Treatment
Shoulder Joint Replacement
This article was written and/or reviewed by a member of American Shoulder and Elbow Surgeons (ASES).
Shoulder replacement surgery is an increasingly common procedure. It is very effective in relieving shoulder pain and is becoming as successful as hip and knee replacement surgery at reducing pain and enabling patients to resume everyday activities.
Shoulder replacement surgery was first performed in the U.S. in the 1950s to treat severe shoulder fractures. Over the years, shoulder joint replacement has come to be used for many other painful conditions of the shoulder, such as different forms of arthritis.
According to an article in the Journal of Shoulder and Elbow Surgery (JSES), by 2025, the number of annual shoulder replacement procedures in the U.S. could total anywhere from 174,000 to 350,000. That includes total shoulder replacement, hemiarthroplasty, and reverse total shoulder replacement.
If nonsurgical treatments like medications and activity changes are no longer helpful for relieving your shoulder pain, you may want to consider shoulder joint replacement surgery.
Whether you have just begun exploring treatment options or have already decided to have shoulder joint replacement surgery, this article will help you understand more about this valuable procedure.
Anatomy
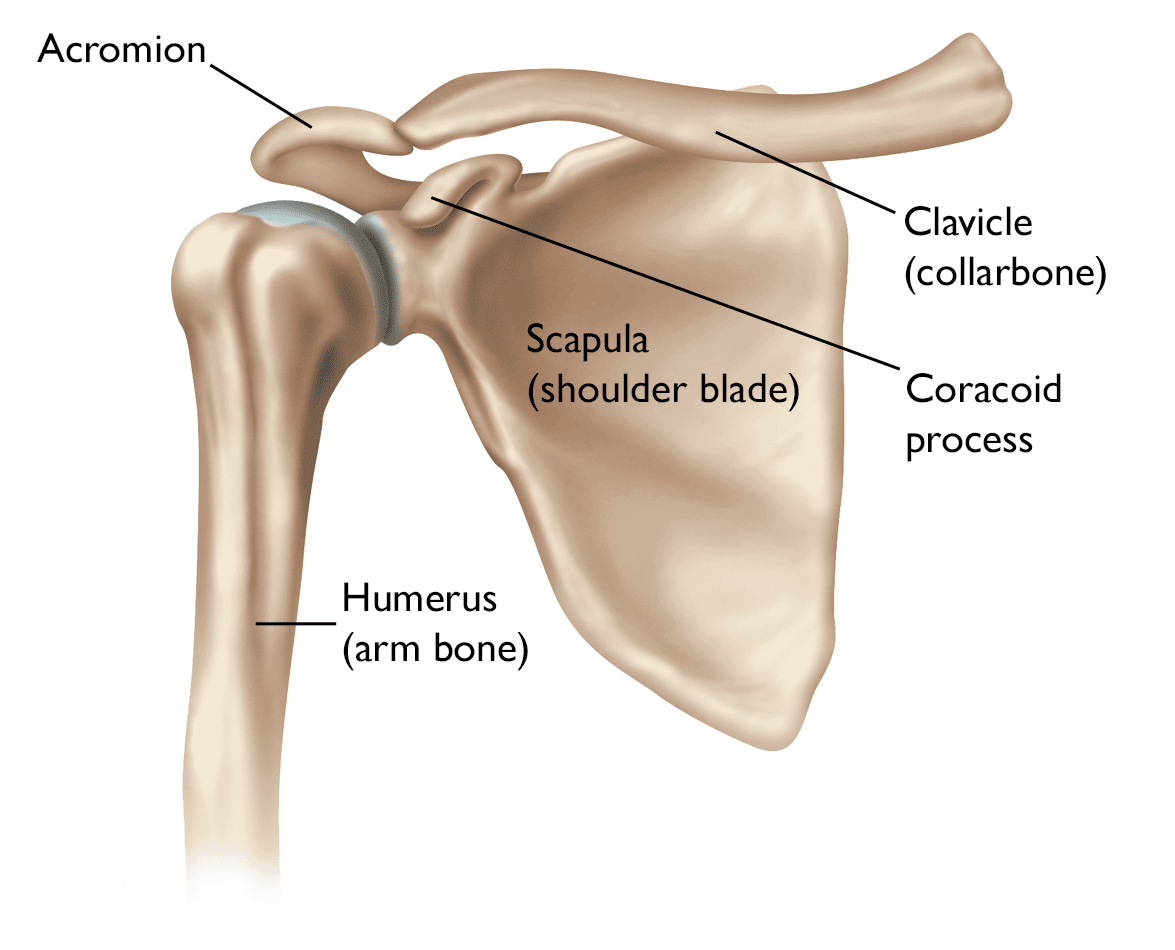
The shoulder is made up of three bones:
- The humerus (upper arm bone)
- The scapula (shoulder blade)
- The clavicle (collarbone)
The shoulder is a ball-and-socket joint: The ball, or head, of the upper arm bone fits into a shallow socket in the shoulder blade. This socket is called the glenoid.
