Recovery
Care of Casts and Splints
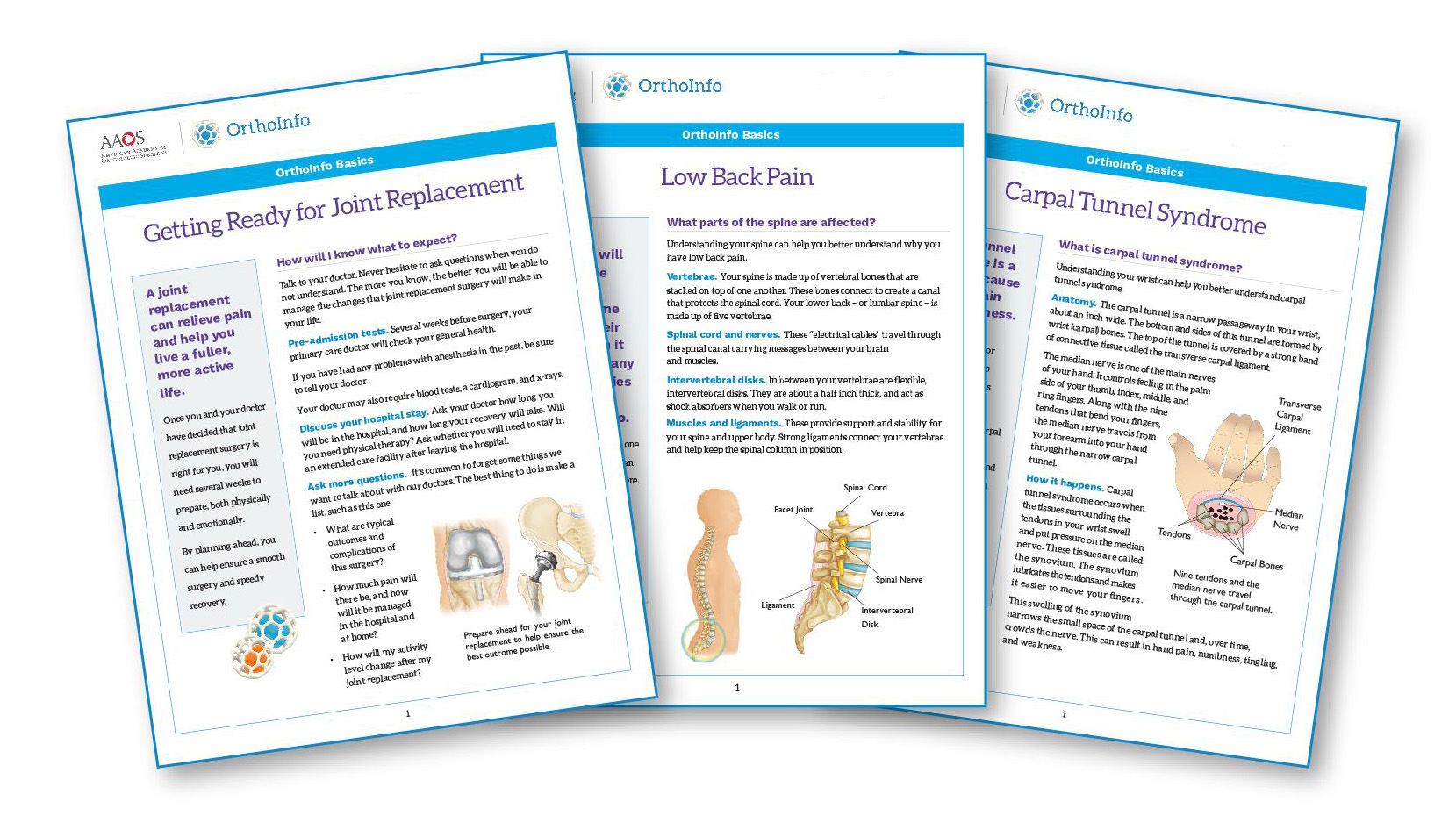
Casts and splints support and protect injured bones and soft tissue. When you break a bone, your doctor will put the pieces back together in the right position. Casts and splints hold the bones in place while they heal. They also reduce pain, swelling, and muscle spasms.
In some cases, splints and casts are applied following surgery.
Splints, otherwise known as half-casts, provide less support than casts. However, splints can be adjusted to accommodate swelling from injuries easier than enclosed casts. Your doctor will decide which type of support is best for you.
Types of Splints and Casts
Casts are custom-made. They must fit the shape of your injured limb correctly to provide the best support. Casts can be made of plaster or fiberglass — a plastic that can be shaped.
Splints, or half-casts, can also be custom-made, especially if an exact fit is necessary.
Other times, a ready-made splint will be used. These off-the-shelf splints are made in a variety of shapes and sizes and are much easier and faster to use. There is typically a metal or hard plastic component to provide support to the injured limb. Some have Velcro straps, which make the splints easy to put on, take off, and adjust.
Materials
Fiberglass or plaster materials form the hard, supportive layer in splints and casts. What is the difference between these two materials?
- Fiberglass is lighter in weight and stronger than plaster.
- X-rays can see through fiberglass better than through plaster. This is important because your doctor will probably schedule additional X-rays after your splint or cast has been applied. X-rays can show whether the bones are healing well or have moved out of place.
- Plaster is less expensive than fiberglass.
