Diseases & Conditions
Achondroplasia
Achondroplasia is a bone disorder that results in dwarfism. Children who are born with achondroplasia typically have short arms and legs, a large head, and an average-sized trunk. They are shorter than most other people because of their bone abnormalities.
Achondroplasia begins during early fetal development when a problem in a gene prevents the body from turning cartilage into bone correctly. The disorder is rare, occurring in only about 1 in 10,000 babies born. Having a parent with achondroplasia significantly increases the risk for being born with the disorder, but most babies with achondroplasia are born to parents of average height.
Health complications are common in babies and children with achondroplasia, but with regular checkups and medical care, most of these can be detected early on and managed. Almost all children with the disorder can lead full and active lives.
Description
During early fetal development, much of the skeleton is made up of a strong, flexible body tissue called cartilage. As the fetus grows, this cartilage becomes bone. In achondroplasia, the body has a problem turning cartilage into bone, especially in the long bones of the arms and legs. This results in shortened bones, short stature, and other distinctive physical characteristics.
Because these changes occur late in pregnancy, doctors and parents often don't realize that the child has this condition until birth.
Physical Characteristics
The physical characteristics of achondroplasia are usually noted at birth or in early infancy. These may include:
- Large head size with a prominent forehead
- A flat bridge of the nose and small facial features
- Short arms and legs, with particularly short upper arms and thighs
- Bowed lower legs
- A trunk that is usually near average in size
- Weak muscle tone and loose joints
Other Characteristics
Early on, children with achondroplasia may have delays in the development of some motor skills. This means that they may be older than the average child when they are able to sit or walk by themselves.
Children with achondroplasia do not typicaly have intellectual disability. Children and adults with the condition almost always have normal intelligence.
Cause
Achondroplasia is caused by a mutation in a gene that is involved in skeletal growth and development. It is an autosomal dominant disorder. This means that only one parent needs to pass down the gene mutation for a child to be born with the disorder. It is common for a parent with achondroplasia to have a child who also has achondroplasia, as there is a 50% likelihood of passing on the gene.
However, most babies with achondroplasia are born to parents of average height. More than 80% of achondroplasia births happen when a random, new (de novo) mutation occurs in the gene that is responsible for this condition.
Doctor Examination
Achondroplasia is sometimes diagnosed before birth during a prenatal ultrasound. In this situation, it would be helpful to speak with a pediatric orthopaedic surgeon before your baby is born to learn more about the condition and how it may affect your baby’s health.
To confirm the diagnosis after birth, your doctor will take a complete medical history, perform a physical examination, and use X-rays and other imaging studies. Only occasionally is genetic testing required to confirm the diagnosis.
Treatment
Currently, there is no cure for achondroplasia. Instead, your child's doctor will focus on treating any problems or complications that may arise from the condition. These may include:
- Ear, nose, and throat problems. Differences in how their bones develop make children with achondroplasia more likely to have:
- Frequent ear infections, leading to the risk of hearing loss; placement of ear tubes is often needed.
- Obstructive sleep apnea (the interruption of breathing for short periods); removal of tonsils and adenoids (tissue in the back of the throat) may be necessary.
- Crowded teeth, sometimes requiring tooth removal.
- Obesity. Children and adults with achondroplasia are more likely to be overweight or obese, which can worsen other complications of the condition, such as sleep apnea and back problems. Parents can help lessen the risk of weight gain by modeling healthy eating and exercise habits from an early age.
- Hydrocephalus (excess fluid around the brain). This rare condition can make your baby’s head look too large or swollen. To recognize hydrocephalus early on, your child's doctor will take measurements of your baby’s head during their well-baby checkups. In some cases, the placement of a shunt may be needed to drain the excess fluid.
There are new medications available that can enhance growth for children with achondroplasia. While these medications increase growth, at this time they have not been shown to improve overall health or reduce the need for surgeries or other medical procedures.