The surfaces of the bones where they touch are covered with articular cartilage, a smooth substance that protects the bones and enables them to move easily. A thin, smooth tissue called synovial membrane covers all remaining surfaces inside the shoulder joint. In a healthy shoulder, this membrane makes a small amount of fluid that lubricates the cartilage and eliminates almost any friction in your shoulder.
The muscles and tendons that surround the shoulder provide stability and support.
All of these structures allow the shoulder to rotate through a greater range of motion than any other joint in the body.
Description
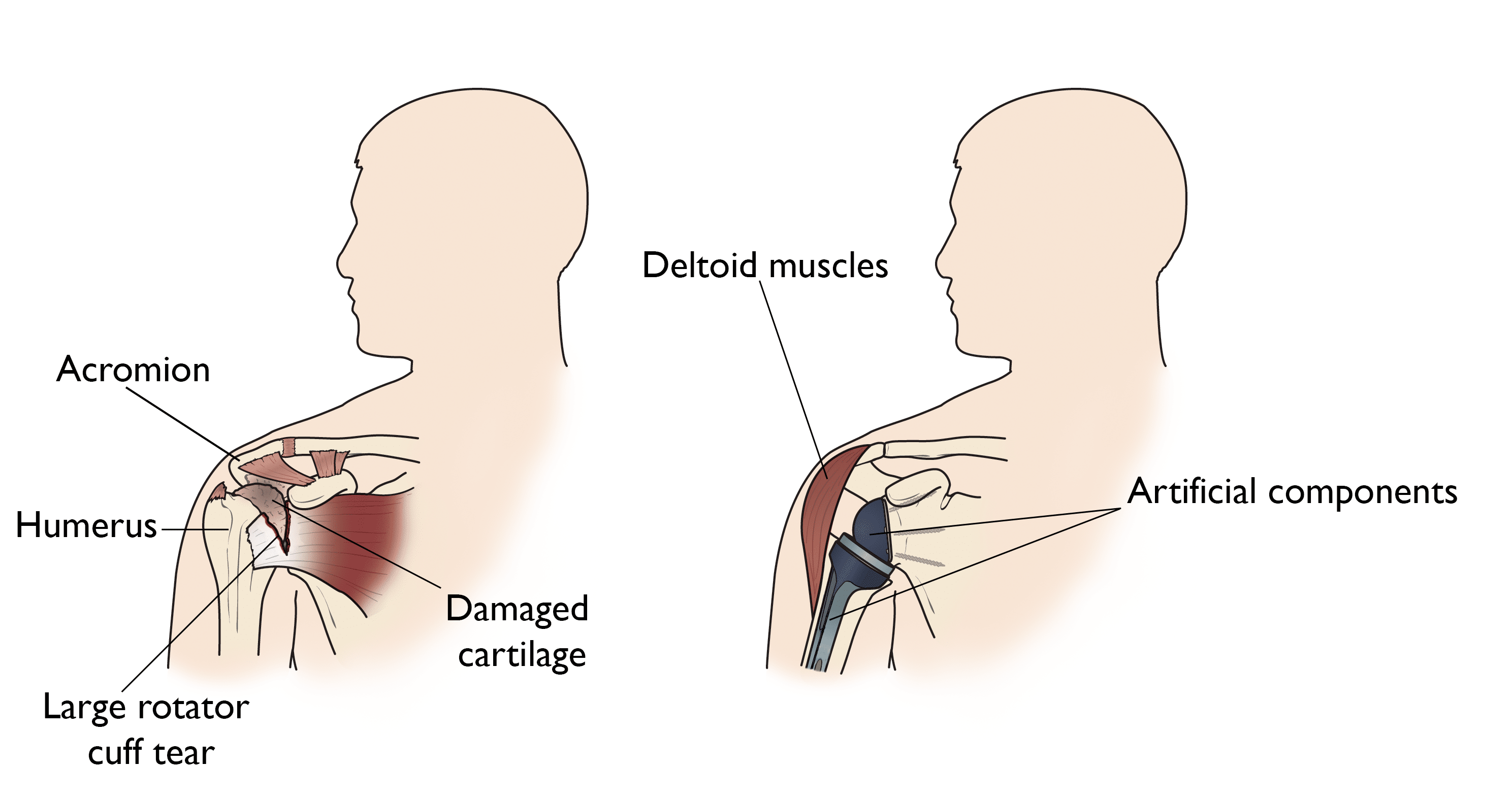
In shoulder replacement surgery, the damaged parts of the shoulder are removed and replaced with artificial components (parts), called a prosthesis.
