Diseases & Conditions
Neurofibromatosis
Neurofibromatosis is a disease that affects the development and growth of nerve cell tissues. It causes tumors to grow on nerves and can affect many systems in the body including the skin, skeleton, and brain. The tumors, called neurofibromas, are usually benign (noncancerous) and grow on nerves within the body, as well as on and under the skin. It is caused by genetic mutations.
Neurofibromatosis can cause skin changes, bone deformities, and other problems. Often, symptoms are present at birth or develop during childhood. Some people have symptoms that are mild or not noticeable at all. In other people, neurofibromatosis causes significant disability. In many cases, neurofibromatosis symptoms worsen as a patient ages.
There is no cure for neurofibromatosis. However, many symptoms can be treated and managed. Children with more severe symptoms will naturally require more medical attention than children who have mild symptoms.
Types of Neurofibromatosis
Neurofibromatosis Type 1 (NF1)
Neurofibromatosis Type 1 is the most common form of the disease, occurring in 1 in 3,000 to 4,000 births. this article will primarily discuss NF1.
Also known as von Recklinghausen disease, NF1 mostly affects nerves of the outer parts of the body (peripheral nervous system).
Symptoms begin at birth or early in life. People with NF1 may develop:
- Multiple birth marks. Six or more light brown-colored birthmarks (cafe-au-lait spots) may be located anywhere on the body. The spots usually appear before about 9 years of age. They take various shapes and measure about 5mm or more in size in young children and about 15mm or more in adolescents.
Other skin abnormalities in NF1 include freckling in the armpit and groin areas (called axillary and inguinal freckling).
- Multiple neurofibromas. These tumors are usually small, painless, and slow growing. They may form nodules on the skin or masses deep in the body. Tumors may appear at any age, but they often first occur around adolescence.
Tumors caused by NF1 sometimes affect the brain or spinal cord. They may grow on nerves of the eye (optic glioma) and in rare instances may interfere with vision.
Sometimes a tumor involves multiple nerves and grows to a very large size (called a plexiform neurofibroma). This is especially true on the face, arms, or legs. This type of tumor may become disfiguring, painful, or life-threatening, and it can cause weakness in the arms or legs.
Most NF1 tumors are benign; however, a small number become cancerous.
- Lisch nodules in the eyes. Lisch nodules are small brown tumors that often appear on the colored part of the eye (iris) in people with NF1. Lisch nodules cause no medical problems and may appear at around 6 to 10 years of age.
- Other complications. Learning disabilities affect many children with NF1. A child may be delayed in learning to walk or talk. Some children also have:
- Mental retardation and/or speech problems
- Short stature
- An oversized head (macrocephaly)
- Hypertension
- An increased risk of cancer (malignancy)
In addition, NF1 can cause orthopaedic problems, including bone abnormalities. The most common orthopaedic problems in children with NF1 include:
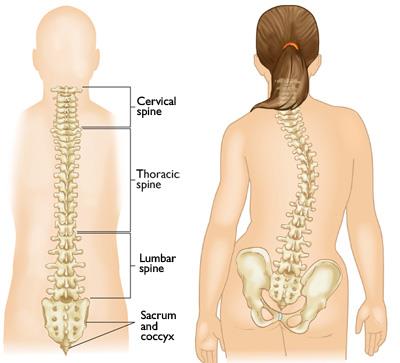
- Scoliosis. Scoliosis is a sideways curve of the spine. Instead of a straight line down the middle of the back, a spine with scoliosis curves, sometimes looking like a letter S or C.
Scoliosis in children with NF1 can range from mild to severe curves. In many cases, the spinal curves progress slowly, at a similar rate as curves seen in children with idiopathic scoliosis. This type of scoliosis in children with NF1 is called nondystrophic. However, a change in severity can occur, resulting in dystrophic changes.
The less common form of scoliosis that affects children with NF1 is dystrophic scoliosis. The curve pattern in this type of scoliosis is short and shapr with associated kyphosis (rounding of the back). There is also thinning of the ribs, as well as abnormal formation of the vertebrae because of nerve root tumors or enlargement of the dural sac within the vertebral canal. These curves can worsen rapidly and can lead to serious deformity.
In addition, children with NF1 may have kyphosis as their main spinal deformity.