Musculoskeletal Complications
It is also common for babies and children with achondroplasia to have abnormalities of the musculoskeletal system that affect the spine and limbs. These may include:
Compression of the upper end of the spinal cord. In babies with achondroplasia, the opening at the base of the skull through which the brainstem and spinal cord pass (foramen magnum) is often too narrow. This can result in compression of the upper end of the spinal cord, which can lead to muscle weakness and breathing problems. For a small number of babies with achondroplasia, this spinal cord compression can be life-threatening.
Your child's doctor may order an MRI scan of your baby’s spine to check the size of the foramen magnum. If it is too narrow, you may be referred to a neurosurgeon who can perform a surgical procedure called decompression to make more room for the spinal cord to pass through the opening in the skull.
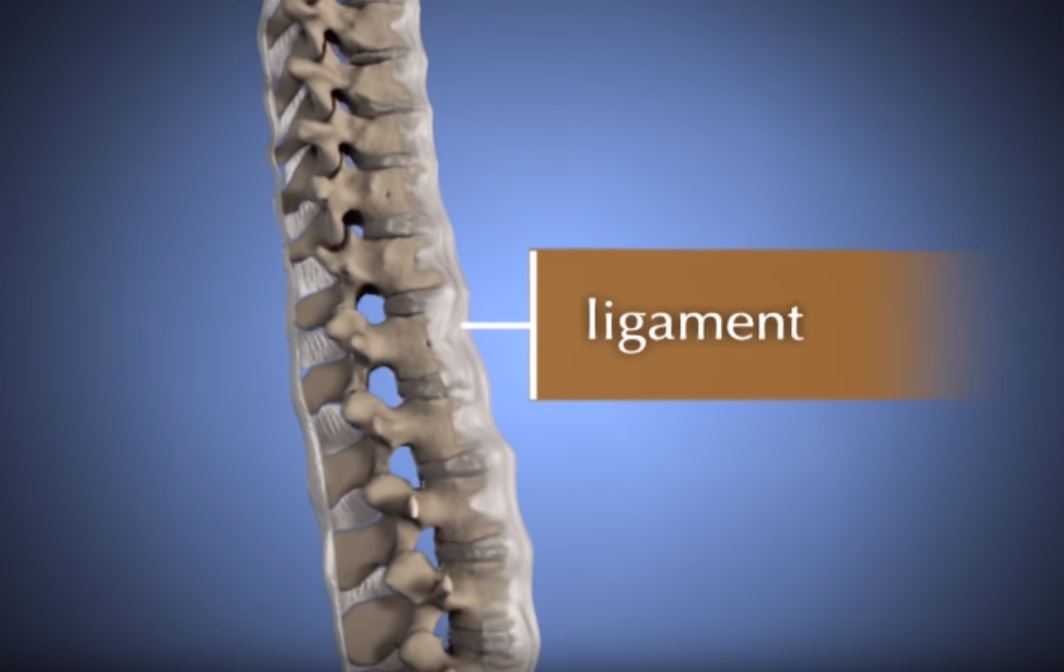
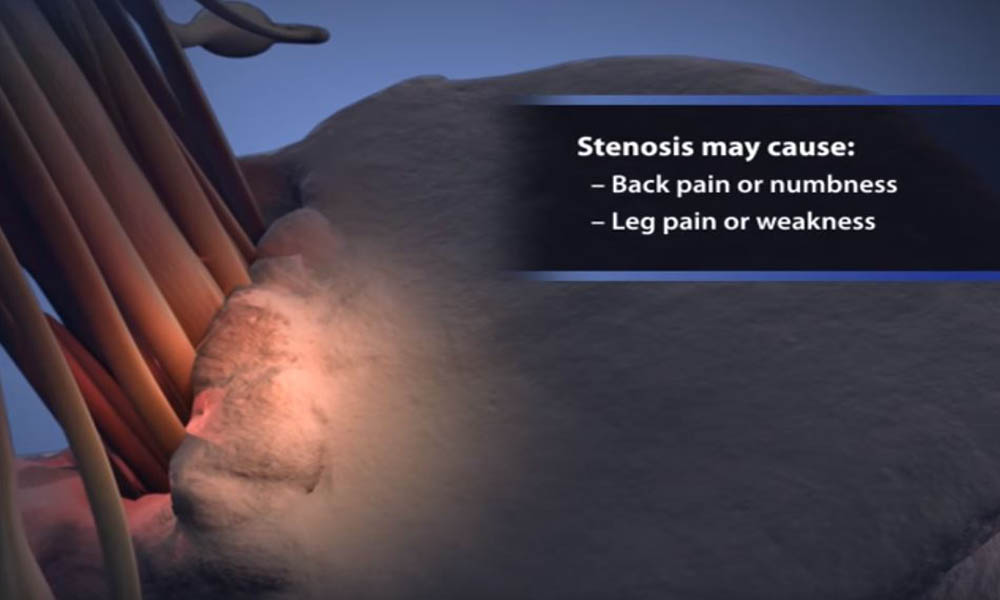
Spinal stenosis. Spinal stenosis is a condition that causes pain, numbness, and weakness in the legs. The condition develops when the space of the spinal canal is too small, putting pressure on the spinal cord and spinal nerve roots. Because of differences in the way the bones (vertebrae) in their spine are formed, spinal stenosis is common in both children and adults with achondroplasia.
Mild symptoms of spinal stenosis will often improve with weight loss, rest, pain medications, and a change in activities. Patients with severe symptoms may need decompression surgery to make more room for the spinal cord and nerves, followed by a procedure to fuse the bones in the spine. In children, decompression may be followed by a procedure to fuse the bones in the spine.
Kyphosis. Kyphosis refers to an excessive roundness or hump in the back. Because they have poor muscle tone and loose joints, it is common for babies with achondroplasia to develop kyphosis. The condition usually goes away when they begin walking and their core muscles become stronger.
Your child's doctor may order regular X-rays to see whether your child's curve is getting bigger, smaller, or staying the same. Children who do not outgrow their curve may need to wear a back brace to prevent it from getting bigger or have surgery to correct it.