The treatment options are either:
- Replacement of just the head of the humerus bone (ball)
- Replacement of both the ball and the socket (glenoid)
Cause
Several conditions can cause shoulder pain and disability, and lead patients to consider shoulder joint replacement surgery.
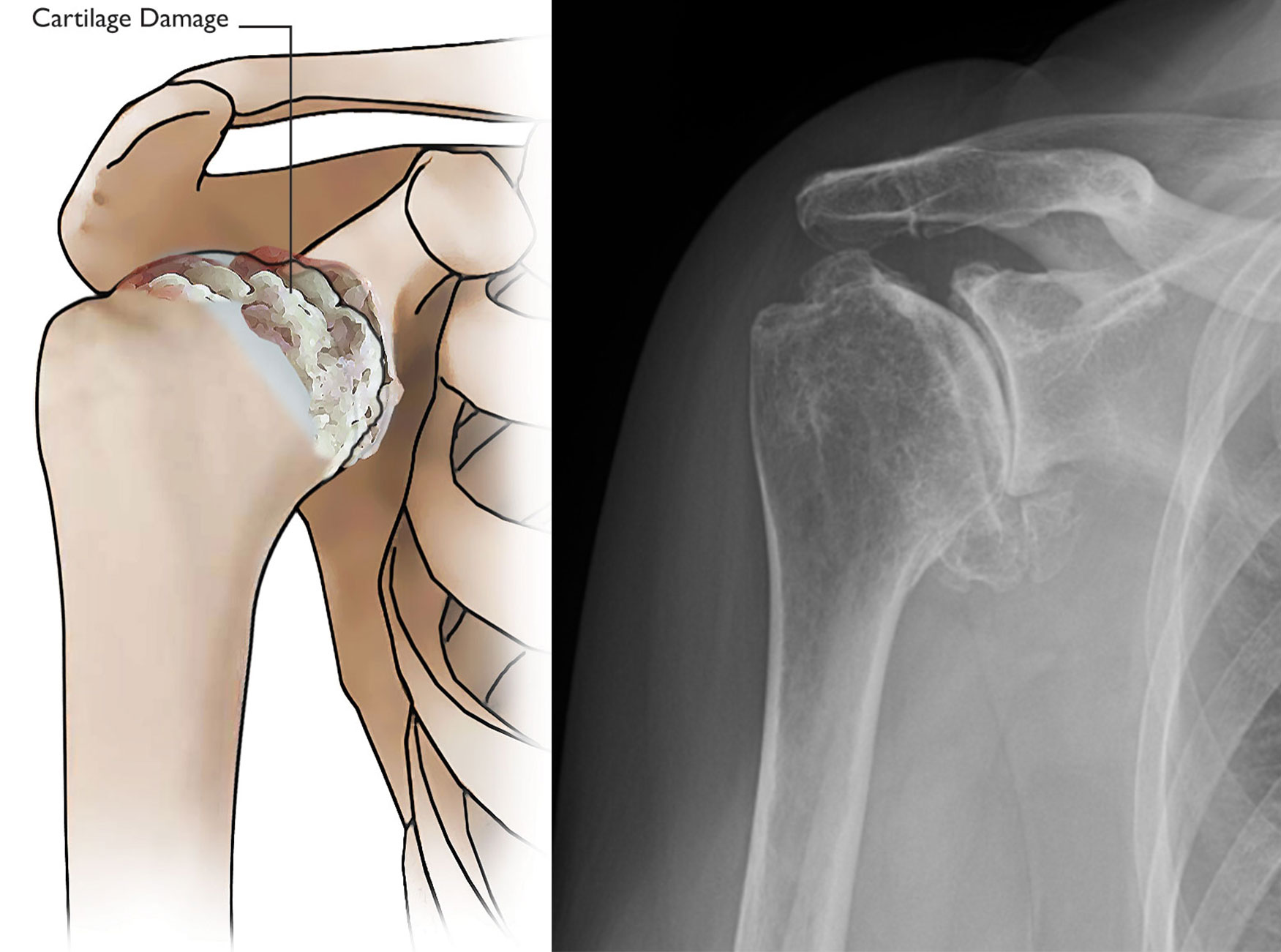
Osteoarthritis (Degenerative Joint Disease)
Osteoarthritis is an age-related wear-and-tear type of arthritis. It usually occurs in people 50 years of age and older, but it may occur in younger people, too. The cartilage that cushions the bones of the shoulder wears away. The bones then rub against one another. Over time, the shoulder joint slowly becomes stiff and painful.
