Diseases & Conditions
Osteogenesis Imperfecta
Osteogenesis imperfecta (OI) literally means "imperfectly formed bone." People with osteogenesis imperfecta have a genetic defect that impairs the body's ability to make strong bones.
OI is a relatively rare condition. Some people have a more severe form of the disorder in which their bones break easily. They may break hundreds of bones during their lives. Many people, however, have a milder form of OI and go through life with few fractures.
Cause
In people with osteogenesis imperfecta, one of the genes that tells the body how to make a specific protein does not function. This protein (type I collagen) is a major component of the connective tissues in bones. Type I collagen is also important in forming ligaments, teeth, and the white outer tissue of the eyeballs (sclera).
As a result of the defective gene, not enough type I collagen is produced, or the collagen that is produced is of poor quality. In either case, the result is fragile bones that break easily but can heal at a normal rate.
In most cases of OI, children inherit the defective gene from one of their parents. But the child's symptoms and the degree of disability can be very different from that of the parent.
In some children, neither parent has osteogenesis imperfecta. In these cases, the genetic defect is a spontaneous mutation (change) in the gene, and it stops functioning correctly.
Symptoms and Signs
There are different types of osteogenesis imperfecta, with symptoms that range from mild to severe. Each person with the condition may have a different combination of symptoms. All people with OI, however, have weaker bones.
Some common symptoms of OI include:
- Short stature
- Triangular-shaped face
- Breathing problems
- Hearing loss
- Brittle teeth
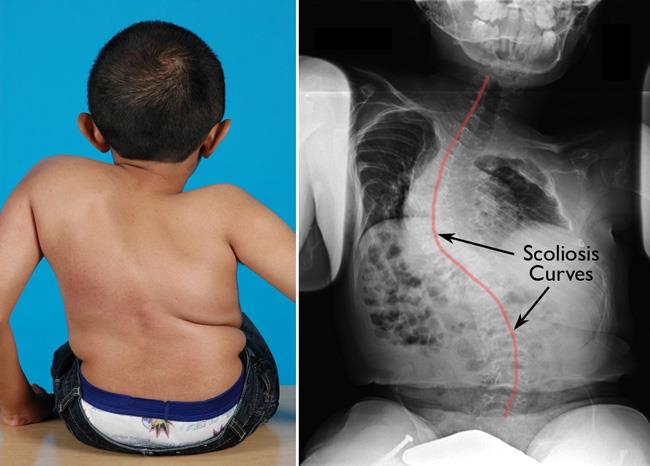
- Bone deformities, such as bowed legs or scoliosis
Description
In many children with OI, the number of times their bones fracture decreases significantly as they mature. However, osteogenesis imperfecta may become active again after menopause in women or after the age of 60 in men.
Scoliosis, or curvature of the spine, is a problem for many children with osteogenesis imperfecta.
There are several types of OI, and they vary in severity and characteristics. As scientists have discovered new genetic problems causing OI, new types of the disorder have been recognized. All types of the disorder, however, have symptoms and severity that fall somewhere within the range of the first four types recognized. These four types are described below.
Type I
Type I osteogenesis imperfecta is the most common and mildest type of this disease. While the structure of the collagen is normal, there is less collagen than there should be. There is little or no bone deformity, although the bones are fragile and easily broken. The effects of OI may extend to the teeth, making them prone to cavities and cracking. The whites of the eyes may have a blue, purple, or gray tint.
Type II
Type II osteogenesis imperfecta is the most severe form of the disease. The collagen does not form properly. Bones may break even while the fetus is in the womb. Many infants with type II osteogenesis imperfecta do not survive.
Type III
Children with type III osteogenesis imperfecta also have improperly formed collagen and often severe bone deformities, plus additional complications. The infant is often born with fractures. The whites of the eyes may be white, blue, purple, or gray. People with type III osteogenesis imperfecta are generally shorter than average. They may have spinal deformities, respiratory complications, and brittle teeth.
Type IV
Type IV osteogenesis imperfecta is moderately severe, with improperly formed collagen. Bones fracture easily, but the whites of the eyes are normal. Some people with type IV osteogenesis imperfecta may be shorter than average and may have brittle teeth. Bone deformities are mild to moderate.