Bowed legs. Bowing of the lower legs can cause pain and trouble with walking in children who have achondroplasia. If your child also has loose joints, it can make these symptoms worse. For severe bowing and significant knee pain, your child's doctor may recommend one of two surgeries to straighten the bones in the leg:
- Guided growth. This procedure temporarily stops the growth on one side of the bone, which gives the other side a chance to catch up. As your child grows, the bone straightens over time.
- Osteotomy. In this procedure, the curved bone is cut and realigned to be straight. The bone is held in place while it heals with either a plate and screws, or with an external fixator (a metal frame that is positioned on the outside of the leg and held in place with metal wires and pins).
Limited range of motion in the elbow joints. Some children with achondroplasia may have difficulty straightening their elbows; however, this does not usually interfere with daily activity.
If problems do arise with grooming, self-care, or other everyday activities, assistive devices can help.
If the arm bone above the elbow (humerus) is too short, limiting self-care, surgery to lengthen that bone may beneficial.
Living with Achondroplasia
There is a slight increase in mortality rates in very young children with achondroplasia but, once this early period has passed, their life expectancy is the same as for any other child.
You can help your child live the best life possible right from the start by taking them to all well-baby checkups and annual appointments. These visits give your child's doctor the opportunity to identify and treat any potential complications of achondroplasia early on so that your child can thrive. They also give you the chance to share any questions or concerns you may have about your child’s development.
Because children with achondroplasia will face many social and physical challenges, it is important to help them meet other children with the disorder who can offer friendship, support, and advice.
There are many discussion groups for people with achondroplasia online. In addition, the following organizations can direct you to local programs, support groups, and social events for children with achondroplasia and their families.
Last Reviewed
April 2022
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.