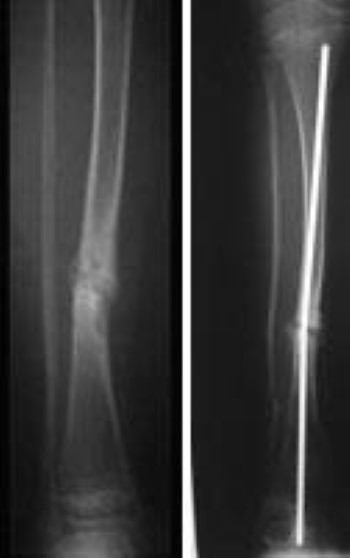
- Congenital pseudarthrosis of the tibia. Neurofibromatosis Type 1 can cause bones to grow abnormally. The tibia (shinbone) is the bone most commonly affected. In a small number of children with NF1, bowing of the tibia is one of the first signs of the disease, most often occurring before a child is 2 years old.
The tibia typically bows toward the front and to the outside of the leg (called an anterolateral bow). If the child has no other symptoms and has not yet been diagnosed with NF1, tibial bowing should prompt the pediatrician to fully evaluate the child for the disease. Although anterolateral bowing of the tibia may occur in patients without neurofibromatosis, it is associated with the disease 50% of the time (though only about 10% of NF1 patients develop this problem).
The bowing of the tibia makes it more vulnerable to a break, or fracture. Often, this fracture does not heal well due to the deformity of the bone, and may lead to a persistence of the fracture, known as a pseudarthrosis. Prevention of this sort of break is very important, as a pseudarthrosis of the tibia is very difficult to treat and requires surgery.
Neurofibromatosis Type 2 (NF2)
Neurofibromatosis Type 2 is less common, occurring in 1 in 25,000 to 40,000 births. Also known as bilateral acoustic neurofibromatosis (acoustic neuroma), NF2 mostly affects the central nervous system, causing tumors of the brain and spinal cord.
Hearing loss that begins in the teens or early 20s is often the first symptom of NF2. People with NF2 may develop:
- Auditory nerve tumors. Most people affected by NF2 develop tumors on the nerves needed for hearing (auditory nerves). Although the tumors are usually benign (noncancerous), they often lead to progressive hearing loss as they grow.
- Other complications. Affected people may also have ringing in the ear(s), headaches, facial pain/numbness, and trouble with their balance.
Schwannomatosis
Schwannomatosis is the rarest form of neurofibromatosis and does not affect the musculoskeletal system. It can be caused by mutations in the SMARCB or LZTR1 genes.
Cause
NF1 and NF2 are genetic disorders. A separate abnormal gene causes each form of the disease.
NF1 is caused by mutations (changes) in the NF1 gene, which provides instructions for the body to make a protein called neurofibromin.
- About 50% of the time, NF1 is an inherited disease, passed down from a parent by what's called autosomal dominant inheritance. The severity of the inherited disease can vary from generation to generation (variable penetrance).
- The other half of NF1 cases are caused by spontaneous (not inherited) mutations.
NF2 is caused by a mutation in the NF2 gene, a tumor suppressor gene. This mutation makes affected people more susceptible to benign and cancerous tumors. Roughly 50% of affected people inherit the abnormal gene; in the other half, the mutation is spontaneous (not inherited).
Doctor Examination
Medical History and Physical Examination
Before a physical examination, the doctor will talk with you about your or your child's general health and current condition. The doctor will want to know which symptoms are present and when they began.
During the physical examination, the doctor will look for changes in skin appearance and the presence of tumors or bone abnormalities. Because neurofibromatosis is often inherited, the doctor may also want to examine close family members (parents, siblings, and children) to look for signs of neurofibromatosis.
Tests
Imaging and laboratory tests can help the doctor diagnose neurofibromatosis, as well as determine a treatment plan.
- X-rays. X-rays create clear pictures of dense structures, like bone. The doctor may order X-rays to look for skeletal deformities.
- Magnetic resonance imaging (MRI) scans. MRI scans create better pictures of soft structures than X-rays. The doctor may use MRI to find soft tissue tumors when they are still small. Tumors along the nerves of the eyes and ears may be easier to treat when discovered early.
- Biopsy. In a biopsy, a tissue sample of the tumor is taken and examined under a microscope. This test is used to check for cancer cells.
