Treatment
Thumb Carpometacarpal (CMC) Arthroplasty
Thumb carpometacarpal (CMC) arthroplasty is a surgery for patients with thumb CMC joint arthritis who continue to have symptoms despite nonsurgical treatment.
- Patients with thumb CMC arthritis have loss of cartilage in the joint that connects the base of the thumb to the wrist. Cartilage helps cushion the joint and allows for smooth, painless motion. Thus, patients with CMC arthritis complain of pain at the base of the thumb that is often made worse by activity.
- In severe cases, patients also can develop a deformity of the thumb that makes it more difficult to perform activities that require grasping and pinching.
Thumb CMC arthroplasty is aimed at improving these symptoms, allowing for better, more painless thumb function.
Anatomy
The thumb is made up of three bones:
- The distal phalanx makes up the very tip of the thumb.
- The next bone toward the wrist is the proximal phalanx. The distal phalanx and proximal phalanx connect via the distal interphalangeal (DIP) joint.
- The bone at the base of the thumb is the metacarpal. It connects to the proximal phalanx via the metacarpophalangeal (MCP) joint.
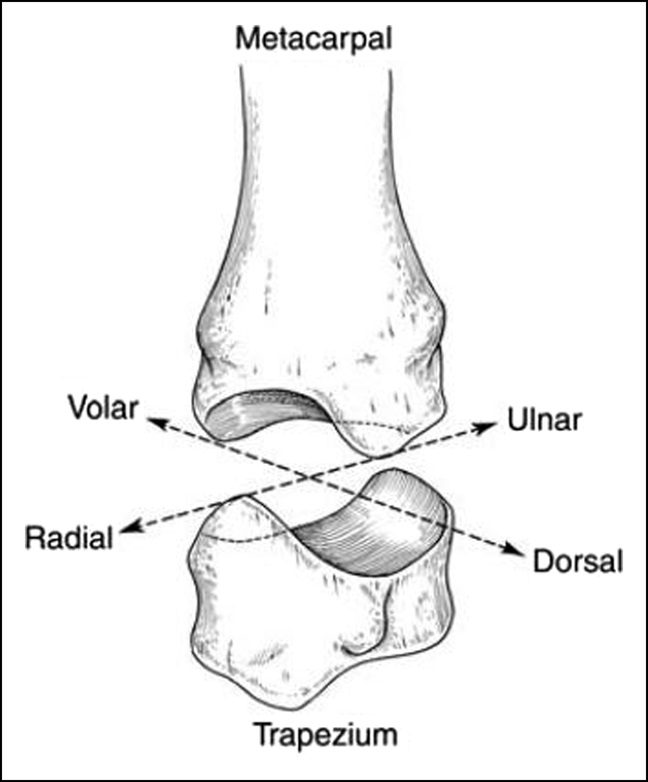
The metacarpal rests on the trapezium, one of the eight bones of the wrist. Together, they make up the carpometacarpal (CMC) joint of the thumb. While the DIP and MCP joints allow for only flexion (bending) and extension (straightening), the CMC joint allows for a variety of different motions.
Treatment
In many cases, your doctor will recommend that you try conservative (nonsurgical) treatments before considering surgery. This may include:
- Splints
- Anti-inflammatory medication (NSAIDs)
- Hand therapy
- Steroid injections
If these treatments don't work, or the surgeon believes the condition is too severe to avoid surgery, then surgery is recommended.
Preparing for the Procedure
Imaging. Typically, you will have X-rays taken before the surgery. This helps the surgeon see how severe the arthritis is and whether there are other conditions that need to be treated at the time of surgery. X-rays also may help the surgeon plan for the type of surgery to be performed; there are several types of CMC arthroplasty procedures to choose from.
Health conditions. Prior to surgery, you should avoid injury to the skin over the thumb. If there is a wound over the surgical site, the procedure may be delayed to avoid infection.
If you are diabetic, you will often be encouraged to keep your blood sugar control as tight as possible. This reduces the risk of post-operative infection and wound issues.
Also to reduce the risk of infections and wound complications, smokers will typically be encouraged to avoid smoking for several weeks prior to the surgery. Learn more about Orthopaedic Surgery and Smoking
Work and home arrangements. You should expect to be sore after surgery for several days to weeks. Thus, you should make arrangements at home and at work to account for this.
- People with sedentary jobs (e.g. working at a computer) may be able to return to work just a few days after surgery.
- Patients with physically demanding jobs (e.g. construction workers) will likely need to take 2 to 3 months off after surgery to allow their wounds to heal and for the thumb to settle into its final position.
Talk to your employer before your procedure about potential missed days or work restrictions.
Anesthesia. For the procedure, patients are often made sleepy, and the surgical site is numbed with medication. Sometimes, before the surgery, the entire arm may be numbed by an anesthesiologist in a procedure known as a "block." This leads to excellent pain control during and after the surgery in many cases.
Most surgeons will apply a tourniquet to the arm to prevent bleeding during the surgery. Some surgeons will keep the patient awake during the surgery and use a cocktail of numbing medicine and blood vessel constricting medicine to provide pain control and prevent bleeding during the surgery without using a tourniquet.
