Diseases & Conditions
Growth Plate Fractures
The bones of children and adults share many of the same risks for injury. But because they are still growing, a child's bones are also subject to a unique injury called a growth plate fracture.
Growth plates are areas of cartilage located near the ends of bones. Because they are the last portion of a child's bones to harden, growth plates are particularly vulnerable to injury.
Because the growth plate helps determine the future length and shape of the mature bone, this type of fracture usually requires prompt attention. If not treated properly, it could result in a limb that is crooked or unequal in length when compared to its opposite limb.
Fortunately, serious problems are rare. With proper treatment, most growth plate fractures heal without complications.
Anatomy
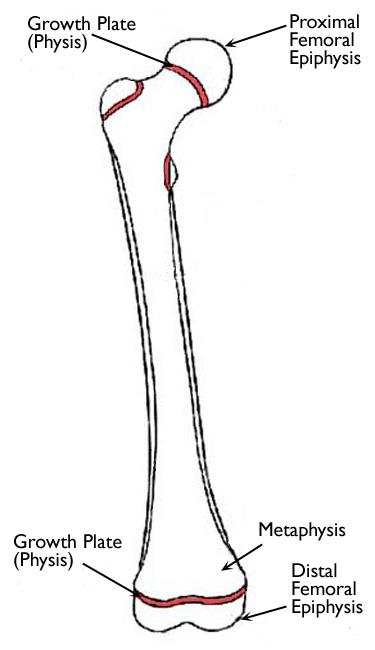
Growth plates are found in the long bones of the body — the bones that are longer than they are wide. Examples of long bones include the femur (thighbone), the radius and ulna in the forearm, as well as the metacarpal bones in the hands.
Most long bones in the body have at least two growth plates, including one at each end. Growth plates are located between the widened part of the shaft of the bone (metaphysis) and the end of the bone (epiphysis).
The long bones of the body do not grow from the center outward. Instead, growth occurs at each end of the bone around the growth plate. When a child is fully grown, the growth plates harden into solid bone.
Description
Most growth plate fractures occur in the long bones of the fingers. They are also common in the outer bone of the forearm (radius) and lower bones of the leg (tibia and fibula).
Growth plate fractures vary greatly in terms of th risk for growth problems. Factors that affect the risk of problems over time include:
- The patient's age
- The bone involved
- Specific fracture pattern
- How much the bone is out of alignment (displaced)
In some areas of the body, such as fingers in younger children, early diagnosis and treatment before healing has set in can sometimes prevent the need for more invasive treatments. Other growth plate fractures, such as those around the knee, are associated with a higher rate of problems and therefore require very careful observation and follow-up.
Classification of Growth Plate Fractures
Several classification systems have been developed that categorize the different types of growth plate fractures. Perhaps the most widely used by doctors is the Salter-Harris system, described below.
Type I Fractures
These fractures break through the bone at the growth plate, separating the bone end from the bone shaft and completely disrupting the growth plate.
Type II Fractures
These fractures break through part of the bone at the growth plate and crack through the bone shaft, as well. This is the most common type of growth plate fracture.
Type III Fractures
These fractures cross through a portion of the growth plate and break off a piece of the bone end. This type of fracture is more common in older children.
Type IV Fractures
These fractures break through the bone shaft, the growth plate, and the end of the bone.
Type V Fractures
These fractures occur due to a crushing injury to the growth plate from a compression force. They are rare fractures.
Cause
Growth plate fractures are often caused by a single event, such as a fall or car accident. They can also occur gradually as a result of repetitive stress on the bone, which may occur when a child overtrains in a sports activity.
All children who are still growing are at risk for growth plate injuries, but there are certain factors that may make them more likely to occur:
- Growth plate fractures occur twice as often in boys as in girls, because girls finish growing earlier than boys.
- Growth plate fractures often occur during participation in competitive sports such as football, basketball, or gymnastics.
- Many growth plate fractures occur during participation in recreational activities such as biking, sledding, skiing, or skateboarding.
- The incidence of growth plate fractures peaks in adolescence.
Symptoms
A growth plate fracture usually causes persistent pain. Other common symptoms include:
- Visible deformity, such as a crooked appearance of the limb
- An inability to move or put pressure on the limb
- A persistent limp
- Swelling, warmth, and tenderness in the area around the end of the bone, near the joint
Doctor Examination
Because a child's bones heal quickly, a potential growth plate injury should be examined by a doctor as quickly as possible. It is important that the bone receives the proper treatment before it begins to heal.
