Diseases & Conditions
Hip Fractures
A hip fracture is a break in the upper portion of the femur (thighbone). Most hip fractures occur in elderly patients whose bones have become weakened by osteoporosis. When a hip fracture occurs in a younger patient, it is typically the result of a high-energy event, such as a fall from a height or motor vehicle/motorcycle collision.
Each year, more than 300,000 people in the U.S. sustain a hip fracture. Most of these fractures occur in adults 65 or older who are injured in household or community falls.
Hip fractures can be very painful. Treating the fracture and getting the patient out of bed as soon as possible will help prevent medical complications such as bed sores, blood clots, and pneumonia. In very old patients, prolonged bed rest can also lead to disorientation, which makes rehabilitation and recovery much more difficult. For these reasons, prompt surgical treatment is recommended.
Anatomy
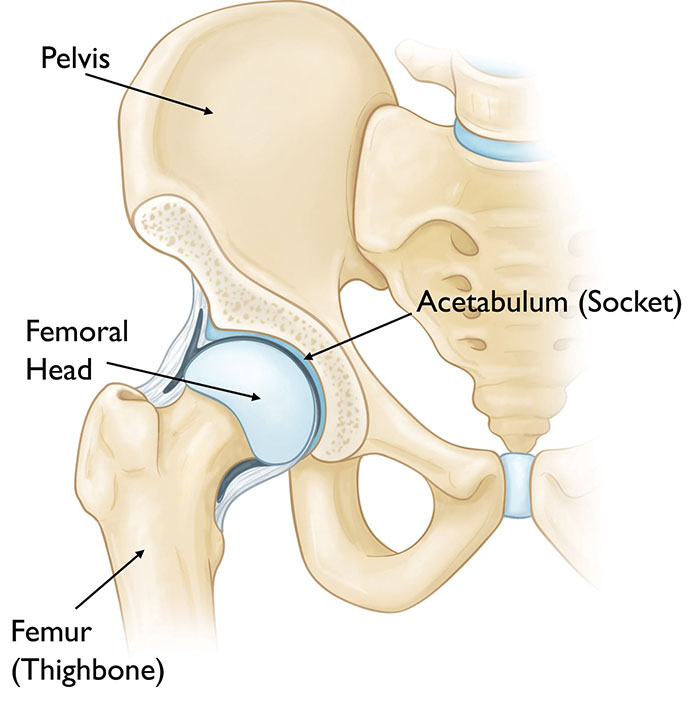
The hip is a ball-and-socket joint.
- The ball is the head of the femur, which is the upper part of the thighbone.
- The socket is called the acetabulum. The acetabulum is part of the pelvis bone. It has a rounded shape that fits around the femoral head.
Fractures of the acetabulum and pelvis are addressed in separate articles. Read more: Acetabular Fractures and Pelvic Fractures.
Description
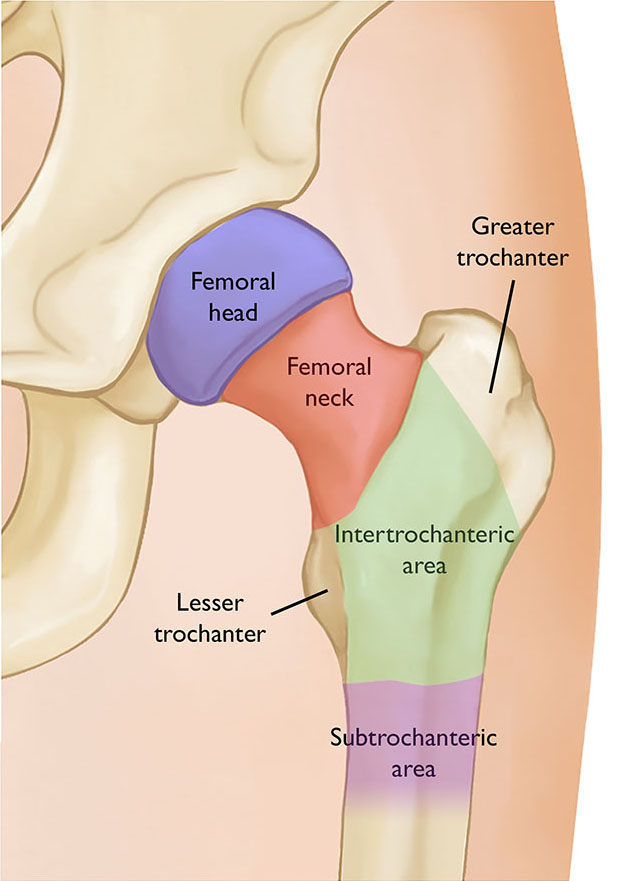
A hip fracture can cause injury to one of four areas of the upper femur:
- Femoral head. The ball of the femur that sits in the socket.