General Treatment
Because there is no cure for neurofibromatosis, treatment focuses on managing the symptoms and preventing complications. Many types of medical specialists may be involved in the treatment of neurofibromatosis, depending on the patient's symptoms. A team approach with knowledgeable caregivers and involved patients and families should help to optimize care.
General Guidelines for Treatment
- Children with neurofibromatosis often need regular medical evaluations to measure growth and blood pressure, and to examine skin, bones, the nervous system, vision, and hearing.
- Sometimes, young children with abnormal spots have not yet developed neurofibromas. If this is the case, regular eye examinations and screening tools may help detect optic nerve gliomas for treatment before a child starts to lose their eyesight.
- Adults with neurofibromatosis often need yearly evaluations of the nervous system and hearing.
- Some people with neurofibromatosis have ongoing medical issues, such as pain and disability. They may need lifelong care from several medical and surgical specialists (i.e., orthopaedic surgeons, neurologists, dermatologists, and radiologists).
- Some people with neurofibromatosis visit multidisciplinary (many different doctors) neurofibromatosis clinics for comprehensive evaluations and management plans. They may receive treatment at the clinic or take a management plan back to their own doctor.
Treatment of Tumors
Most tumors caused by neurofibromatosis do not need treatment. However, you or your child may need treatment for tumors that are:
- Painful
- Disfiguring
- Rapidly growing
- Impairing the function of or compressing other body parts
Some neurofibromas grow fast and may be at risk for becoming cancerous.
The following are some of the treatment options available for abnormal tissue growth.
Surgery. The doctor may remove a tumor by cutting it out of the body.
Radiation. Beams of energy (radiation) can shrink tumors and destroy cancer cells.
Chemotherapy. Chemotherapy is a drug treatment used to kill a tumor and any spread of cancer. It is often used initially to shrink a tumor and make it easier to remove with surgery.
Treatment for Orthopaedic Problems
The majority of people with NF1 will experience only moderate symptoms throughout their lives. Only a small percentage of NF1 patients will have orthopaedic problems that require treatment.
Scoliosis Treatment
Scoliosis associated with neurofibromatosis may require more intensive treatment than scoliosis that is not associated with the disease.
Bracing. If your child has a curve of 15° to 25° and is still growing, your child's doctor may recommend wearing a brace. Although bracing will not straighten scoliosis curves, it may slow the progress of the curves or prevent them from getting worse. Brace treatment may be more appropriate for the non-dystrophic type of scoliosis.
Spinal fusion. To treat severe scoliosis caused by NF1, the doctor may recommend surgery.
The operation for scoliosis is a spinal fusion. This is essentially a welding process. The basic idea is to realign and fuse together the curved vertebrae so that they heal into a single, solid bone. Implants made up of screws, rods, hooks, or wires will keep the bones in place while the fusion heals.
Treatment for Pseudarthrosis of the Tibia
Children with NF1 who have tibial bowing require special braces that are intended to protect the bone from fracture. If the bone breaks, surgery is frequently required.
During the operation, the bone fragments are first repositioned (reduced) into the best alignment possible, then held together with special implants.
These fractures, often delayed in their healing and referred to as pseudarthroses, are difficult to treat, and the surgeon may need to apply special bone grafts to stimulate healing. Refracture is common. If the bone does not heal despite several surgical interventions, the surgeon, patient, and patient's family may need to consider amputation.
Newer techniques now available utilize implants that allow for growth, better support, and extensive bone grafting, which can enhance healing.
Living with Neurofibromatosis
Some people with neurofibromatosis and other genetic disorders may experience emotional or psychological issues as a result of their illness. They may become isolated and withdrawn because they feel different from others. They may have emotional and/or social pain related to their appearance. They may experience fear of the complications and they may even wonder whether to have children.
Many parents of children diagnosed with neurofibromatosis may also be suffering feelings of shock, anger, sadness, confusion, guilt, and/or anxiety.
Family counseling, genetic counseling, and support groups may help people with neurofibromatosis and their families by offering support, answering questions, and helping with plans for the future.
Sources:
NORD https://rarediseases.org/rare-diseases/neurofibromatosis-type-1-nf1/
Neurofibromatosis Fact Sheet. The National Institute of Neurological Disorders and Stroke (2021).
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.