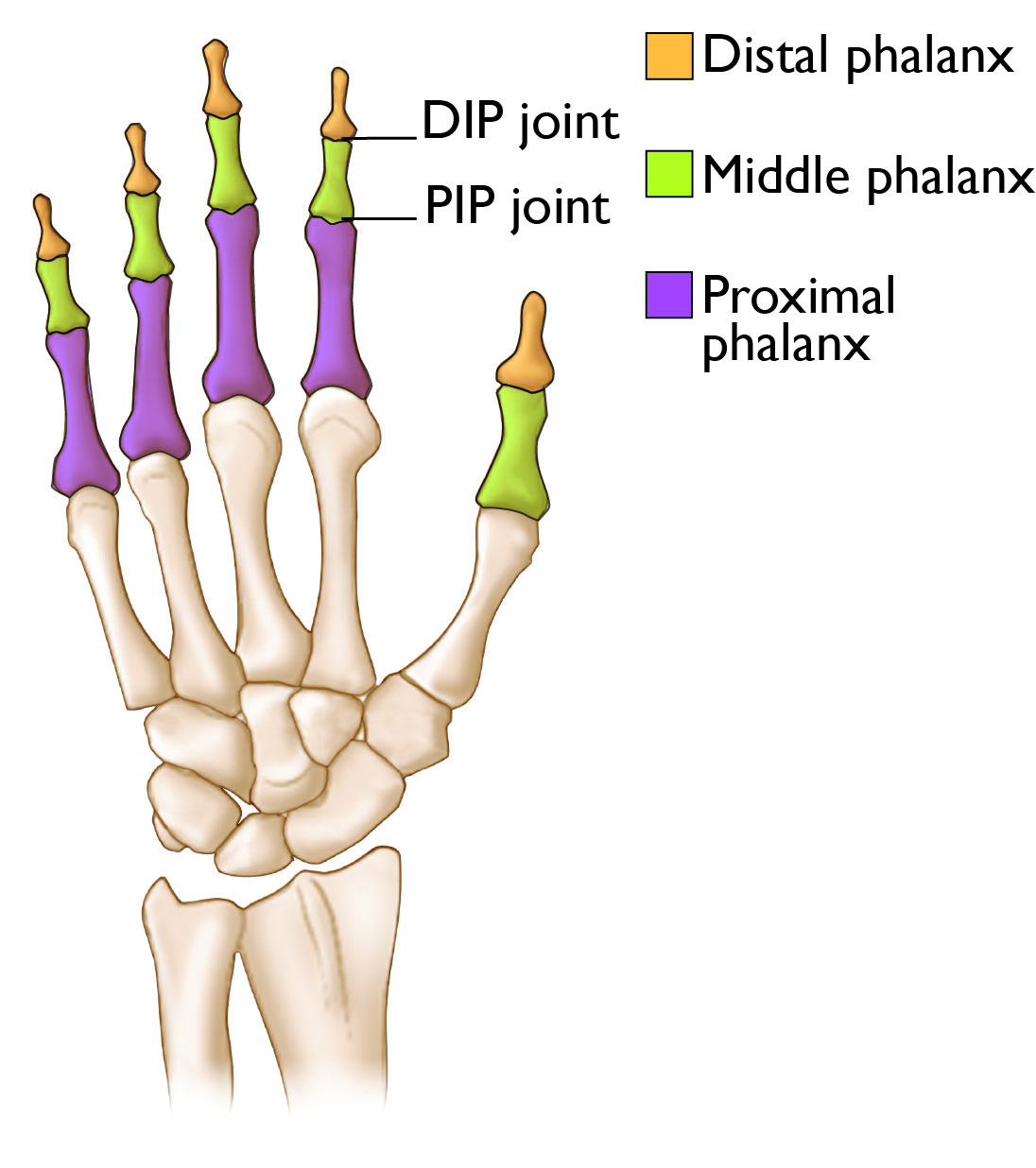
Anatomy
The interphalangeal joints are the joints in the middle and at the end of the fingers and in the middle of the thumb. They allow the fingers and thumb to straighten (e.g., to point) and flex (e.g., to grab an object).
The fingers have two IP joints:
- The distal interphalangeal (DIP) joint at the very end of the finger
- The proximal interphalangeal (PIP) joint in the middle of the finger
The thumb has one IP joint at the junction between the middle and end of the thumb.
The DIP joint is more commonly fused than the PIP joint or thumb IP joint.
The IP joints are essentially hinge joints, similar to the hinges on a cabinet, that allow the fingers and thumb to straighten and bend. The motion of the joints is controlled by tendons that pass the joint beneath and above it. The IP joints are held together by ligaments and a joint capsule that surrounds the joint.
Aging (osteoarthritis), trauma to the finger or thumb, disease (rheumatoid arthritis), infection, gout, etc. can all contribute to dysfunction or pain of the IP joints resulting in poor finger function, pain, and deformity.
