Diseases & Conditions
Tibial (Shinbone) Shaft Fractures
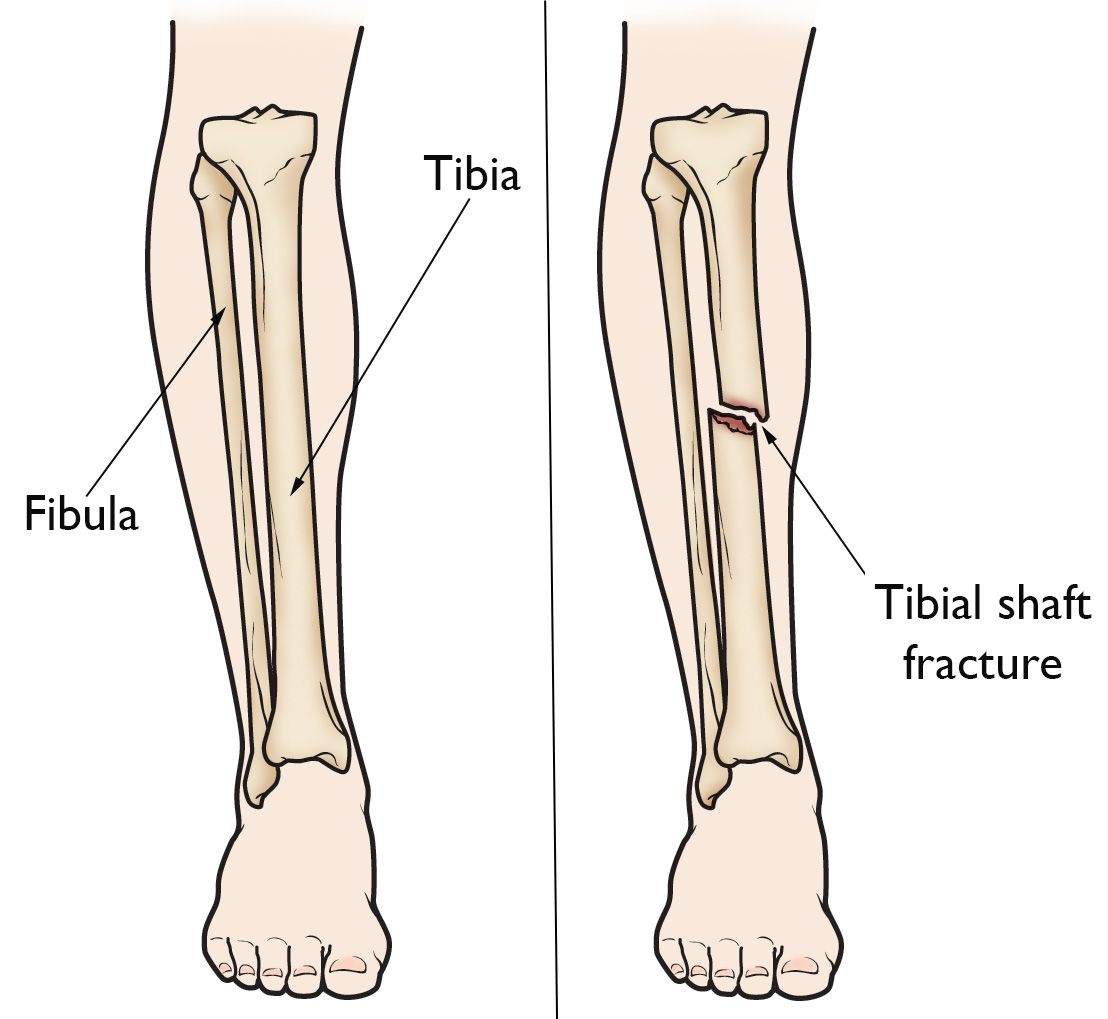
The tibia, or shinbone, is the most commonly fractured long bone in the body. A tibial shaft fracture occurs along the length of the bone, below the knee and above the ankle.
It typically takes a major force to cause this type of broken leg. Motor vehicle collisions, for example, are a common cause of tibial shaft fractures. In many tibia fractures, the smaller bone in the lower leg (fibula) is broken as well.
Anatomy
The lower leg is made up of two bones: the tibia and fibula. The tibia is the larger of the two bones. It supports most of your weight and is an important part of both the knee joint and ankle joint.
Types of Tibial Shaft Fractures
Tibia fractures vary greatly, depending on the force that causes the break:
- The pieces of bone may line up correctly (stable fracture) or they may be out of alignment (displaced fracture).
- The skin around the fracture may be intact (closed fracture) or the bone may puncture the skin (open fracture).