Unfortunately, there is no way to prevent the development of osteoarthritis. It is a common reason people have shoulder replacement surgery.
Rheumatoid Arthritis
This is a disease in which the synovial membrane that surrounds the joint becomes inflamed and thickened. This chronic inflammation can damage the cartilage and eventually cause cartilage loss, pain, and stiffness. Rheumatoid arthritis is the most common form of a group of disorders termed inflammatory arthritis.
Posttraumatic Arthritis
This can follow a serious shoulder injury. Fractures of the bones that make up the shoulder or tears of the shoulder tendons or ligaments may damage the articular cartilage over time. This can occur after a broken bone, a dislocation, or both.
Like the other forms of arthritis, posttraumatic arthritis causes shoulder pain and limits shoulder function.
Rotator Cuff Tear Arthropathy
A patient with a very large, long-standing rotator cuff tear may develop a condition called cuff tear arthropathy. In this condition, the changes in the shoulder joint due to the rotator cuff tear may lead to arthritis and destruction of the joint cartilage.
Avascular Necrosis (Osteonecrosis)
Avascular necrosis (AVN), or osteonecrosis, is a painful condition that occurs when the blood supply to the bone is disrupted. Because bone cells die without a blood supply, osteonecrosis can ultimately cause destruction of the shoulder joint and lead to arthritis.
Risk factors for avascular necrosis include:
- Chronic steroid use
- Complications from deep sea diving
- Heavy alcohol use
- Severe fracture of the shoulder
- Sickle cell disease
Severe Fractures
A severe fracture of the shoulder is another common reason people have shoulder replacements. When the head of the upper arm bone is shattered, it may be very difficult for a doctor to put the pieces of bone back in place. In addition, the blood supply to the bone pieces can be interrupted. In this case, a surgeon may recommend a shoulder replacement.
Older patients with osteoporosis are most at risk for severe shoulder fractures. In fact, even a fall from standing height can cause a severe shoulder fracture in an older person whose bones are weakened due to osteoporosis.
Failed Previous Shoulder Replacement Surgery
Although uncommon, some shoulder replacements fail, most often because of:
- Implant loosening
- Wearing down of the implant parts
- Infection
- Dislocation
When this occurs, a second joint replacement surgery — called a revision surgery — may be necessary.
Is Shoulder Joint Replacement for You?
The decision to have shoulder replacement surgery should be a cooperative one between you, your family, your family physician, and your orthopaedic surgeon.
There are several reasons why your doctor may recommend shoulder replacement surgery. People who benefit from surgery often have:
- Severe shoulder pain that interferes with everyday activities, such as reaching into a cabinet, dressing, toileting, and washing.
- Moderate to severe pain while resting. This pain may be severe enough to prevent sleep.
- Loss of motion and/or weakness in the shoulder.
- Failure to substantially improve with other treatments such as anti-inflammatory medications, cortisone injections, and/or physical therapy.
Orthopaedic Evaluation
You may be referred to an orthopaedic surgeon for a thorough evaluation to determine if you can benefit from this surgery.
An evaluation with an orthopaedic surgeon consists of several components:
- A medical history. Your orthopaedic surgeon will gather information about your general health and ask you about the extent of your shoulder pain and your ability to function.
- A physical examination. This will assess shoulder motion, stability, and strength.