Nonsurgical Treatment
In many cases, non-operative treatments will be tried prior to the surgery. This may include:
- Splints
- Anti-inflammatory medication
- Pain relieving measures, such as wrapping the joints or altering activity
- Steroid injections
If these treatments do not work, or the surgeon believes the condition is too severe to avoid surgery, then surgery is recommended. As mentioned above, fusion typically cannot be reversed, so make sure to discuss and carefully weigh the pros and cons of the procedure with your surgeon.
Preparing for the Procedure
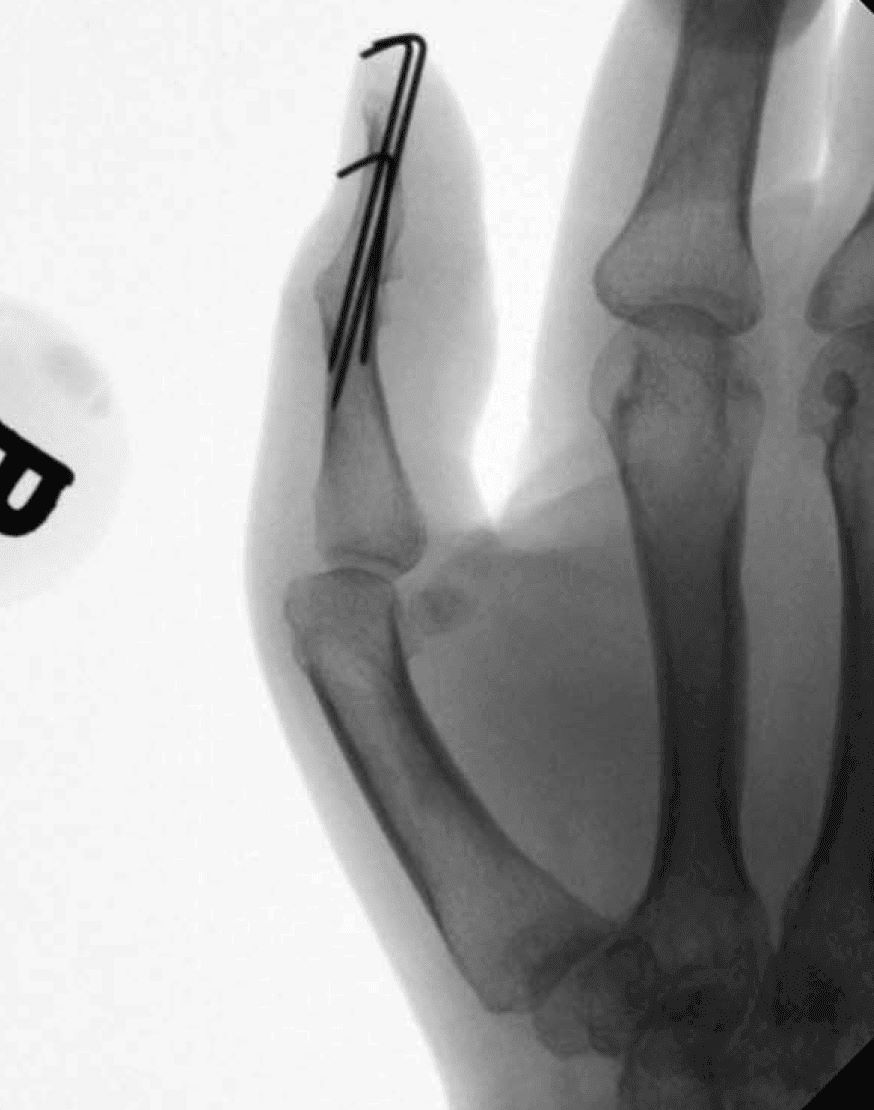
Typically, you will have X-rays before your surgery. X-rays help your surgeon:
- See how severe the arthritis is.
- Determine whether there are other conditions that need to be treated at the time of surgery.
- Plan how the surgery will be performed, in some cases. IP joint arthrodesis (fusion) can be performed in a variety of ways, including with the use of pins, screws, plates, and/or wires to hold the bones together.
Prior to surgery:
- Patients should avoid injury to the skin over the affected digit. If a wound is present over the surgical site prior to the operation, the procedure may be delayed to prevent infection.
- If you are diabetic, you will be encouraged to keep your blood sugar control as tight as possible. This reduces the risk of post-operative infection and wound issues.
- Smokers will typically be encouraged to avoid smoking for several weeks or more prior to the surgery to reduce the risk of infections, healing problems and wound complications. Smokers may also be at increased risk of nonunion after the surgery. A nonunion is when the joint does not heal in the position selected and continues to move (painfully) around the fixation. This is a potential complication of the surgery that could require a return to the operating room.
Patients should expect to be sore after surgery for several days to weeks. Make arrangements at home and at work to account for this.
- People with sedentary jobs (e.g., working at a computer) may be able to return to work just a few days after surgery.
- Patients with physically demanding jobs (e.g., construction or warehouse workers) will likely need to take a longer time off after surgery to allow their wound(s) and arthrodesis (fusion) site to heal. You should address the recovery period with your employer ahead of time.
