Treatment
Bone Grafts in Spine Surgery
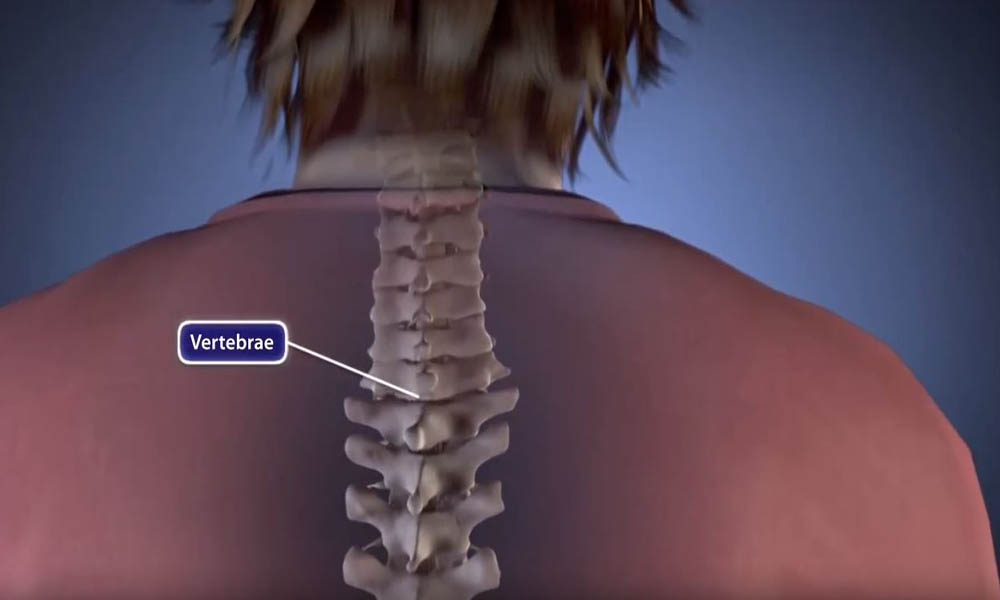
Spinal fusion is one of the most common surgeries performed on the neck or back. The basic idea is to fuse together painful or unstable bones in the spine so that they heal into a single, solid bone.
While bones can sometimes fuse on their own, spine surgeons use several strategies during surgery to help your spine with this process and improve the chances of a successful fusion — including many types of bone grafts and other added substances.
For successful fusion of the bones, there must typically be:
- Stability during the process of fusion. Therefore, screws, rods, and/or plates are used to hold the bones still.
- Cells that can make bone, proteins to stimulate bone, and a scaffold on which bone can be built. If a bone graft material has all of these properties, it can successfully make bone. If it lacks one or more of these properties, the bone graft material must be combined with other graft materials.
There are many bone graft options available today. The graft or combination of grafts that will work best for you depends on which section of your spine needs to be fused, your age, and your general health. Your surgeon will discuss your options with you.
Types of Bone Grafts
Local Bone Autograft
In most spinal fusion procedures, parts of the spinal bones are removed during surgery. This removed bone is often saved during surgery and used as the graft. The bone is essentially recycled; it is moved from an area where it is no longer needed to the area that the surgeon wants to fuse.
The advantages of using local bone are:
- It is the patient's own bone and, therefore, cannot be rejected.
- It requires no additional incision.
- This graft has all the necessary properties to create more bone for fusion to occur.
The only disadvantage is that there is a limited amount of bone that can be collected in this area, and sometimes it is not enough.
Autograft
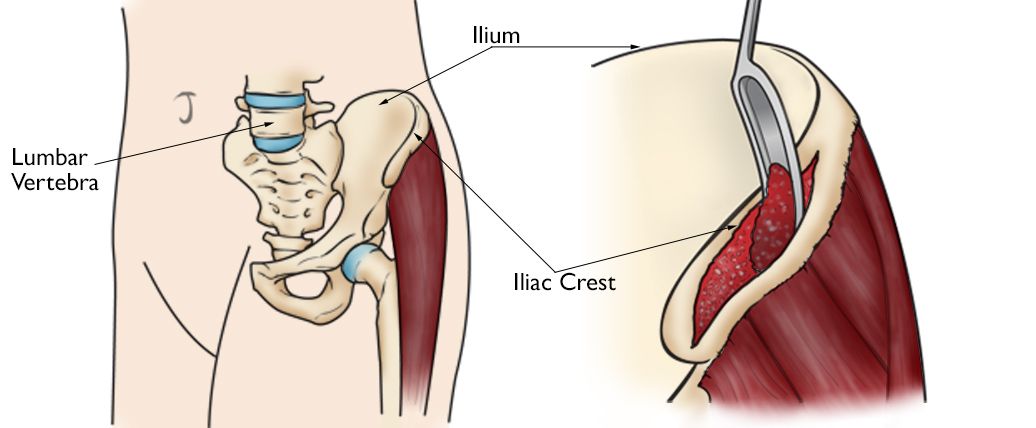
The standard technique used in fusion is to take extra bone from one part of the patient's body (harvest) and move (graft) it to another part of the body, such as the spine. This type of bone graft is called an autograft.