- Femoral neck. The area of the femur below the ball (femoral head).
- Intertrochanteric area. The area below the neck of the femur and above the long part, or shaft, of the femur. It is called intertrochanteric because it is marked by two bony landmarks: the greater trochanter and the lesser trochanter.
- Subtrochanteric area. The upper part of the shaft of the femur below the greater and lesser trochanters.
Intertrochanteric and femoral neck fractures are the most common types of hip fracture. Femoral head fractures are extremely rare and are usually the result of a high-energy event.
Cause
Most hip fractures result from low-energy falls in elderly people who have weakened or osteoporotic bone. In these people, even a simple twisting or tripping injury may lead to a fracture.
In some cases, the bone may be so weak that the fracture occurs spontaneously while someone is walking or standing. When this happens, it is often said that “the break occurs before the fall.” Spontaneous fractures usually occur in the femoral neck.
Stress fractures or fractures from repeated impact may also occur in the femoral neck. These fractures are often seen in distance runners, including military recruits in basic training. When stress fractures occur in the subtrochanteric region of the hip, they are usually associated with long-time use of certain osteoporosis medications.
Fractures of the femoral head are rare and are usually the result of a high-impact injury or are part of a fracture dislocation of the hip.
Symptoms
- Typically, a hip fracture is acutely painful. The pain is usually limited to the groin and the upper part of the thigh.
- With most hip fractures, you will not be able to stand, bear weight, or move the upper part of your leg (above knee).
- You will be able to move your ankle and toes unless there is an injury to your lower leg in addition to your hip.
- Often, the injured leg will appear shorter than the opposite leg and will be twisted or rotated.
- There may be a bruise on the outer part of the hip or thigh at the point of impact where you fell, and all movement will be limited and painful.
- With some fractures, it may be possible to bear part of your weight on the leg — but it will be severely painful.
- A small number of hip fractures may not be as painful at first. Typically, these are nondisplaced fractures of the femoral neck. In a nondisplaced fracture, the bone breaks, but the pieces of bone stay properly aligned. In this situation, you may choose to go to a doctor's office rather than an emergency room. With this type of fracture, you may still be able to move your leg and bear weight even though it is painful.
- Stress fractures may cause increasing pain over time (vs. more immediate pain caused by a traumatic injury).
Doctor Examination
Physical Examination
Most of the time, a patient with a hip fracture will be taken by ambulance to a hospital emergency room.
At the hospital, you will be examined by either an emergency room physician or an orthopaedic surgeon. They will take a history of your injury and check to make sure you do not have injuries to other parts of your body. The doctor will also check the sensation, movement, and circulation in your lower leg.
Imaging Tests
Imaging tests will help confirm the diagnosis and provide more information about the fracture.
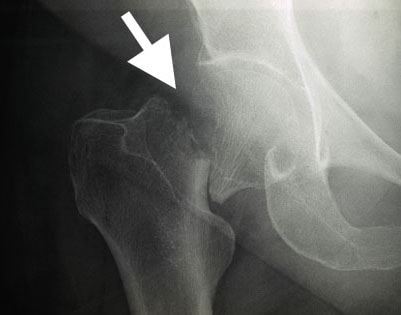
X-rays. X-rays provided images of dense structures, such as bone. Most hip fractures can be diagnosed with an X-ray.
Computerized tomography (CT) scans. A CT scan will provide a detailed cross-sectional image of your hip. Your doctor may order a CT scan if X-rays do not show a fracture or to learn more about your fracture to aid in surgical planning.
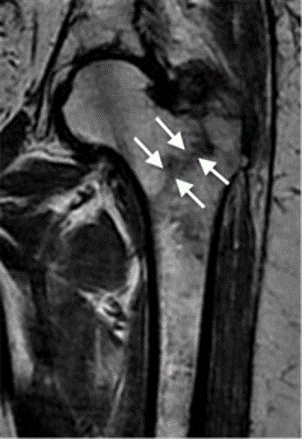
Magnetic resonance imaging (MRI) scans. MRI scans are rarely needed. An MRI scan provides detailed images of both soft tissues and bone. Because it is very sensitive, an MRI can sometimes detect a small or incomplete fracture that cannot be seen on an X-ray. MRI is more commonly ordered if both X-rays and CT scans are negative and if your doctor suspects a stress fracture.