Imaging Tests
- X-rays. Your child's doctor will likely order an X-ray to help determine whether a growth plate fracture has occurred. X-rays provide clear images of dense structures, such as bone.
- Other scans. If greater detail is needed, the doctor may order other tests that can better show the soft tissues, or a cross-sectional view of the injured area. These tests include magnetic resonance imaging (MRI) scans and computed tomography (CT) scans.
Physical Examination
After discussing your child's symptoms and medical history, your child's doctor will perform a careful physical examination of the injured area.
The clinical exam is key for diagnosing growth plate fractures because some non-displaced growth plate fractures cannot be seen on X-rays. This is because they occur through the part of the bone that is made up of cartilage, which is not as dense as bone.
Also, because children’s bones have a different structure and break in different patterns than adult bones, some minor changes on X-rays indicating a growth plate fracture can easily be missed. Conversely, some areas that look like a fracture can be recognized by a pediatric specialist to be a normal development or normal growth plate appearance.
Treatment
Treatment for growth plate fractures depends on several factors, including:
- Which bone is injured
- The type of fracture
- How much the broken ends of the bone are displaced
- The age and health of the child
- Any associated injuries
Nonsurgical Treatment
Many growth plate fractures can heal successfully when treated with immobilization: A cast is applied to the injured area and the child limits some types of activity.
Doctors most often use cast immobilization when the broken fragments of bone are not significantly out of place. A cast will protect the bones and hold them in proper position while they heal.
Occasionally, a week or two later, the bone may have lost its alignment and need to be corrected. Timely follow-up will help your child's doctor discover this early and continue appropriate treatment.
Surgical Treatment
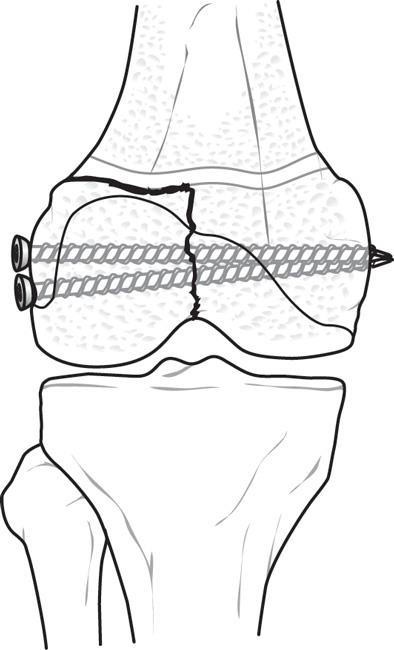
If the bone fragments are displaced and the fracture is unstable, surgery may be necessary. The most common operation used to treat fractures is called open reduction and internal fixation.
During the procedure, the bone fragments are first repositioned into their normal alignment (called a reduction). The bones are then fixed into place with special implants like screws or wires, or by attaching metal plates to the outer surface of the bone.
In some cases, the bone can be made straight by pulling it into place without making any incisions and then securing it with a cast and/or metal pins. These can be removed in the office later once healing has improved.
A cast is often applied after surgery to protect and immobilize the injured area while it heals.
Complications
Although most growth plate fractures heal without any lasting effect, complications can occur.
Rarely, a bony bridge will form across the fracture line, stunting the growth of the bone or causing the bone to curve. If this occurs, your child's doctor may perform a procedure to remove the bony bar and insert fat or other materials to prevent it from reforming. If the problem is diagnosed early, the doctor may be able to take care of it with small surgeries. A long delay in diagnosis — once growth has advanced or is complete, or the bone is very curved — will require a more involved procedure to straighten the bone.
In other cases, a growth plate fracture may actually stimulate growth so that the injured bone ends up longer than its opposite, uninjured limb. If this occurs, surgery can help achieve a more even length.
Recovery
A child's bones heal quickly, but a growth plate fracture can still take several weeks to fully heal. If cast immobilization is used, the length of time the cast is worn will vary depending on the severity of the fracture.
After the bone heals, your child's doctor may recommend specific exercises to strengthen the muscles that support the injured area of bone and improve the joint's range of motion.
Long-Term Outcomes
Growth plate fractures with risks for problems must be treated early and watched carefully to ensure proper long-term results. Regular follow-up visits to the doctor should continue for at least a year after injury to make sure that the growth plate is growing appropriately.
More complicated fractures, as well as fractures to the femur and tibia, may require follow-up visits until the child reaches skeletal maturity.
Continue to Thighbone (Femur) Fractures in Children
Last Reviewed
July 2021
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.