The surgeon usually takes the bone from an area of the body where its removal will not cause a problem. In spine surgery, the bone is typically harvested from the iliac crest, which is the rim of the pelvic bone. The surgeon uses sharp tools to scoop the bone out of the iliac crest.
Bone taken from the iliac crest has been used with good results. The advantages of using iliac crest autograft are:
- It contains cells, proteins, and scaffolding to promote bone healing.
- It is the patient's own bone and therefore does not get rejected.
The disadvantages of using iliac crest autograft are:
- The surgeon must make another incision, which has its own associated risks.
- There may be pain at the donor site.
- There is a limited amount of bone in the iliac crest, especially as we get older and our bone thins and weakens.
- The iliac crest may fracture or break.
- An infection or bleeding may occur.
As newer technologies have emerged, this technique has been used less frequently. Surgeons now typically reserve this more invasive technique for high-risk patients. This includes patients who have had difficulty fusing in the past, patients who smoke, or patients who otherwise may not be as likely to achieve fusion.
Cadaver or Allograft Bone
Many surgeons use bone that is harvested from a donor or cadaver. This type of graft — called an allograft — is typically acquired through a bone bank. Like other organs, bone can be donated upon death. After donation, the bone is sterilized and freeze-dried.
Allografts have been used for a long time in spinal fusion surgery. Unlike autografts taken from a patient, allografts do not form new bone on their own. Instead, the allograft works as a scaffold on which our body can build new bone. Over time, the natural bone replaces the donor bone.
The advantages of using allografts are:
- Allograft bone comes in different shapes and sizes to fit into the area of the spine where it is needed.
- In most cases, allografts do a good job of getting bone to heal.
- Because the donor bone is dead and is used only as a scaffold for bone growth, the tissue is rarely rejected. Therefore, this graft does not need to have cells or proteins to stimulate growth.
- The transmission of diseases from the donor bone is also very rare.
Biologics or Proteins
We all have proteins in our bodies that naturally stimulate bone growth. One protein that is particularly powerful at stimulating bone growth is bone morphogenic protein (BMP). Synthetic BMP has been used to promote solid spine fusions for some time and is a common graft option.
BMP use has been widely studied and proven to increase fusion rates with minimal additional risks. BMP can cause local swelling and therefore is not commonly used in anterior neck surgeries (procedures performed through the front of the neck) due to risk of airway compression.
Demineralized Bone Matrix (DBM)
DBM is made by removing calcium from bone. This creates a scaffold that has necessary proteins and structure available for new bone to form within.
The disadvantage of this graft is that there are no cells that can form bone. Like allografts, DBM serves as a scaffold for bone to grow. Because of the lack of bone cells, DBM relies on the body or other added substances to create bone.
Synthetic Bone
Synthetic bone grafts are made from calcium materials and are often called ceramics. They are similar in shape and consistency to autograft bone. Ceramics have the advantage of being made without cadaver bone and are available in large amounts.
Like DBM, these grafts do not have any cells that can become bone. They also do not have any proteins to stimulate growth. As a result, synthetic grafts are often combined with other bone products to be successful.
Stem Cells
Stem cells can be harvested from the patient themselves, a living donor, or a cadaver. Stem cells are living cells that can transform into bone cells and aid in the fusion. They are unlikely to cause tissue rejection because they are basic cells that have not differentiated into (transformed into) specific cell types.
While stem cells show promise in many fields of medicine, there is limited evidence supporting routine use in spine surgery to achieve fusion. Although stem cells have all three properties needed to make bone, there probably are not enough living cells to make bone on their own.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.