Diseases & Conditions
Toe and Forefoot Fractures
Fractures of the toes and forefoot are quite common. These fractures can result from:
- A direct blow to the foot — such as accidentally kicking something hard or dropping a heavy object on your toes.
- The overuse and repetitive stress that comes with participating in high-impact sports like running, football, and basketball; this is called a stress fracture.
Although fracturing a bone in your toe or forefoot can be painful, it rarely requires surgery. In most cases, a fracture will heal with rest and a change in activities.
Anatomy
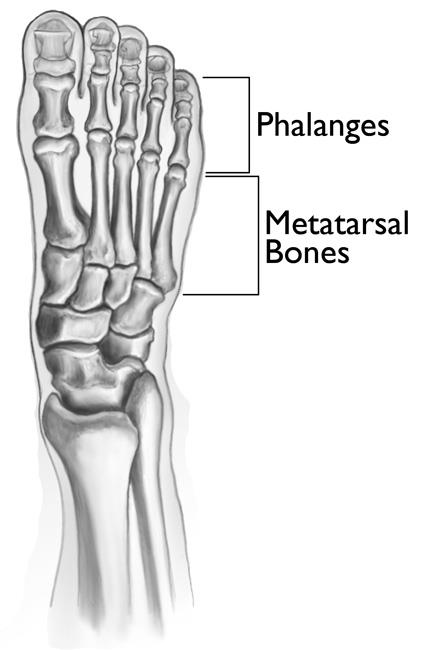
The forefoot has five metatarsal bones and 14 phalanges (toe bones). There are three phalanges in each toe — except for the first toe, which usually has only two.
All the bones in the forefoot are designed to work together when you walk. A fracture, or break, in any of these bones can be painful and impact how your foot functions.
Description
Toe and forefoot fractures may be either:
- Nondisplaced, where the bone is cracked but the ends of the bone stay properly aligned
- Displaced, where the ends of the broken bones have partially or completely separated and are out of alignment
Fractures can also be divided into:
- Closed fractures, where the skin is not broken
- Open fractures, where the skin is broken, and the wound extends down to the bone. Open fractures are particularly serious because, once the skin is broken, bacteria can enter the wound and cause infection in the bone. Immediate treatment is required to prevent infection.
Symptoms
The most common symptoms of a toe or forefoot fracture are pain and swelling. Other symptoms may include:
- Bruising or discoloration that extends to nearby parts of the foot
- Pain with walking and weightbearing
First Aid
If you think you have a fracture, it is important to see your doctor as soon as possible. A fracture that is not treated can lead to chronic foot pain and arthritis and affect your ability to walk.
While you are waiting to see your doctor, you should do the following:
- Apply ice to help reduce swelling.
- Elevate your foot as much as possible.
- Limit weightbearing.
- Lightly wrap your foot in a soft compressive dressing.
Doctor Examination
Physical Examination
When you see your doctor, they will take a history to find out how your foot was injured and ask about your symptoms. Your doctor will then examine your foot and may compare it to the foot on the opposite side.
During the exam, the doctor will look for:
- Swelling
- Tenderness over the fracture site
- Bruising or discoloration — your foot may be red or ecchymotic ("black and blue")
- Deformity
- Skin abrasions or open wounds
- Loss of sensation — an indication of nerve injury
Imaging Tests
Your doctor will also order imaging tests to help diagnose the fracture.
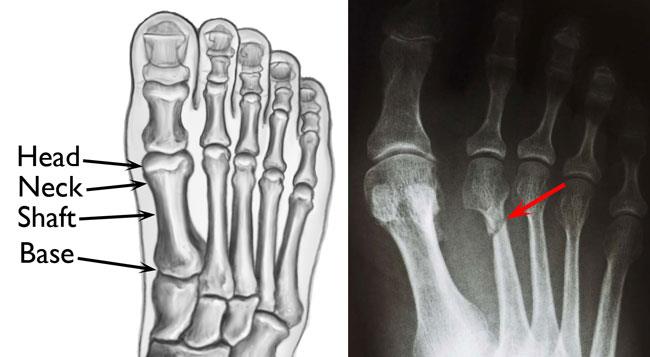
X-rays. X-rays provide images of dense structures, such as bone. An X-ray can usually be done in your doctor's office.
Most fractures can be seen on X-rays. A stress fracture, however, may start as a tiny crack in the bone and may not be visible on a first X-ray.
In many cases, a stress fracture cannot be seen until several weeks later when it has actually started to heal, and a type of healing bone called callus appears around the fracture site.
Magnetic resonance imaging (MRI) scans. If your doctor suspects a stress fracture but cannot see it on an X-ray, they may recommend an MRI scan.
More sensitive than an X-ray, an MRI can detect changes in the bone that may indicate a fracture. Unlike an X-ray, there is no radiation with an MRI.
Treatment
Treatment for a toe or forefoot fracture depends on:
- The location of the injury
- The type of fracture
Fractures of the Toes
Even though toes are small, injuries to the toes can be very painful.
- A fracture of the toe may result from a direct injury, such as dropping a heavy object on the front of your foot, or from accidentally kicking or running into a hard object.
- A fracture may also result if you accidentally hit the side of your foot on a hard object on the ground — like a piece of furniture — and your toes are twisted or pulled sideways or in an awkward direction.
