Diseases & Conditions
Osteoporosis
Osteoporosis is a condition in which the bones become thinner, weaker, and more likely to break.
According to the National Center for Health Statistics (part of the Centers for Disease Control and Prevention), in 2017-2018, the prevalence of osteoporosis and low bone mass in adults 50 and older was 55.7%*. That means more than half of all adults 50 and older in the U.S. are either living with or have an increased risk of developing osteoporosis.
People with osteoporosis are more vulnerable to fractures (broken bones) than those without this disorder. The National Osteoporosis Foundation states that about 1 in 2 women and up to 1 in 4 men over the age of 50 will break a bone due to osteoporosis.
Why Osteoporosis Occurs
Your bone changes over time, just like the other tissues in your body. In fact, your body naturally removes old, damaged bone and replaces it with new bone every 7 to 10 years after you become an adult. This process is called bone remodeling.
- Balanced bone remodeling. Before age 30, especially around the time of puberty and early adulthood, people can make bigger, thicker bones with weight-bearing exercise and good nutrition. Until about age 30, your body makes new bone at about the same rate as the old bone tissue is removed; in other words, bone remodeling is balanced.
- Unbalanced bone remodeling. After age 30-40, bone remodeling may gradually become unbalanced. You start to remove old bone more quickly than your body can replace it — leading to a loss of both bone density and architecture, which decreases the strength and quality of your bones as you age.
Osteoporosis is more common in women than in men. This occurs because the loss of estrogen in women at menopause causes rapid bone loss, and women often have smaller, thinner bones than men to begin with. Bone weakness develops later in life in men because their hormone loss occurs gradually with age.
Weakened bone can also occur in both men and women at younger ages due to various causes, including poor nutrition and a sedentary lifestyle.
Osteopenia, or Low Bone Mass
Osteopenia is a condition in which you have low bone mass that is not severe enough to be called osteoporosis by bone density measurements. Osteopenia is now called low bone mass, which occurs because of low peak bone mass and/or bone loss after age 30.
It might be helpful to think of osteopenia as "pre-osteoporosis." If unbalanced bone remodeling continues with aging, it will eventually lead to osteoporosis. Your risk of a fracture is higher than normal with low bone mass, but not as high as with osteoporosis.
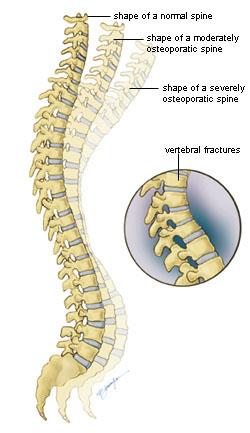
The loss of bone tends to occur the most in the spine, lower forearm above the wrist, and upper femur or thigh — the site of hip fractures. Spine fractures, wrist fractures, and hip fractures are common injuries in older adults.
The first sign that low bone mass has progressed to osteoporosis can be suffering a broken bone from a minor injury that probably would not have caused a fracture in a healthy person.
- For example, if you trip over a rug at home and break your wrist or your hip, this is most likely because of underlying bone weakness. A person with normal bone strength is not likely to break a wrist or hip from this minor trauma.
- Similarly, if you lift bags of groceries or push up a heavy window and sustain a spinal fracture, it’s also likely to be due to osteoporosis.
Recent studies have shown that even fractures caused by greater degrees of injury than simple falls, such as car crashes, can be associated with bone weakness.
Main causes of Osteoporosis
Aging
Most people with osteoporosis are over 50; at this age, bone formation is not keeping up with bone removal.
With aging, the thick outer shell of the bone (cortex) becomes thinner, and the architecture in the spongy bone also becomes thinner and less connected. This causes structural weakness in the bone that leads to fractures.
People who have less dense bones at the end of growth are at more risk of fractures with aging than those who have more dense bones. After age 30, weightbearing exercise can help decrease bone loss and maintain bone mass and strength, but it cannot make denser bones. That is why it's so important to build a maximum peak skeletal density and strength during your growth years.
Hormonal Changes
The levels of certain sex hormones — estrogen in both sexes and testosterone in men — are involved in the process of building and remodeling bones:
- Estrogen levels in women drop quickly at menopause.
- In men, loss of sex hormones occurs more slowly with age, though some men experience testosterone deficiency (hypogonadism) at a younger age.
Sex hormone loss and other aging factors increase the rate of bone turnover, causing more bone to be removed than replaced and leading to progressive bone loss.
Genetic Predisposition
Your risk increases if you have:
- A family history of osteoporosis
- A history of fractures on your mother's side of the family
Additional Risk Factors for Osteoporosis
Certain other factors can increase your risk of osteoporosis independent of your bone density, age, or gender.