Treatment
Most hip fractures require surgical treatment. Only a very small group of nondisplaced fractures in healthy patients can be treated without surgery, while a separate small group of patients may be too sick to safely have surgery.
Surgical treatment is required to relieve the acute pain of the fracture and to allow the patient to get out of bed. Having surgery as soon as possible, within 24 to 48 hours (1 to 2 days) may reduce the risk of complications.
- If you are admitted to the hospital with a hip fracture, you will have preoperative testing and will most likely be seen by an internist. They will make sure that you are medically ready to have surgery.
- In some cases, you may need to be seen by a specialist, such as a heart doctor (cardiologist) or lung doctor (pulmonologist), to treat specific medical problems.
- If you have been on a blood thinner, you may need to wait for your clotting times to improve before you go to the operating room.
This process of getting a patient medically ready for surgery is called optimization. Ideally, it should be done within 48 hours, but sometimes it may take longer. Even if it does takes longer, it is better to be optimized than to rush to surgery.
Treatment for a hip fracture depends on the type and location of the fracture, as well as the age and condition of the patient.
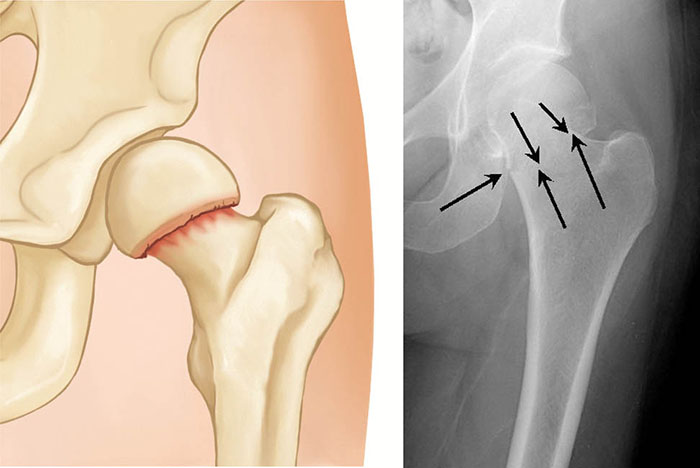
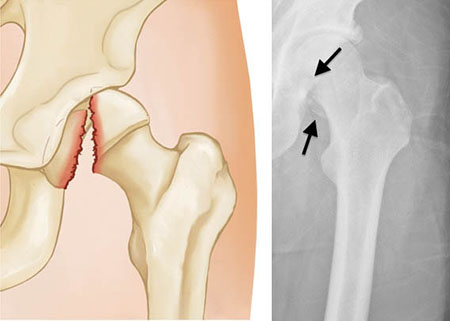
Femoral Neck Fracture
This type of fracture is also sometimes called a subcapital or intracapsular fracture.
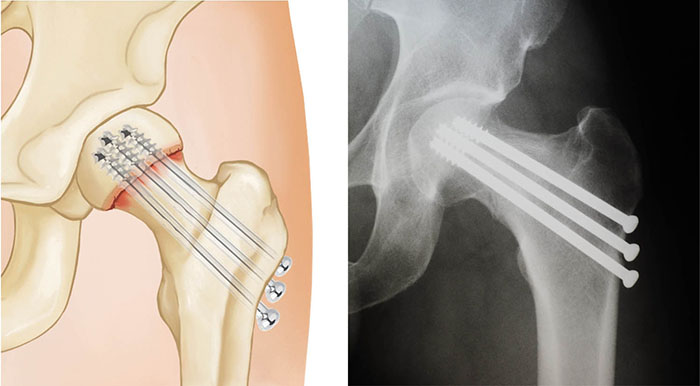
If a femoral neck fracture is not displaced (meaning the pieces of bone are properly aligned), the most common treatment is in-situ fixation.