Doctor Examination
In many cases, broken bones that occur with little or no force are the first sign of osteogenesis imperfecta, and will cause your doctor to suspect the condition.
Medical History and Physical Examination
Because osteogenesis imperfecta is often inherited, your doctor will discuss family medical history in addition to your child's medical history. Your doctor will also complete a thorough physical examination that includes checking your child's eyes and teeth.
Tests
- X-rays. X-rays will provide your doctor with clear images of your child's bones, showing fractures as well as malformations of bone.
- Laboratory tests. Your doctor may take blood or tissue samples for genetic testing. In many cases, these tests are able to identify the mutation, particularly if the parent's mutation is also known.
- Ultrasound. Ultrasound can often detect severe cases of osteogenesis imperfecta during pregnancy.
Treatment
While there is no cure for osteogenesis imperfecta, there are ways to improve a child's quality of life. Treatment is individualized and depends on the severity of the disease and the age of the patient. Care is provided by a team of healthcare professionals, including several types of doctors, a physical therapist, a nurse-clinician, and a social worker. Support from a social worker or psychologist is very helpful for both the child and the family, and often becomes even more important during adolescence.
Nonsurgical Treatment
In most cases, treatment is nonsurgical.
- Medication. Medical bisphosphonates, given to the child either by mouth or intravenously, slow down bone resorption. In children with more severe osteogenesis imperfecta, bisphosphonate treatment often reduces bone pain and the number of fractures. These medications must be administered by properly trained doctors and require close monitoring.
- Immobilization. Casting, bracing, or splinting fractures is necessary to keep the bones still and in line so that healing can occur.
- Exercise. After a fracture, movement and weight bearing are encouraged as soon as the bone has healed. Specific exercises will increase mobility and decrease the risk of future fractures. Low-impact exercise, such as swimming and walking, can help strengthen bones and the muscles that support them. Exercise is part of a healthy lifestyle for every child.
Surgical Treatment
Surgery may be recommended in cases of:
- Repeated fractures of the same bone
- Fractures that do not heal properly
- Bone deformity, such as scoliosis
Rodding. Metal rods may be inserted in the long bones of the arms and legs to help reinforce the bone, and subsequently lessen the number of fractures. Some rods are a fixed length and must be replaced as a child grows. Other rods are designed like telescopes, and they expand as a child's bones grow. There are, however, other complications that may occur with telescoping rods. Do not hesitate to ask your orthopaedic surgeon about both rodding options.
Spinal fusion for scoliosis. Although bracing is the usual treatment for scoliosis, it is not often effective in children with osteogenesis imperfecta because the ribs will become deformed from the brace, without preventing the scoliosis from worsening. The doctor may recommend spinal fusion, a surgery in which the bones of the spine are realigned and fused together, when the scoliosis becomes severe.
Living with Ostogenesis Imperfecta
Below are some tips developed by the Osteogenesis Imperfecta Foundation for taking care of children with osteogenesis imperfecta. Most important, do not feel guilty if your child breaks a bone. Children must grow and develop, and fractures will occur no matter how careful you are.
- Do not be afraid to touch or hold an infant with osteogenesis imperfecta, but be careful. To lift an infant with osteogenesis imperfecta, spread your fingers apart and put one hand between the legs and under the buttocks. Place the other hand behind the shoulders, neck, and head.
- Never lift a child with osteogenesis imperfecta by holding them under the armpits.
- Do not pull on arms or legs or, in those with severe osteogenesis imperfecta, lift the legs by the ankles to change a diaper.
- Select an infant car seat that reclines. It should be easy to place your child in the seat and remove them. Consider padding the seat with foam and placing a layer of foam between your child and the harness.
- Be sure your stroller is large enough to accommodate casts. Do not use a sling- or umbrella-type stroller.
- Follow your doctor's instructions carefully, especially with regard to cast care and mobility exercises. Swimming and walking are often recommended as safe exercises.
- Adults with OI should avoid activities such as smoking, drinking, and taking steroids because they have a negative impact on bone density.
- Increasing awareness of child abuse and a lack of understanding about osteogenesis imperfecta may lead to inaccurate conclusions about a family situation. Always have a letter from your family doctor and a copy of your child's medical records handy in case child abuse is suspected after a fracture.
Last Reviewed
June 2021
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.