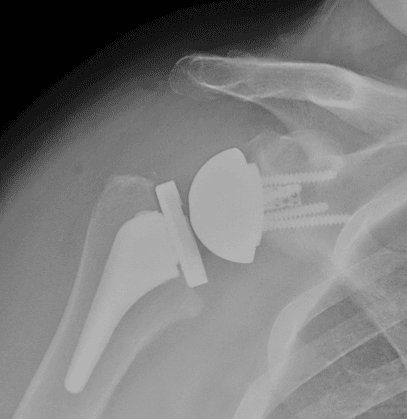
- X-rays. X-rays help to determine the extent of damage in your shoulder. They can show loss of the normal joint space between bones, flattening or irregularity in the shape of the bone, bone spurs, and loose pieces of cartilage or bone that may be floating inside the joint.
- Other tests. Occasionally, your doctor may order blood tests, a computed tomography (CT) scan, or a magnetic resonance imaging (MRI) scan to determine the condition of the bones and soft tissues of your shoulder.
Your orthopaedic surgeon will review the results of your evaluation with you and discuss whether shoulder joint replacement is the best method to relieve your pain and improve your function. The surgeon will also talk to you about other possible treatment options, such as:
- Medications
- Injections
- Physical therapy
- Other types of surgery
Shoulder Replacement Options
Shoulder replacement surgery is highly technical. It should be performed by a surgical team with a lot of experience in this procedure.
There are several types of shoulder replacements. Your surgeon will evaluate your situation carefully before making any decisions. They will discuss with you which type of replacement will best meet your health needs. Do not hesitate to ask which type of implant you will receive, and why that choice is right for you.
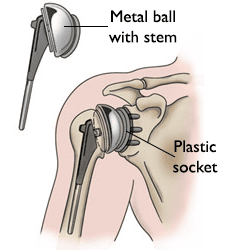
Total Shoulder Replacement
The standard total shoulder replacement involves replacing the arthritic joint surfaces with a highly polished metal ball and a plastic socket.
These components come in various sizes. They may be either cemented or press fit into the bone.
- If the bone is of good quality, your surgeon may choose to use a non-cemented (press-fit) humeral component.
- If the bone is soft, the humeral component may be implanted with bone cement.
- In most cases, a plastic (polyethylene) glenoid (socket) component is implanted with bone cement.
Implantation of a glenoid component is not advised if:
- The glenoid has good cartilage
- The glenoid bone is severely deficient
- The rotator cuff tendons are torn and cannot be repaired
Patients with bone-on-bone osteoarthritis and intact rotator cuff tendons are generally good candidates for conventional total shoulder replacement.
Hemiarthroplasty
Depending on the condition of your shoulder, your surgeon may replace only the ball. This procedure is called a hemiarthroplasty.
In a traditional hemiarthroplasty, the surgeon replaces the head of the humerus with a metal ball, similar to the component used in a total shoulder replacement.
Some surgeons recommend hemiarthroplasty when the humeral head is severely fractured but the socket is normal. Hemiarthroplasty may also be the best option for patients with:
- Arthritis that involves only the head of the humerus, with a glenoid that has a healthy and intact cartilage surface
- Severely weakened or deficient (not enough) bone in the glenoid
- Severely torn rotator cuff tendons and arthritis
Sometimes, surgeons make the decision between a total shoulder replacement and a hemiarthroplasty in the operating room at the time of the surgery.
Studies show that patients with osteoarthritis get better pain relief from total shoulder arthroplasty than from hemiarthroplasty.
Resurfacing Hemiarthroplasty
Resurfacing hemiarthroplasty involves replacing just the joint surface of the humeral head with a cap-like prosthesis without a stem. With its bone-preserving advantage, it offers those with arthritis of the shoulder an alternative to the standard stemmed shoulder replacement.
Resurfacing hemiarthroplasty may be an option for you if:
- The glenoid still has an intact cartilage surface
- There has been no fresh fracture of the humeral neck or head
- There is a desire to preserve humeral bone
For patients who are young or very active:
- Resurfacing hemiarthroplasty avoids the risks of component (implant part) wear and loosening that may occur with conventional total shoulder replacements in this patient population.
- Due to its more conservative nature, resurfacing hemiarthroplasty may be easier to convert to total shoulder replacement, if necessary, at a later time.