In this procedure, surgical pins/screws or a plate and screw device are passed across the fracture site to hold the ball of the femur in place while the fracture heals. This procedure prevents the femoral head from dislodging or slipping off of the femoral neck, a situation that would require partial or total hip replacement. Both options provide stability to allow for immediate mobilization (getting out of bed and moving around)
A small number of femoral neck fractures may be treated without surgery. These are typically nondisplaced fractures in younger, healthy patients. Because there is a risk of displacement, these patients need to be monitored carefully. Non-operative treatment consists of limited or protected weightbearing with crutches for several weeks.
Patients who did not walk before surgery or have severe medical problems may also be considered for nonsurgical treatment.
Displaced fractures of the femoral neck present a more difficult problem than nondisplaced fractures. The blood supply to the head of the femur comes through a structure called the posterior capsule. The posterior capsule is often injured with a displaced femoral neck fracture, so the fracture has less chance of healing.
Even if the fracture does heal, a condition called avascular necrosis may develop in the head of the femur. This causes damage to the bone cells, collapse of part of the femoral head, and subsequent arthritis.
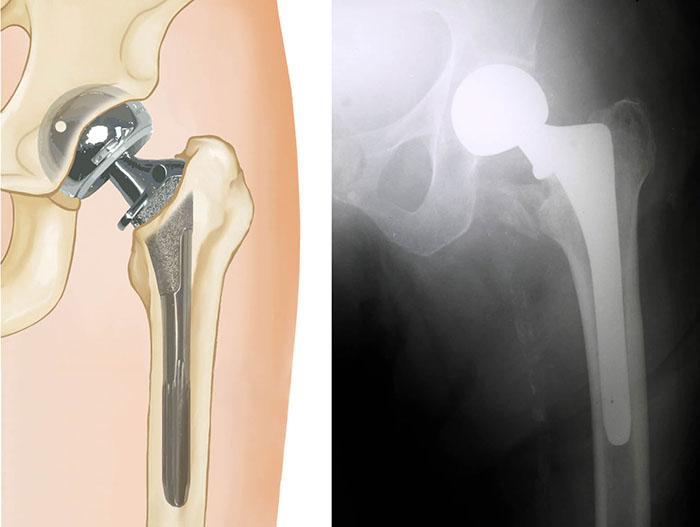
For this reason, displaced fractures of the femoral neck are often treated with hip replacement.
- For elderly patients, a hemi-arthroplasty, or partial hip replacement, is typically the treatment of choice.
- In properly selected patients, there may be a benefit to total hip replacement (at the risk of increasing complications). Total hip replacement may also be considered in younger, more active patients.
In some younger patients, it is desirable to preserve the natural femoral head rather than do a replacement. In these patients an open reduction is performed. This involves making an incision over the hip joint, putting the bone back into place, and then holding the bone with pins, screws, or another type of metal fixation.
While this procedure does carry the risks of avascular necrosis and failure to heal (nonunion), it is generally agreed that the goal is to preserve a younger person’s normal hip.
Your orthopedic surgeon will review the treatment options with you and your family.
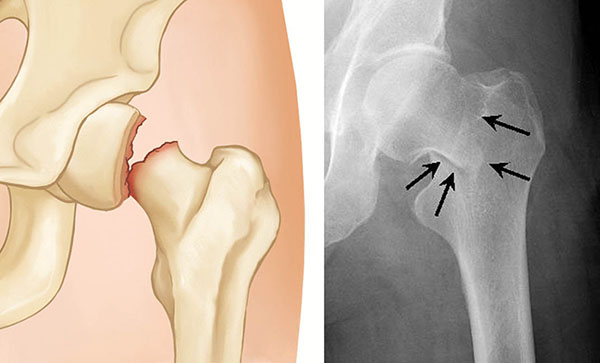
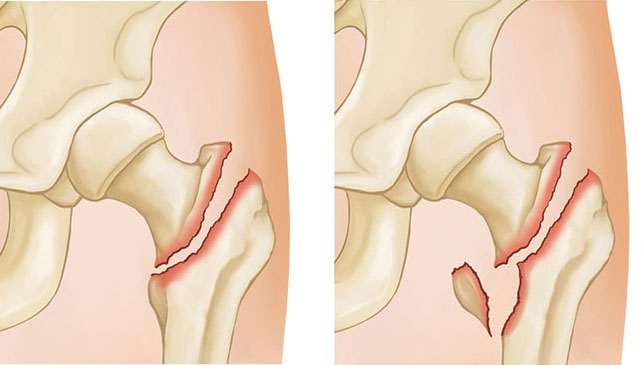
Intertrochanteric Fracture
Intertrochanteric fractures occur below the femoral neck in a broader region between the greater and lesser trochanters. The greater trochanter is the bump you feel on the side of your hip. There may be two, three, or even more fracture fragments.