The proximal phalanx is the bone in the toe that is closest to the metatarsals. Because it is the longest of the bones in the toe, it is the most likely to fracture.
A fractured toe may become swollen, tender, and discolored. If the bone is out of place, your toe will appear deformed.
Treatment
Most broken toes can be treated without surgery. For several days, it may be painful to bear weight on your injured toe. As your pain subsides, however, you can begin to bear weight as you are comfortable. During this time, it may be helpful to wear a wider than normal shoe.
Taping your broken toe to an adjacent toe can also sometimes help relieve pain.
If the bone is out of place and your toe appears deformed, it may be necessary for your doctor to manipulate, or reduce, the fracture. This procedure is most often done in the doctor's office. You may be given a local anesthetic to numb your foot, and your doctor will then manipulate the fracture back into place to straighten your toe.
Metatarsal Fractures
The metatarsals are the long bones between your toes and the middle of your foot. Each metatarsal has the following four parts:
- Head — which makes a joint with the base of the toe
- Neck — the narrow area between the head and the shaft
- Shaft — the long part of the bone
- Base — which makes a joint with the midfoot
Fractures can occur in any part of the metatarsal, but most often occur in the neck or shaft of the bone.
Like toe fractures, metatarsal fractures can result from either a direct blow to the forefoot or from a twisting injury.
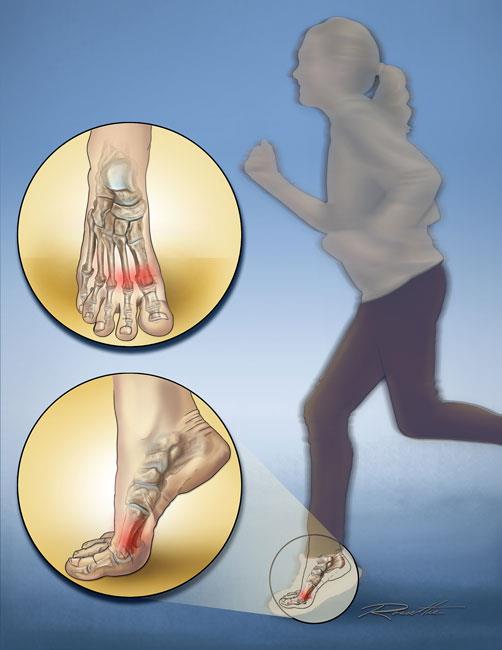
Some metatarsal fractures are stress fractures. Stress fractures are small cracks in the surface of the bone that may extend and become larger over time.
Stress fractures are typically caused by repetitive activity or pressure on the forefoot. They are common in runners and athletes who participate in high-impact sports such as soccer, football, and basketball.
A stress fracture can also come from a sudden increase in physical activity or a change in your exercise routine.
Treatment
Most metatarsal fractures can be treated with an initial period of elevation and limited weightbearing. This is followed by gradual weightbearing, as tolerated, in a cast or walking boot. Surgery is not usually required.
However, if you have fractured several metatarsals at the same time and your foot is deformed or unstable, you may need surgery.
During the procedure, your doctor will make an incision in your foot, then insert pins or plates and screws to hold the bones in place while they heal. This is called internal fixation.
Surgery may be delayed for several days after the injury to allow the swelling in your foot to go down. If you have an open fracture, however, your doctor will perform surgery more urgently.
Fifth Metatarsal Fractures
The fifth metatarsal is the long bone on the outside of your foot. Injuries to this bone may act differently than fractures of the other four metatarsals.
Most commonly, the fifth metatarsal breaks through the base of the bone. This usually occurs from an injury where the foot and ankle are twisted downward and inward.
In this type of injury, the ligament that attaches to the base of the fifth metatarsal may stretch and pull a fragment of bone away from the base. Since the fragment is pulled away from the rest of the bone, this type of injury is called an avulsion fracture.
Treatment
Most fifth metatarsal fractures can be treated with weightbearing as tolerated, and immobilization in a cast or walking boot. However, if an avulsion fracture results in a large, displaced fracture fragment, your doctor may need to:
- Do an open reduction and internal fixation with plates and/or intramedullary screws, or
- Possibly remove a portion of the bone and repair the soft tissues
The appropriate treatment depends on:
- The location of the fracture
- The amount of displacement — how much the two ends of the fracture have shifted out of place
- The activity level of the patient
Because Jones fractures are located in an area with poor blood supply, they may take longer to heal.
- In some cases, a Jones fracture may not heal at all, a condition called nonunion. When this happens, surgery is often required.
- Your doctor may recommend surgery as initial treatment for a Jones fracture if there are concerns about delayed healing and/or the patient is highly active (e.g., a competitive athlete or person with a physically demanding job).
Recovery
- For a broken toe, it may take 6 to 8 weeks before you are comfortable walking in normal shoewear. However, it is normal for the toe to still be achy and swollen for 3 to 6 months, and X-rays may not show full healing for 1 year or more.
- Metatarsal fractures usually heal enough for weightbearing in 6 to 8 weeks but may take longer. Your doctor will take follow-up X-rays to make sure that the bone is properly aligned and healing. Even with proper healing, your foot may be swollen for several months, and it may be hard to find a comfortable shoe.
Your doctor will tell you when it is safe to resume activities and return to sports. If you experience continued pain, you should stop your activity and notify your doctor. Returning to activities too soon can put you at risk for re-injury.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.