Reverse Total Shoulder Replacement
Another type of shoulder replacement is called reverse total shoulder replacement. Reverse total shoulder replacement is used for people who have:
- Completely torn rotator cuffs with severe arm weakness
- The effects of severe arthritis and rotator cuff tearing (cuff tear arthropathy)
- A previous shoulder replacement that failed
- Severe humeral head fractures, with or without underlying arthritis
For these patients, a conventional total shoulder replacement can still leave them with pain. They may also be unable to lift their arm up past a 90° angle. Not being able to lift your arm away from the side can be severely debilitating.
In reverse total shoulder replacement, the socket and metal ball are switched:
- A metal ball is attached to the shoulder bone.
- A plastic socket is attached to the upper arm bone.
This allows the patient to use the deltoid muscle instead of the torn rotator cuff to lift the arm.
Learn more: Reverse Total Shoulder Replacement
Complications
Your orthopaedic surgeon will explain the potential risks and complications of shoulder joint replacement, including those related to the surgery itself and those that can occur over time after your surgery.
When complications occur, most are successfully treatable. Possible complications include the following.
Infection
Infection is a complication of any surgery. In shoulder joint replacement, infection may occur in the wound or deep around the prosthesis. It may happen while in the hospital or after you go home. It may even occur years later.
- Minor infections in the wound area are usually treated with antibiotics.
- Major or deep infections may require more surgery and removal of the prosthesis.
Any infection in your body can spread to your joint replacement.
Prosthesis Problems
Although prosthesis designs and materials, as well as surgical techniques, continue to advance:
- The prosthesis may wear down and the components (parts) may loosen from the bone.
- The components (parts) of a shoulder replacement may also dislocate.
Excessive wear, loosening, or dislocation may require additional surgery (revision procedure).
Nerve damage
Nerves in the area of the joint replacement may be damaged during surgery, although this type of injury is infrequent. Over time, these nerve injuries often improve and may completely recover.
Fractures
When you have an implant in your bone, the bones around the implant can become weaker, and you can sustain a stress fracture of the bones surrounding the implant. These stress fractures can be serious complications.
Preparing for Surgery
Medical Evaluation
If you decide to have shoulder replacement surgery, your orthopaedic surgeon may ask you to schedule a complete physical examination with your family physician several weeks before surgery. This is needed to make sure you are healthy enough to have the surgery and complete the recovery process.
Many patients with chronic medical conditions, like heart disease or kidney disease, must also be evaluated by a specialist, such as a cardiologist or nephrologist, before the surgery.
Medications
Be sure to talk to your orthopaedic surgeon about the medications you take. Some medications may need to be stopped before surgery. For example, the following over-the-counter medicines may cause excessive bleeding and should be stopped 2 weeks before surgery:
- Non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin, ibuprofen, and naproxen
- Most arthritis medications
If you take blood thinners, either your primary care doctor or cardiologist will advise you about stopping these medications before surgery.
Learn more: Preparing for Surgery - Medication Safety Checklist
Home Planning
Making changes in your home before surgery can make your recovery period easier.
For the first several weeks after your surgery, it will be hard to reach high shelves and cupboards. Before your surgery, be sure to go through your home and place any items you may need afterwards on low shelves.
When you come home from the hospital, you will need help for a few weeks with some daily tasks like dressing, bathing, cooking, and laundry. If you will not have any support at home immediately after surgery, or if financial limitations will make it challenging to recover at home, you may need a short stay in a rehabilitation facility until you become more independent.
Learn more: Joint Replacement for Patients With Limited Social or Financial Resources
Learn more: Preparing for Joint Replacement Surgery
Your Surgery
Before Your Operation
Wear loose-fitting clothes and a button-front shirt when you go to the hospital for your surgery. After surgery, you will be wearing a sling and will have limited use of your arm.
You, your anesthesiologist, and your surgeon will discuss the type of anesthesia to be used. You may be given:
- General anesthetic (you are asleep for the entire operation)
- Regional anesthetic (you may be awake but have no feeling around the surgical area)
- A combination of both types of anesthesia
Surgical Procedure
The procedure to replace your shoulder joint with an artificial device usually takes about 2 hours.
After surgery, you will be moved to the recovery room, where your recovery from anesthesia is monitored.