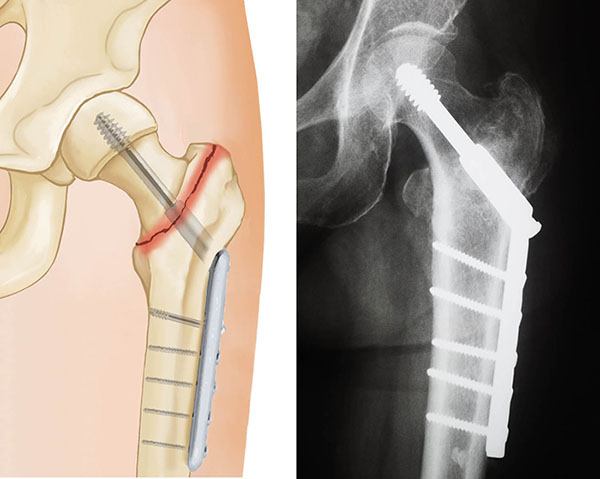
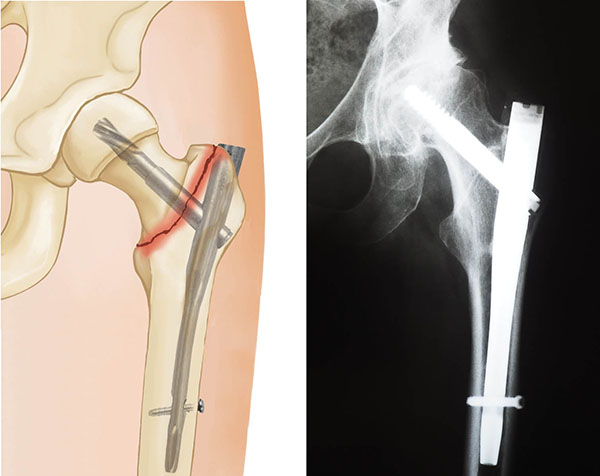
Intertrochanteric fractures are treated surgically with either a sliding compression hip screw and side plate or an intramedullary nail.
The compression hip screw is fixed to the outer side of the bone with bone screws. A large secondary screw (lag screw) is placed through the plate into the femoral head and neck. This design allows for compression at the fracture site, increasing stability and promoting healing.
The intramedullary nail is placed directly into the marrow canal of the bone through an opening made at the top of the greater trochanter. One or multiple screws are then placed through the nail and into the femoral head. An additional screw is placed into the bone to control rotation.
Fracture of the Greater Trochanter
Isolated fractures of the greater trochanter usually come from a low-energy household fall. While they are often painful, they usually heal without surgery. These fractures are stable and can be treated with protected weightbearing using either crutches or a walker.
If an X-ray shows an isolated fracture of the greater trochanter, it is often helpful to get a CT scan to make sure that the fracture does not extend to the intertrochanteric area.
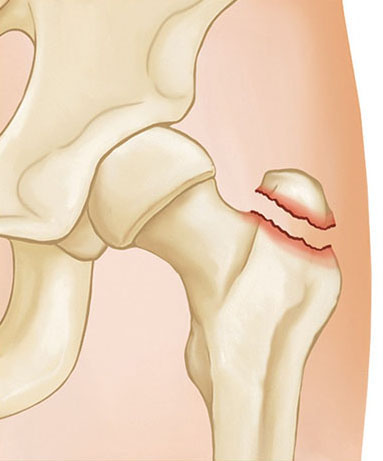
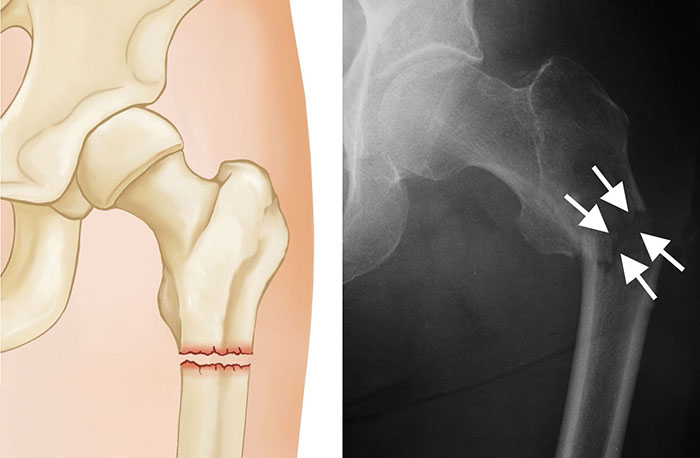
Subtrochanteric Fracture
Subtrochanteric fractures involve the upper part of the shaft of the femur, just below the hip joint.