- Often, the fibula is broken as well.
Doctors describe fractures to each other using classification systems. Tibia fractures are classified depending on:
- The location of the fracture (the tibial shaft is divided into thirds: distal, middle, and proximal)
- The pattern of the fracture (for example, the bone can break in different directions, such as crosswise, lengthwise, or in the middle)
- Whether the skin and muscle over the bone is torn by the injury (open fracture)
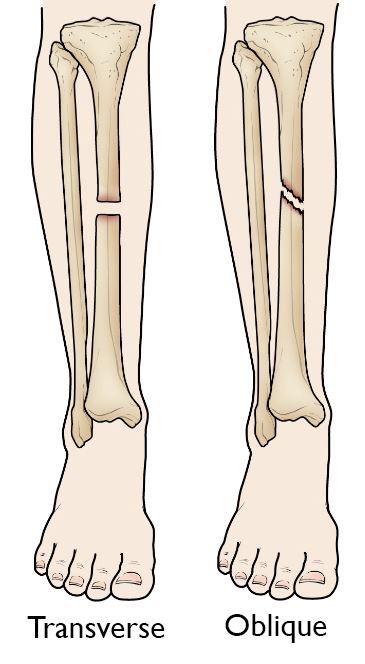
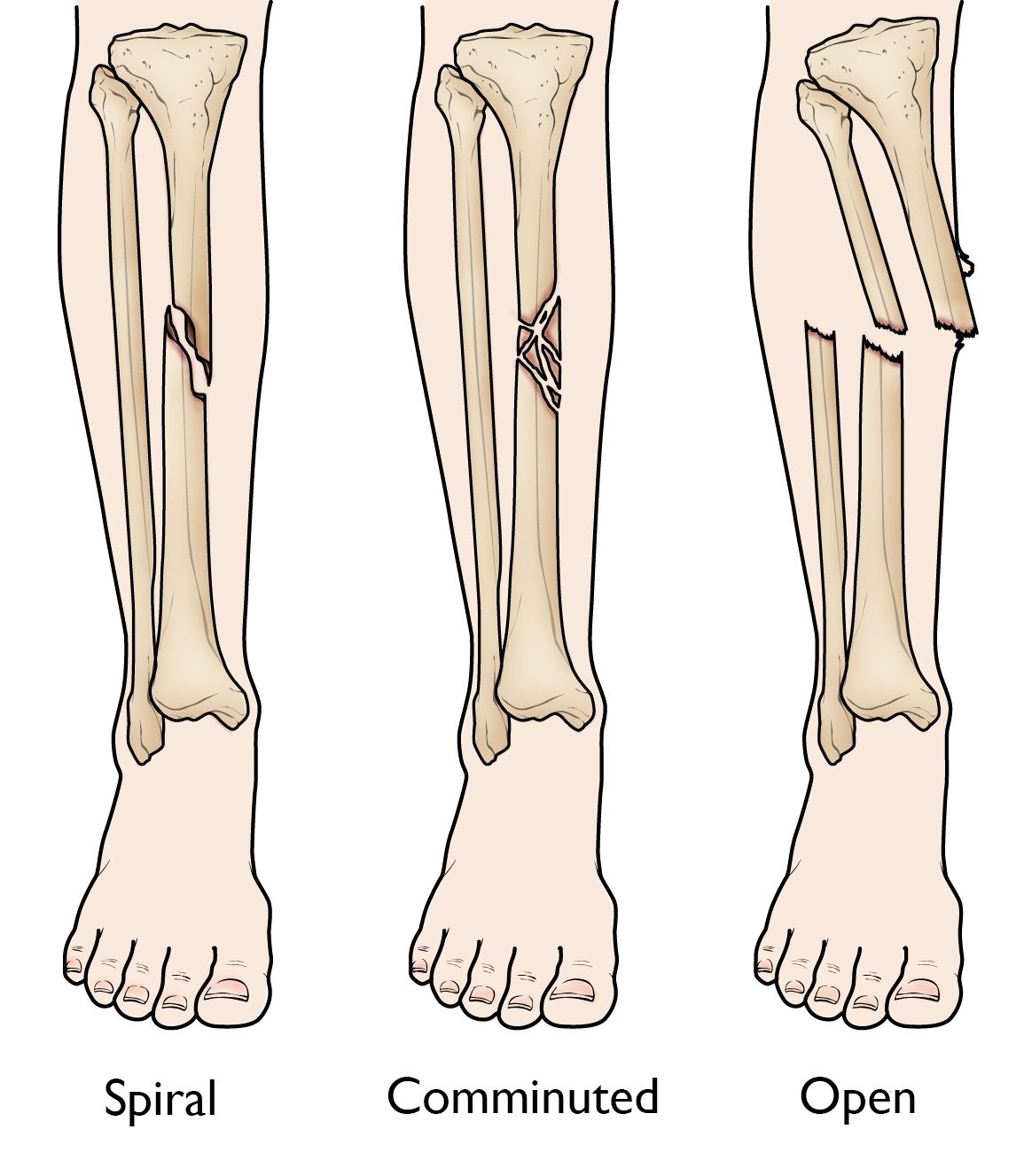
The most common types of tibial shaft fractures include:
- Transverse fracture: In this type of fracture, the break is a straight horizontal line going across the tibial shaft.
