Diseases & Conditions
Thighbone (Femur) Fractures in Children
The femur (thighbone) is the largest and strongest bone in the body. In a child, the femur can break as the result of a sudden forceful impact. About 1.7% of pediatric fractures occur in the femur.
Anatomy
The femur extends from the hip to the knee. The long, straight part of the femur is called the femoral shaft. When there is a break anywhere along this length of bone, it is called a femoral shaft fracture.
Cause
- The most common cause of thighbone fractures in infants under 6 months old is child abuse.
- For infants 6 to 12 months old, the most common cause is a fall from a height, like rolling off of a bed or changing table.
- Child abuse is also a leading cause of thighbone fracture in children between the ages of 1 and 4 years, but the incidence is less in this age group.
- In adolescents, motor vehicle collisions (when the child is either riding in a car or on a bicycle, or is a pedestrian) are responsible for the vast majority of femoral shaft fractures. Other common causes include falling hard on the playground and taking a hit in contact sports.
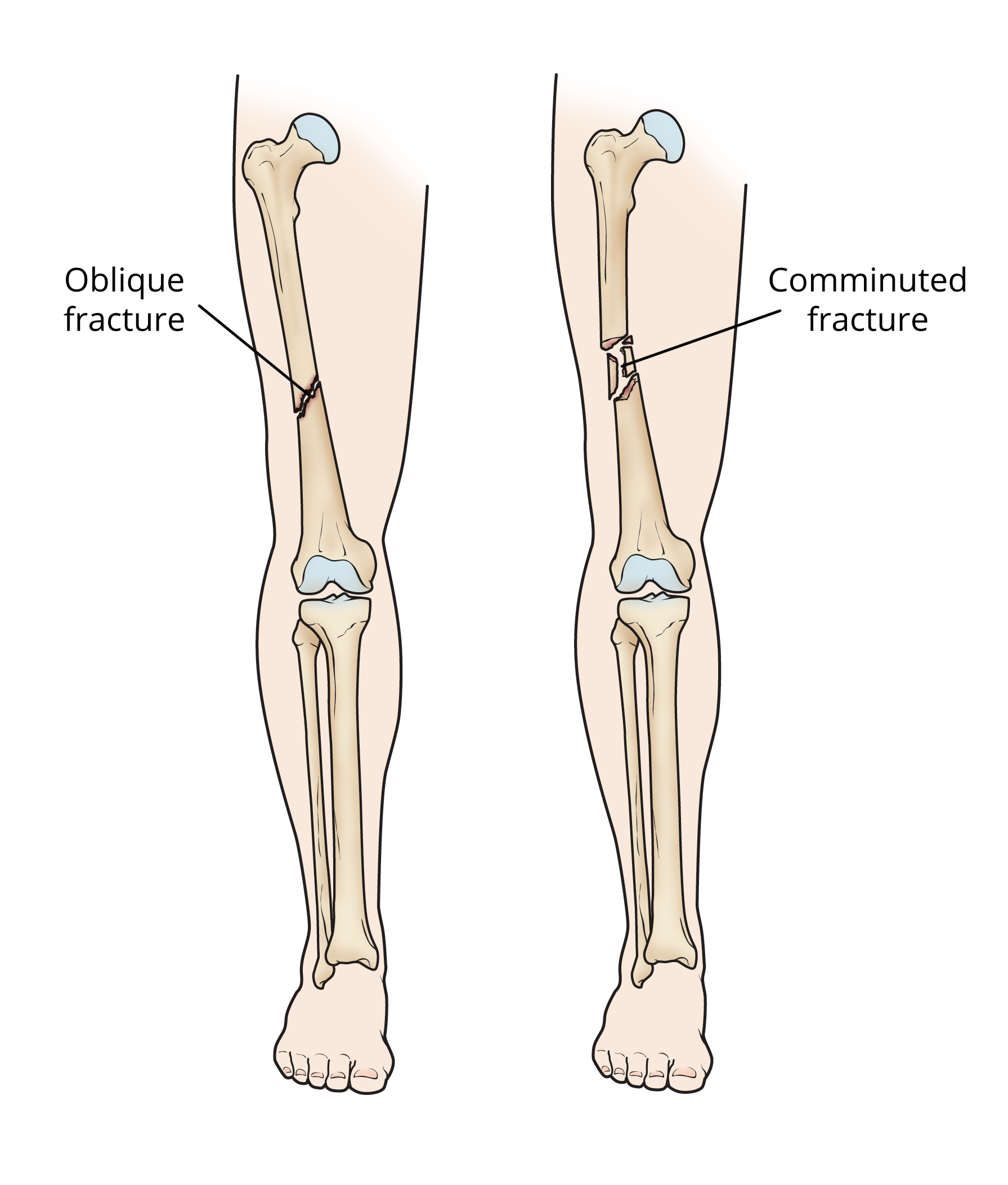
Types of Femur Fractures (Classification)
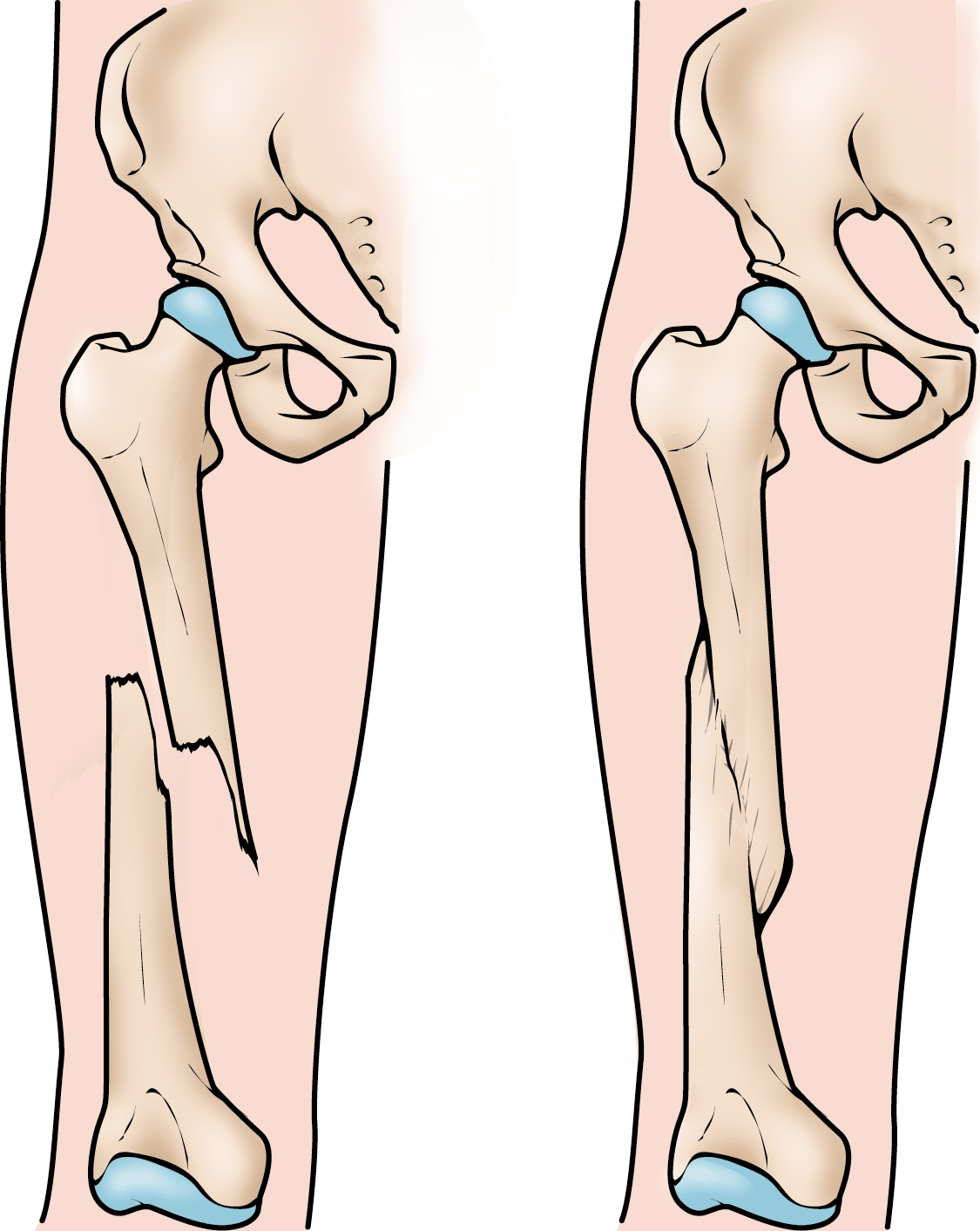
Femur fractures vary greatly. The pieces of bone may be aligned correctly (straight) or out of alignment (displaced), and the fracture may be closed (skin intact) or open (bone piercing through the skin). Open fractures, where the bone is exposed to air, are rare.