- Plaster shapes better than fiberglass for some uses.
Application
Both fiberglass and plaster splints and casts use padding, usually cotton, as a protective layer next to the skin. Both materials come in strips or rolls, which are dipped in water and applied over the padding covering the injured area.
In some cases, special waterproof padding and cast material may be used. Your doctor will let you know if your cast is made and padded with these waterproof materials.
The splint or cast must fit the shape of the injured arm or leg correctly to provide the best possible support. Generally, the splint or cast also covers the joint above and below the broken bone.
In many cases, a splint is applied to a fresh injury first. As swelling subsides, a full cast may replace the splint. If a cast is initially applied to your injury, it may be “valved” (cut) to allow for swelling, then repaired (overwrapped) at your first follow-up appointment.
Sometimes, it may be necessary to replace a cast as swelling goes down and the cast gets too big. As a fracture heals, the cast may be replaced by a splint to make it easier to perform physical therapy exercises.
Getting Used to a Splint or Cast
Swelling due to your injury may cause pressure in your splint or cast for the first 48 to 72 hours (2 to 4 days). This may cause your injured arm or leg to feel snug or tight in the splint or cast. If you have a splint, your doctor will show you how to adjust it to accommodate the swelling.
It is very important to keep the swelling down. This will lessen pain and help your injury heal. To help reduce swelling:
- Elevate. It is very important to elevate your injured arm or leg for the first 24 to 72 hours (2 to 4 days). Prop your injured arm or leg up above your heart by putting it on pillows or some other support. You will have to recline if the splint or cast is on your leg. Elevation allows clear fluid and blood to drain "downhill" to your heart.
- Exercise. Move your uninjured, but swollen fingers or toes gently and often. Moving them often will prevent stiffness.
- Ice. Apply ice to the splint or cast. Place the ice in a dry plastic bag or ice pack and loosely wrap it around the splint or cast at the level of the injury. Ice that is packed in a rigid container and touches the cast at only one point will not be effective.
Warning Signs
Swelling can create a lot of pressure under your cast. This can lead to problems. If you experience any of the following symptoms, contact your doctor's office immediately for advice.
- Increased pain and the feeling that the splint or cast is too tight. This may be caused by swelling.
- Numbness and tingling in your hand or foot. This may be caused by too much pressure on the nerves.
- Burning and stinging. This may be caused by too much pressure on the skin.
- Excessive swelling below the cast. This may mean the cast is slowing your blood circulation.
- Loss of active movement of toes or fingers — meaning they cannot move on their own. This requires an urgent evaluation by your doctor.
Taking Care of Your Splint or Cast
Your doctor will explain any restrictions on using your injured arm or leg while it is healing. You must follow your doctor's instructions carefully to make sure your bone heals properly. The following information provides general guidelines only and is not a substitute for your doctor's advice.
After you have adjusted to your splint or cast for a few days, it is important to keep it in good condition. This will help your recovery.
- Moisture. It is essential to keep your cast dry. Moisture weakens plaster, and damp padding next to the skin can cause irritation. Use 2 layers of plastic or purchase waterproof shields to keep your splint or cast dry while you shower or bathe. Even if the cast is covered, do not submerge it (place it into standing water, such as in a bathtub, sink, or pool) or hold it under running water (faucet, hose, etc.). A small pinhole in the cast cover can cause the injury to get soaked.
- Walking on a walking cast. Do not walk on a walking cast until it is completely dry and hard. It takes about 1 hour for fiberglass, and 2 to 3 days for plaster to become hard enough to walk on. You will be given a cast shoe to wear over your walking cast. The cast shoe will help protect the bottom of the cast.
- Dirt and sand. Keep dirt and sand away from the inside of your splint or cast.
- Padding. Do not pull out the padding from your splint or cast.
- Itching. Do not stick objects such as coat hangers inside the splint or cast to scratch itching skin. If something gets stuck inside your cast, it may irritate your skin. Also, do not apply powders or deodorants to itching skin inside the spint or cast.
- Trimming. Do not break off rough edges of the cast or trim the cast before asking your doctor.
- Skin. Inspect the skin around the cast to make sure the skin looks healthy.
- Damage. Inspect the cast regularly to make sure there are not any issues that need to be addressed.
Contact your doctor if:
- Itching persists (continues)
- Something gets stuck inside your cast
- The skin around the cast becomes red or raw
- The cast becomes cracked or develops soft spots
After the initial swelling has subsided, proper splint or cast support will usually allow you to continue your daily activities with a minimum of inconvenience.
Cast Removal
Never remove the cast yourself. You may cut your skin or prevent proper healing of your injury.
Your doctor will use a cast saw to remove your cast. The saw vibrates but does not rotate. If the blade of the saw touches the padding inside the hard shell of the cast, the padding will vibrate with the blade and will protect your skin. Cast saws make noise and may feel hot from friction, but they will not harm you.
If you do feel pain while the cast is being removed, let your doctor or an assistant know, and they will be able to adjust.
Rehabilitation
Broken bones take several weeks to several months to heal. Pain usually stops long before the bone is solid enough to handle the stresses of everyday activities. You will need to wear your cast or splint until your bone is fully healed and can support itself.
While you are wearing your cast or splint, you will likely lose muscle strength in the injured area. Exercises during the healing process and after your cast is removed are important. They will help you restore normal muscle strength, joint motion, and flexibility.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.