They are treated surgically with an intramedullary nail into the shaft of the femur and a screw placed through the nail into the femoral head.
To keep the bones from rotating around the nail or from shortening (telescoping) on the nail, additional screws may be placed at the lower end of the nail near the knee. These are called interlocking screws.
In some cases, your surgeon may choose to use a compression screw with a long side plate instead of a nail.
Femoral Head Fracture
Femoral head fractures are rare; they account for less than 1% of all hip fractures. They usually result from a high-velocity event. Sometimes there may be an associated fracture of the hip joint socket.
- If the fracture is not displaced, it may be treated nonsurgically with limited weightbearing.
- If there is a small displaced fragment that does not involve a large part of the joint surface, the fragment may be simply removed.
- If there is a large fragment in a young active person, open reduction and fixation with screws is often done.
- In an older person, the treatment of choice is hip replacement — either partial or total — to replace the damaged femoral head.
Recovery
Most patients are able to get of bed and start physical therapy the day after surgery. It is important to begin moving as soon as possible. This helps prevent medical complications, such as blood clots, pneumonia, and bed sores. For older patients, it also helps prevent disorientation and deconditioning (harmful effects on the body caused by long periods of inactivity).
Hip fractures in the elderly may cause disability and lack of independence. Early movement and rehabilitation have been shown to improve long-term results.
During recovery, you will work with physical and occupational therapists. They will give you exercises and tell you how much weight you can put on your leg. They will also show you how to manage the activities of daily living, such as bathing and dressing.
Medical Care
If you take medications for a problem such as heart disease, an internist or hospitalist will most likely assist in your care. They will address any medical problems and prescribe the appropriate treatment.
You will be given antibiotics to prevent infection for 24 hours after surgery.
You will also be placed on a blood thinner to help prevent blood clots. The medication may be given as either pills or injections. Your doctor will determine the length of time you need to be on blood thinners. Compression boots may be placed on your legs while you are in bed.
Pain Management
Your doctor and nurses will work with you to help reduce your pain. Typically, you will be given medicine through an IV in the first few hours after surgery. Then you will be switched to oral pain medicine. This may take the form of opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), or over-the-counter pain medication such as acetaminophen. Your doctor may also use a combination of these medications to manage pain.
Be aware that while opioids can relieve pain after surgery, their use has risks and complications. These medications can be addictive and potentially dangerous. It is therefore important to use opioids only as directed by your doctor, to use as little as possible for as short a time as possible, and to stop taking them as soon as your pain starts to improve. Your surgeon will help you with pain management during your recovery.
Rehabilitation
Many patients go home after hip fracture surgery, but some will need short-term care in a rehabilitation facility. Usually, these patients are elderly or have no caregivers at home.
- If you go to a rehabilitation facility, you will need to stay there until you can walk independently and manage your daily activities.
- If you go directly home, you will have in-home physical therapy until you are strong enough to go to therapy at an outside facility.
- It is important to recognize that these types of fractures often occur in elderly people, emphasizing how frail the elderly tend to be. Hip fractures may therefore be challenging for elderly patients to recover from; they often need more assistance in their daily lives and experience a stepwise decrease in their level of function after their hip fracture.
Your doctor will manage your care in the post-operative period. They will check the wound, prescribe physical therapy, and take X-rays to monitor healing.
- If you have had a procedure that includes internal fixation, your doctor will let you know whether you can bear weight immediately or have any limitations or restrictions.
- If you have a hip replacement, you can bear weight fully right away unless you are experiencing complications from surgery.
To assist doctors in the management of hip fractures in the elderly, the American Academy of Orthopaedic Surgeons has conducted research to provide some useful guidelines. These are recommendations only and may not apply to every case. For more information: Plain Language Summary - Clinical Practice Guideline - Hip Fractures - AAOS
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.