Medications
- Corticosteroids, such as prednisone
- Heparin, if taken chronically
- Anti-seizure (epilepsy) drugs
- Thyroid medications, if taken in larger doses than necessary
- Drugs used to treat breast and prostate cancers
- Methotrexate, given for inflammatory arthritis
- Diuretics
- Lithium
- Depo-progesterone, used for birth control
- Antacids that contain aluminum
Health Conditions and Procedures
- Gastrointestinal and digestive disorders, including inflammatory bowel disease and celiac disease
- Prostate or breast cancer
- Chronic kidney disease or liver disease (including biliary cirrhosis)
- Autoimmune disorders, including lupus, rheumatoid arthritis, multiple sclerosis, and ankylosing spondylitis
- Hematologic disorders, including leukemia, lymphoma, multiple myeloma, and sickle cell disease
- Neurological disorders, including stroke, spinal cord injury, and Parkinson's disease
- Endocrine disorders, such as hyperparathyroidism or hyperthyroidism, diabetes, Cushing's syndrome, or premature menopause
- Certain surgical procedures, including gastrointestinal bypass, gastrectomy, and organ transplantation
Learn more about health conditions and medications that can have a negative impact on bone health.
Poor Nutrition
- Low intake of calcium
- Vitamin D deficiency
- Low intake of dietary protein
- Significant weight loss, an eating disorder, or relative energy deficiency in sports (RED-S) during peak bone-building years. RED-S is a syndrome that happens when an athlete does not consume enough calories to properly fuel their bodies.
Lifestyle Choices
- Excessive use of alcohol. Women should consume no more than 1 daily alcoholic beverage; men should have no more than 2 drinks per day.
- Smoking. Nicotine acts directly on bone-forming cells to decrease the amount of bone formed. It also causes your body to lose bone even more quickly than normal by affecting hormone metabolism. Learn more: Smoking and Musculoskeletal Health.
- Lack of physical activity, both in childhood and adulthood. You should aim for at least 150 minutes per week of moderate physical activity, including weightbearing exercises that help build or maintain bone. Learn more: Exercise and Bone Health
Doctor Examination
At a routine health checkup, your doctor might look for signs of osteoporosis, such as significant height loss with age. This is especially important if you have a family history of osteoporosis, have any medical diagnoses that increase fracture risk, or are taking medications that can lead to bone loss.
At your appointment, your doctor will examine you and take a complete medical history. This means reviewing:
- Your past health
- Your family members' health
- All of your medications and supplements
- Recent falls
- Any problems or concerns you have now, including balance issues or a history of fractures
If you sustain a fracture after age 40, not only should you receive treatment for the fracture itself, you should also notify your family physician so you can be seen and evaluated for future fracture risk.
Tests
If your doctor believes you might have low bone mass/osteoporosis, you will probably have further testing. The doctor wants to learn if you do have low bone mass and how severe the problem is. Testing, which may also detect treatable cause of excessive bone loss, typically includes:
- Blood and urine tests
- Specialized X-ray testing called bone densitometry testing, or DXA. A DXA scan is the main way doctors look for low bone mass because this test can find low bone mass before a fracture occurs. The test is safe (with less radiation than you get from a regular chest X-ray), accurate, and painless. If you have low bone mass or osteoporosis, your doctor will usually follow DXA scans every 2 or 3 years to recheck your bones as you age.
T score
Your DXA scan gives your doctor a result called a T score. Your T score is the main measurement of your bone density, indicating how your bone density compares to that of a healthy 30-year-old.
This is what different T scores mean:
- If your T score is -1 to +1, you have normal bone density
- If your T score is -1 to -2.4, you have osteopenia, now called low bone mass
- If your T score is -2.5 or lower, you have osteoporosis
Prevention and Treatment
Bone loss and fractures don't have to be an inevitable part of aging. Based on your test results and medical history, your doctor will work with you to develop a treatment plan to protect and improve your bone and prevent falls that may lead to fractures.
Prevention and treatment for osteoporosis will probably include one or more of the following:
- Changing your diet
- Taking supplements — especially calcium and vitamin D
- Making lifestyle modifications, such as developing a sustainable exercise plan, quitting smoking if you smoke, and limiting alcohol consumption
- Taking medications to lower your risk of fractures by increasing bone density, preventing bone loss, or building new bone
- Preventing falls, including addressing fall risks in your home, and doing exercises to improve your balance. Learn more about how to prevent falls.
- Preventing or controlling diabetes
- Preventing or controlling high blood pressure
- Lowering disease risk, including the risk of breast and prostate cancer, multiple sclerosis, rheumatoid arthritis, and osteoarthritis
- Starting estrogen replacement therapy if you are less than 10 years postmenopausal; menopausal hormone therapy has been shown to reduce the risk of fragility fractures
Learn more: Osteoporosis Prevention and Treatment
*NCHS Data Brief No. 405, March 2021; PDF Versionpdf iconpdf icon
Contributed and/or Updated by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.