- Oblique fracture: This type of fracture has an angled line across the shaft.
- Spiral fracture: The fracture line encircles the shaft like the stripes on a candy cane. This type of fracture is caused by a twisting force.
- Comminuted fracture: In this type of fracture, the bone breaks into three or more pieces.
- Open fracture: If a bone breaks in such a way that bone fragments stick out through the skin or a wound penetrates (reaches) down to the broken bone, the fracture is called an open or compound fracture. Open fractures often involve much more damage to the surrounding muscles, tendons, and ligaments. They have a higher risk for complications — especially infections — and take a longer time to heal.
Cause
Tibial shaft fractures are often caused by some type of high-energy collision, such as a motor vehicle or motorcycle crash. In cases like these, the bone can be broken into several pieces (comminuted fracture).
Sports injuries, such as a fall while skiing or a collision with another player during soccer, are lower-energy injuries that can cause tibial shaft fractures. These fractures are typically caused by a twisting force and result in an oblique or spiral fracture.
Symptoms
A tibial shaft fracture usually causes immediate, severe pain. Other symptoms may include:
- Inability to walk or bear weight on the leg
- Deformity or instability of the leg
- Bone "tenting" over the skin at the fracture site or bone protruding through a break in the skin
- Occasional loss of feeling in the foot
Doctor Examination
Medical History and Physical Examination
It is important that your doctor knows the specifics of how you hurt your leg. For example, if you were in a car accident, it would help your doctor to know:
- How fast you were going
- Whether you were the driver or the passenger
- Whether you were wearing your seatbelt
- Whether the airbags went off
This information will help your doctor determine how you were hurt and whether you may be hurt somewhere else.
It is also important for your doctor to know if you have any other health conditions like:
- Allergies
- Asthma
- Diabetes
- High blood pressure
Your doctor will also ask you if you use tobacco products or are taking any medications.
After discussing your injury and medical history, your doctor will perform a careful examination. They will assess your overall condition and then focus on your leg. Your doctor will look for:
- An obvious deformity of the tibia/leg (an unusual angle, twisting, or shortening of the leg)
- Breaks in the skin
- Bruises
- Swelling
- Bony pieces that may be pushing on the skin
- Instability (some patients may retain a degree of stability if the fibula is not broken or if the fracture is incomplete)
After the visual inspection, your doctor will feel along your tibia, leg, and foot looking for abnormalities. If you are awake and alert, your doctor will test for sensation and movement in your leg and foot.
Imaging Tests
Imaging tests will provide your doctor with more information about your injury.
X-rays. The most common way to evaluate a fracture is with X-rays, which provide clear images of dense structures like bones. X-rays can:
- Show whether the tibia is broken or intact
- Show the type of fracture and where it is located within the tibia
- Help identify the involvement of the knee or ankle joints
- Show whether there is also a fibula fracture
Computed tomography (CT) scans. If your doctor still needs more information after reviewing your X-rays, they may order a CT scan.
A CT scan shows a cross-sectional image of your limb. It can provide your doctor with valuable information about the severity of the fracture or, in some cases, detect subtle fractures. For example, sometimes the fracture lines can be very thin and hard to see on an X-ray. A CT scan can help your doctor see the lines more clearly.
Treatment
In planning your treatment, your doctor will consider several things, including:
- Your overall health
- The cause of your injury
- The severity of your injury
- The extent of soft tissue damage
Nonsurgical Treatment
Nonsurgical treatment may be recommended for patients who:
- Are poor candidates for surgery due to their overall health problems
- Are less active, so they are better able to tolerate bones that are not perfectly aigned or differences in leg length
- Have closed fractures with minimal (very little) movement of the fracture ends
Initial treatment. Most injuries cause some swelling for the first few weeks. Your doctor may initially apply a splint to provide comfort and support. Unlike a full cast, a splint can be tightened or loosened to allow swelling to occur safely. Once the swelling goes down, your doctor will consider a range of treatment options.