Procedure
During the surgery, the patient is often made sleepy and the surgical site is numbed with medication. Sometimes, prior to the surgery, the entire arm may be numbed by an anesthesiologist in a procedure known as a "block." This leads to excellent pain control during and after the surgery in many cases.
Some surgeons will apply a tourniquet to the arm (or finger) to prevent bleeding during the surgery. Some surgeons will keep the patient awake during the surgery and use numbing medicine and blood vessel constricting medicine to provide pain control and prevent bleeding during the surgery without using a tourniquet. This is called wide awake local anesthesia no torniquet (WALANT) surgery.
For the procedure:
- Typically, the surgeon makes an incision over the joint on the nail side of the finger. The joint is opened so that the surgeon can access the joint surfaces. The joint surfaces are prepared with tools to make them match each other well and expose the healthy/bleeding bone just below the joint.
- Bone spurs, loose bodies, or other issues related to arthritis may also be addressed at this time.
- The joint is aligned so the finger is straight from an overhead view and straight or, in some cases, slightly bent from a side view.
- The joint is then held in this position with the joint surfaces pressed against each other so they can heal together.
- For the DIP joint or thumb IP joint, this is commonly achieved with a small screw (or multiple screws) that buries all the way in the bone so it cannot be felt after surgery.
- For the PIP joint, this can be accomplished with pins, screws, wires, plates, or other devices designed for this purpose.
During the surgery, X-rays are performed to ensure proper alignment of the fused joint and placement of the hardware.
When the surgeon is satisfied with the surgical result:
- The wound is washed with a saltwater solution (saline)
- The tourniquet is removed.
- Bleeding is treated with a cautery device that seals the bleeding vessels.
- The wound is then sutured (stitched) together and cleaned.
- A bandage and splint are applied.
In total, this procedure takes about 30 to 60 minutes depending on the joint being fused and the severity of the arthritis/deformity prior to surgery. It is almost always done on an outpatient basis, meaning the patient gets to go home after surgery and does not have to stay overnight in the hospital.
Recovery
Patients are commonly groggy from anesthesia the day of surgery, so you will need to be driven home by a family member or friend. You will not be able to drive yourself home, or use a rideshare/cab or public transportation by yourself.
- You will need some rest as the anesthesia wears off. If a block was done, your arm will be numb and weak for several hours up to a few days.
- You may be given a sling in the recovery area to use until strength comes back in your arm.
- The pain after surgery may not start for a few hours or even a few days due to the numbing medication/block given for the procedure.
Patients may be sent home with prescription pain medicine, which can be used for pain the first few days after surgery. Many patients find that acetaminophen and ibuprofen are enough and do not need narcotic medications, such as opioids.
Opioids can provide excellent pain relief; however, their use has risks and complications. These medications can be addictive and potentially dangerous. It is therefore important to use opioids only as directed by your doctor, to use as little as possible for as short a time as possible, and to stop taking them as soon as your pain starts to improve.
Antibiotics are not commonly needed after surgery and will not be prescribed in most cases.
As mentioned above, patients with sedentary professions may feel up to returning to work a few days after surgery. Those with labor-intensive positions may need more time off from work.
The dressing and splint are commonly left on for 10 to 14 days after surgery to keep the wound sterile and keep stress off of the fused joint.
After that initial 10- to 14-day period, the bandage can be removed and patients can shower. Clean and running water is safe at this time; however, the wound should not be submerged in stagnant water such as an ocean, lake, pool, bathtub, or hot-tub for about 30 days after surgery.
Once the bandage is removed, patients typically are placed in a removable splint and start therapy for gentle motion of the other fingers and the other joints around the fused joint.
Most patients have soreness and stiffness for several weeks after surgery. It will likely take around 6 to 12 weeks for the surgery to start to feel beneficial. Many surgeons counsel their patients that it can take 9 to 12 months after surgery to see the final results.
Most patients are ultimately happy with the surgery. It has excellent rates of pain improvement and functional benefits. Patients should clearly understand before having the surgery that the fused joint will never move again; the position the joint is in after surgery is permanent.
Complications
Complications from surgery can include:
- Infection
- Wound healing issues
- Injuries to nearby structures such as nerves/vessels/tendons
- Lack of improvement after surgery
- Failure of the surgery
- Hardware issues with the implants used for fixing the fusion
- Nonunion
Patients with compromised immune systems, diabetics, and smokers may be at increased risk for complications. You should discuss any concerns you have about your personal risks with your surgeon prior to surgery.
Long-Term Outcomes
Overall, long-term outcomes of IP joint arthrodesis (fusion) are quite good. In general, most patients are happy with their result. The surgery reliably corrects finger deformities and reduces or eliminates pain.
Nonunion after an attempt at arthrodesis (fusion) is rare. When it does happen, it can often be addressed with a return to the operating room to redo the surgery.
As mentioned above, it commonly takes patients about 6 to 12 months to be happy with the procedure. In those rare patients who do not improve after surgery, revision (repeat) surgery may be necessary.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.