Femur fractures are classified depending on:
- Location of fracture on the bone (top, middle, bottom)
- Shape of the fractured ends — bones can break in different directions, such as straight across (transverse), angled (oblique), or spiraled (spiral)
- Whether the edges of the fracture are angled or displaced
- Number of fractured parts — a bone that is broken into three or more pieces is called a comminuted fracture
Symptoms
A femur fracture is a serious injury. It may be obvious that the bone is broken because:
- Your child has severe pain
- The thigh is noticeably swollen or deformed
- Your child is unable to stand or walk, and/or
- Range of motion in your child's hip or knee is limited due to pain.
If you suspect your child has a broken femur, take them to the emergency room right away.
Doctor Examination
It is important that the doctor knows exactly how the injury occurred. Tell the doctor if your child had any disease or other trauma before the injury happened.
The doctor will give your child pain relief medication and carefully examine the leg, including the hip and knee. A child with a femur fracture should always be evaluated for other serious injuries.
Imaging Tests
X-rays. X-rays provide images of dense structures, such as bone. The doctor will order X-rays to see where the bone is broken and what it looks like (see Classification section).
The doctor will also check the X-ray for any damage to the growth area (growth plate) near the end of the femur. This is the part that enables the child's bone to grow. If needed, surgery may help to restore the growth plate's function, and regular X-rays may be taken for many months to track the bone's growth.
Treatment
Treatment depends on many factors, such as your child's age and weight, the type of fracture, how the injury happened, and whether the broken bone pierced the skin (open fracture).
Nonsurgical Treatment
In many femur fractures, the doctor may be able to manipulate the broken bones back into place without an operation (closed reduction).
Bracing and casting. In a baby younger than 6 months , most femur fractures can be treated with a Rhino hip abduction brace or a Pavlik harness. Both of these braces are commonly used to treat infant hip dysplasia. Treatment with the Pavlik harness, however, carries a greater risk of femoral nerve damage (transient femoral nerve palsy), a complication that can cause pain, numbness, and/or weakness in the legs.
Femur fractures in infants aged 7 to 12 months can be treated with a Rhino brace or a spica cast (body cast).
For femur fracture in children between 1 and 5 years old, a spica cast or functional fracture brace can be used. However, in children older than 3 years, surgical fixation may be preferred (see Surgical Treatment below).
There are different types of spica casts, but, in general, a spica cast begins at the chest and extends all the way down the fractured leg. The cast may also extend down the uninjured leg, or stop at the knee or hip. Your child's doctor will decide which type of spica cast is most effective for treating your child's fracture.
When a bone breaks and is displaced, the pieces often overlap and shorten the normal length of the bone. Because children's bones grow quickly, your child's doctor may not need to manipulate the pieces back into perfect alignment. While in the cast, the bones will grow and heal back into a more normal shape.
In general, for the best results, the broken pieces should not overlap more than 2 cm when in the cast. The growth of the femur may be temporarily increased by the trauma. The mild shortening from the overlap will resolve (get better on its own, with time).
Traction. If the shortening of the bones is more than 3 cm or if the bone is too crooked in the cast, it may be helpful to put the leg in traction. Traction uses a gentle, steady pulling action to properly realign the bones.
Surgical Treatment
Doctors generally agree that displaced femur fractures that have shortened more than 3 cm require treatment to correct at least a portion of the shortening.