Procedure
The surgery is most commonly performed through one of two incisions:
- A "dorsal incision" on the back of the base of the thumb
- A "Wagner incision" at the base of the thumb at the palm
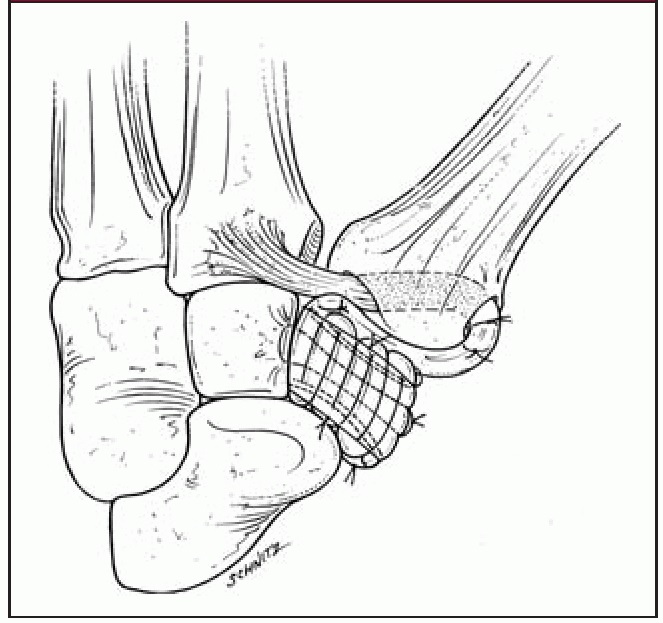
There are a variety of thumb CMC arthroplasty procedures. What they all have in common is removal of the trapezium bone. Once the trapezium is removed, there is no longer an arthritic joint between it and the thumb metacarpal.
To prevent the thumb from collapsing into the space previously filled by the trapezium, a variety of techniques have been developed. These include, but are not limited to:
- Harvesting a tendon from the wrist and weaving it through a drill hole in the metacarpal to hold it up (LRTI)
- Suturing (stitching) together a tendon from the wrist and a thumb tendon to create a "sling" to hold up the metacarpal (APL/FCR sling)
- Placing a temporary pin or a permanent suture (stitch) from the thumb metacarpal to the index finger metacarpal to keep the thumb metacarpal in place
Sometimes, patients with CMC arthritis have arthritis of a nearby joint called the scaphotrapeziotrapezoid (STT) joint. When they do, this arthritis is often treated with debridement (cleaning up) or removal of part of the trapezoid.
Patients may also have arthritis or instability of the thumb MCP joint. This may be addressed at the time of surgery with a fusion of the joint, tightening of the capsule around the joint, or rearranging tendons around the joint.
When the surgery is complete, the wound is cleaned, and a bandage and splint are applied.
The procedure takes around 30 to 60 minutes depending on which type of CMC arthroplasty is performed. It is almost always done on an outpatient basis, meaning the patient gets to go home after surgery and does not have to stay overnight in the hospital.
Recovery
After surgery, patients are commonly groggy from anesthesia, so you should make plans to be driven home by a family member, friend, or neighbor. You will need some rest as the anesthesia wears off.
If you had a block, your arm will be numb and weak. You may be given a sling in the recovery area to use until strength comes back in the arm after a few hours. The pain after surgery may not start for a few hours due to the numbing medication or block you were given for the procedure.
Medications
- You may be sent home with prescription pain medicine, which can be used for pain the first few days after surgery. Many patients find that acetaminophen and ibuprofen are enough and do not need narcotic medications. If you do require narcotics, you should try to come off them as soon as possible, as these medications are highly addictive.
- Antibiotics are not commonly needed after surgery and will not be prescribed in most instances.
Return to Work
As mentioned above:
- If you have a sedentary job, such as a desk job, you may feel up to returning to work a few days after surgery.
- If you have a labor-intensive job, such as those that require lifting heavy objects or operating heavy machinery, you may need a few months off from work.
Wound and Dressing Care
The dressing and splint are commonly left on for 10 to 14 days after surgery to keep the wound sterile and keep stress off of the CMC joint.
After 10 to 14 days, you can remove the bandage and shower. Clean and running water is safe at this time; however, the wound should not be submerged in stagnant water, such as an ocean, lake, pool, or hot tub, for about 30 days after surgery.
Patients typically are placed in a removable splint at this time and start therapy for gentle motion of the thumb. In some cases, patients may be immobilized for as long as 2 to 3 months in a splint or cast before starting therapy.
Complications
Complications from surgery can include:
- Infection
- Wound healing issues
- Injuries to nearby structures, such as nerves, blood vessels and/or tendons
- Lack of improvement after surgery
- Failure of the surgery
In addition:
- Many patients complain of numbness over the tip of the back of the thumb after surgery. This is due to irritation of nerves that cross the surgery site. While these nerves can be accidentally cut during surgery, more commonly the nerves are simply irritated by the operation, and these symptoms will get better over time.
- The deep branch of the radial artery runs through the surgical site and can be injured during surgery, which may cause bleeding in the operating room. In rare cases, injury to the radial artery could cause cold intolerance or poor blood flow to the fingers; however, this is rare.
- Rarely, tendons crossing the surgery site are injured, which may result in reduced function of the thumb.
Long-Term Outcomes
Most patients have soreness and stiffness for several weeks after surgery. It will likely take around 3 months for the surgery to start to feel beneficial. Many surgeons counsel their patients that it can take 9 to 12 months after surgery to see the final results.
Most patients are ultimately happy with the surgery. It has an excellent track record of reducing pain and improving function. However, patients should expect to lose some pinch strength, even in surgeries with an outstanding result.
Recurrence of the condition after surgery is quite rare. When it does happen, it commonly occurs years after surgery. In those cases, or in cases where patients do not improve after surgery, revision (repeat) surgery may be needed.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.