After you wake up, you will either be discharged home (outpatient, or same-day, surgery) or admitted overnight to the hospital for observation. Some patients with other health conditions (e.g., heart disease, diabetes) or limited help at home may need a longer hospital stay and/or inpatient rehabilitation.
Recovery
- Your medical team will give you antibiotics to prevent infection.
- Most patients are able to eat solid food and get out of bed the day after surgery.
- If you are admitted to the hospital, you will most likely be able to go home the first day after surgery (for example, if you have surgery on Monday, you will be able to go home on Tuesday).
Pain Management
After surgery, you will feel some pain. This is a natural part of the healing process. Your doctor and nurses will work to reduce your pain, which can help you recover from surgery faster.
Medications are often prescribed for short-term pain relief after surgery. Many types of medicines are available to help manage pain, including:
- Opioids
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Local anesthetics.
Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids.
Be aware that although opioids help relieve pain after surgery, their use has risks and complications. These medications can be addictive and potentially dangerous. It is therefore important to use opioids only as directed by your doctor, to use as little as possible for as short a time as possible, and to stop taking them as soon as your pain starts to improve. Tell your doctor if your pain has not begun to improve within a few days after surgery.
Pain management is an important part of your recovery. You will begin physical therapy soon after surgery, and when you feel less pain, you can start moving sooner and get your strength back more quickly. Talk with your doctor if post-operative pain becomes a problem.
Rehabilitation
A careful, well-planned rehabilitation program is critical to the success of a shoulder replacement. You usually start gentle physical therapy soon after the operation. Your surgeon or physical therapist will provide you with a home exercise program to strengthen your shoulder and improve flexibility.
Your Recovery at Home
When you leave the hospital, your arm will be in a sling. You will need the sling to support and protect your shoulder for the first 2 to 6 weeks after surgery, depending on the complexity of your surgery and your surgeon's preference.
Wound care. You will have staples running along your wound or a suture beneath your skin. The staples will be removed several weeks after surgery. A dissolving suture beneath your skin will not require removal.
Avoid soaking the wound in water until it has thoroughly sealed and dried. You may continue to bandage the wound to prevent irritation from clothing. Your surgeon or a member of their team will give you specific instructions.
Activity
- Exercise is a critical component of home care, particularly during the first few weeks after surgery. Follow your surgeon's home exercise plan to help you regain strength.
- Most patients are able to perform simple activities such as eating, dressing, and grooming, within 2 weeks after surgery.
- Some pain with activity and at night is common for several weeks after surgery.
- You should not drive a car for 2 to 6 weeks after surgery.
Do's and Don'ts
The success of your surgery will depend largely on how well you follow your orthopaedic surgeon's instructions at home during the first few weeks after surgery. Here are some common do's and don'ts for when you return home:
Do's
- Do follow the program of home exercises prescribed for you. You may need to do the exercises 2 to 3 times a day for a month or more.
- Do ask for assistance. Your physician may be able to recommend an agency or facility to help if you do not have home support. Learn more: Joint Replacement for Patients With Limited Social or Financial Resources
Don'ts
- Don't use the arm to push yourself up in bed or from a chair because this requires forceful contraction of muscles.
- Don't place your arm in any extreme position, such as straight out to the side or behind your body, for the first 6 weeks after surgery.
- Don't overdo it! If your shoulder pain was severe before the surgery, the experience of pain-free motion may lull you into thinking that you can do more than is prescribed. Early overuse of the shoulder may result in severe limitations in motion.
- Don't lift anything heavier than a glass of water for the first 2 to 6 weeks after surgery.
- Don't participate in contact sports or do any repetitive heavy lifting after your shoulder replacement.
Hundreds of thousands of patients have experienced an improved quality of life after shoulder joint replacement surgery. They experience less pain, improved motion and strength, and better function.
Research
There are ongoing efforts to design and develop newer and better shoulder replacements that can be performed with less invasive surgical techniques.
Researchers are also collecting data to determine which patients are the best candidates for which type of shoulder replacement surgery. This information will allow your surgeon to offer you the best recommendation for the treatment of your arthritic shoulder.
To help doctors in the management of glenohumeral joint arthritis, the American Academy of Orthopaedic Surgeons has conducted research to provide some useful guidelines. These are recommendations only and may not apply to every case. For more information: Glenohumeral Joint Osteoarthritis - Clinical Practice Guideline (CPG) | American Academy of Orthopaedic Surgeons (aaos.org)
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.