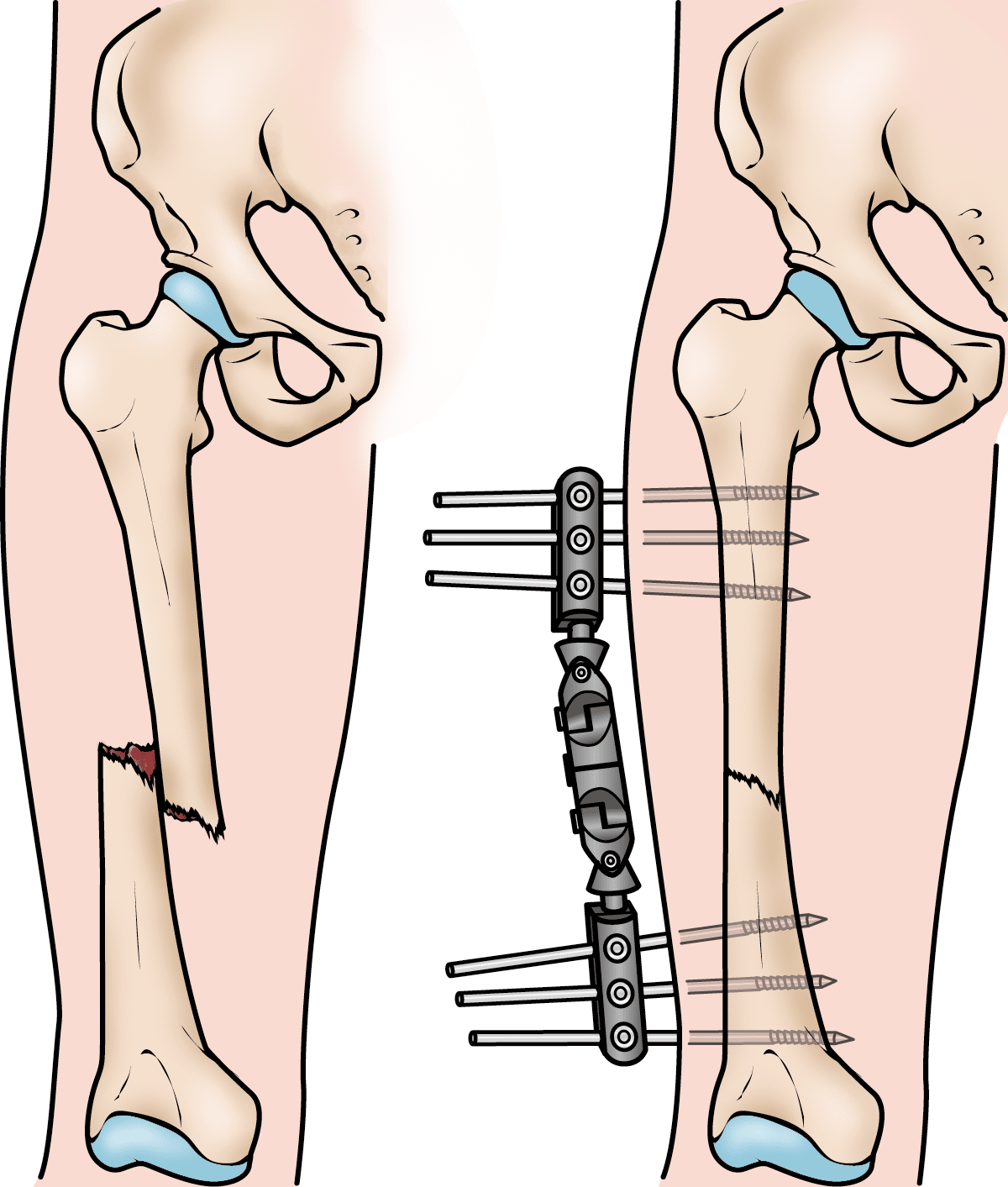
In some more complicated injuries, the doctor may need to surgically realign the bone and use an implant to stabilize the fracture.
Doctors are treating pediatric femur fractures more often with surgery than in previous years due to the benefits that have been recognized. These include:
- Earlier mobilization (walking)
- Faster rehabilitation
- Shorter time spent in the hospital
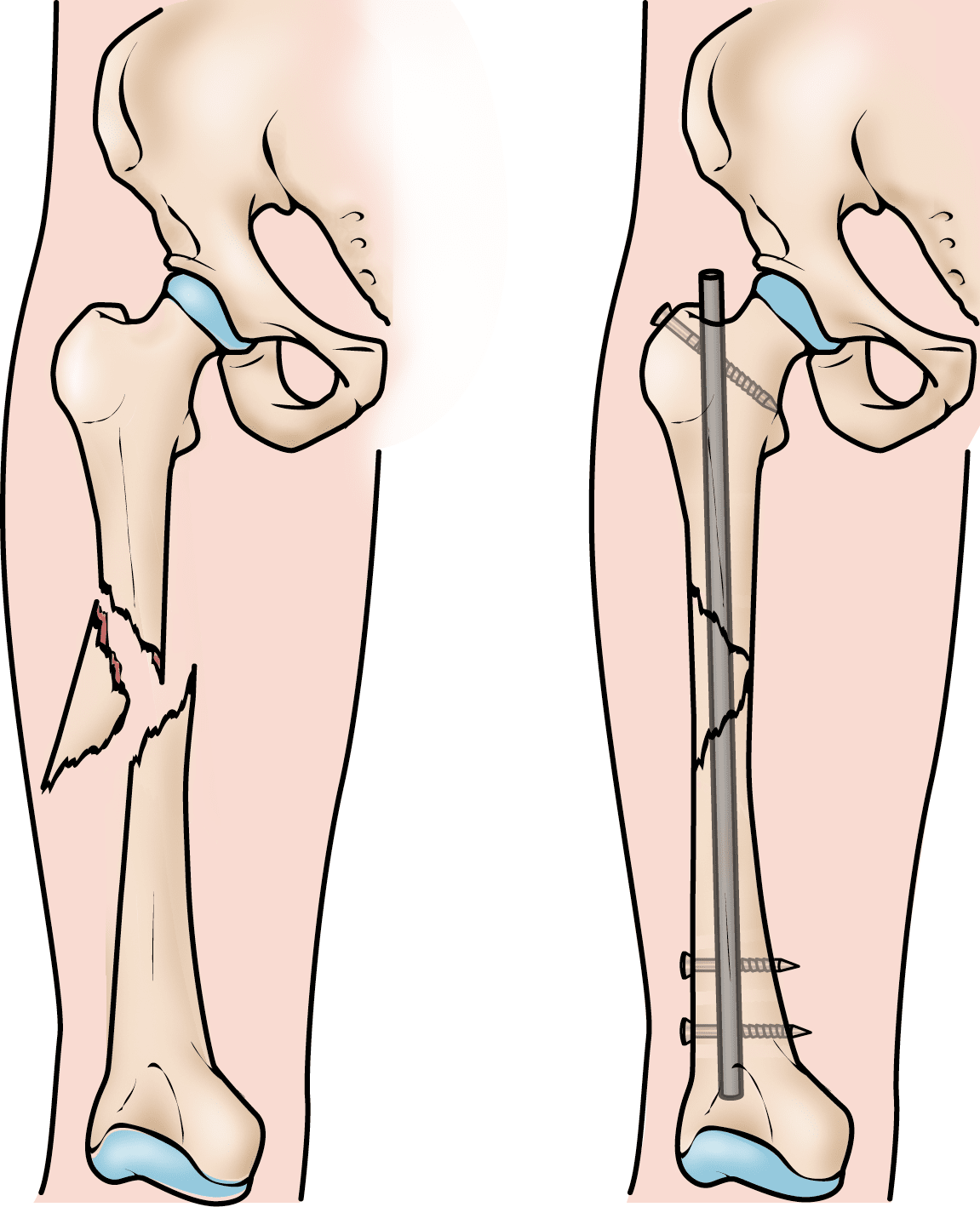
In children ages 6 to 10 years, flexible intramedullary (inside the bone) nails are often used to stabilize the fracture. Over the past 10 to 15 years, this treatment method has gained great acceptance.
Occasionally, the broken bone has too many pieces and cannot be treated successfully with flexible nails. Other options that can lead to successful outcomes in this situation include:
- A plate with screws that "bridges" the fractured segments
- An external fixator (stabilizing frame) — this is often used if there has been a large open injury to the skin and muscles
- Prolonged traction with a pin temporarily placed into the bone
As the child nears the teenage years (11 years to skeletal maturity), the most common treatment choices include either flexible intramedullary nails or a rigid locked intramedullary nail. The rigid nail is particularly useful when the fracture is unstable. Both types of nails allow for the child to begin walking immediately.
Long-Term Outcomes
Generally, children who sustain a femur fracture will heal well, regain normal function, and have legs that are equal in length. The intramedullary nails may need to be removed following healing if they cause irritation of the skin and tissues underneath.
Occasionally, children will require further treatment, either early on or in the future, if:
- There is a significant difference in the length of the legs
- The bone heals at an abnormal angle
- The healed bone is rotated abnormally
- There is an Infection
- The bone fails to heal (nonunion), though this is rare with femur fractures
These problems can nearly always be resolved with further treatment.
To assist doctors in the management of pediatric diaphyseal femur fractures, the American Academy of Orthopaedic Surgeons has conducted research to provide some useful guidelines. These are recommendations only and may not apply to every case. For more information: Plain Language Summary - Clinical Practice Guideline - Diaphyseal Femur Fractures - AAOS
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.