Casting and bracing. Your doctor may immobilize the fracture in a cast for initial healing. After several weeks, the cast can be replaced with a functional brace made of plastic and fasteners. The brace will provide protection and support until healing is complete. The brace can be taken off for hygiene purposes (such as showering or bathing) and for physical therapy.
Surgical Treatment
Surgery may be recommended for certain types of fractures, including:
- Open fractures with wounds that need monitoring
- Fractures that have not healed with nonsurgical treatment
- Fractures with many bone fragments for which the bones are out of position
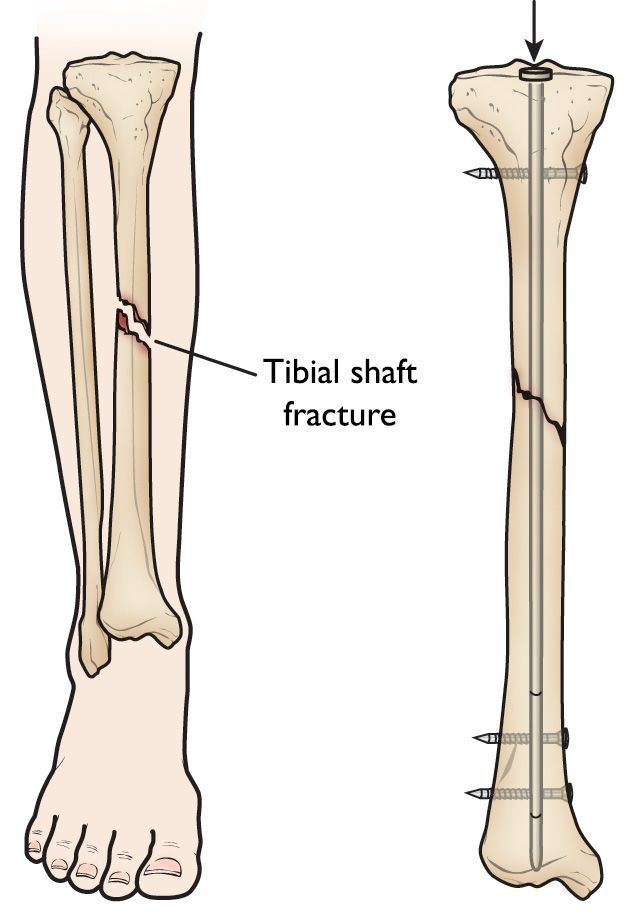
Intramedullary nailing. Currently, the method most surgeons use for treating tibia fractures is intramedullary nailing. During this procedure, a specially designed metal rod (nail) is inserted inside the tibia. The nail passes across the fracture to keep it in position.
Screws are used to stabilize the nail at both ends (top and bottom). This keeps the nail and the bone in proper position during healing.
Intramedullary nails are usually made of titanium. They come in various lengths and diameters to fit most tibia bones.
Intramedullary nailing is not ideal for fractures in children and adolescents because care must be taken to avoid crossing the bone's growth plates.
Plates and screws. During this operation, the bone fragments are first repositioned (reduced) into their normal alignment. They are held together with screws and metal plates attached to the outer surface of the bone.
Plates and screws are often used when intramedullary nailing may not be possible, such as for fractures that extend into either the knee or ankle joints.
External fixation. In this type of operation, metal pins or screws are placed into the bone above and below the fracture site. The pins and screws are attached to a bar outside the skin. This device is a stabilizing frame that holds the bones in the proper position so they can heal.
Recovery
Most tibial shaft fractures take 4 to 6 months to heal completely. Some take even longer, especially if the fracture was open or broken into several pieces or if the patients uses tobacco products.
Pain Management
Pain after an injury or surgery is a natural part of the healing process. Your doctor and nurses will work to reduce your pain, which can help you recover faster.
Medications are often prescribed for short-term pain relief after surgery or an injury. Many types of medicines are available to help manage pain. These include:
- Acetaminophen
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Gabapentinoids
- Muscle relaxers
- Opioids
- Topical pain medications
Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids. Some pain medications may have side effects that can impact your ability to drive and do other activities. Your doctor will talk to you about the side effects of your medications.
Opioids can provide excellent pain relief; however, their use has risks and complications. These medications can be addictive and potentially dangerous. It is therefore important to use opioids only as directed by your doctor, to use as little as possible for as short a time as possible, and to stop taking them as soon as your pain starts to improve. Tell your doctor if your pain has not begun to improve within a few days after surgery.
Weightbearing
Many doctors encourage leg motion early in the recovery period. It is very important to follow your doctor's instructions for putting weight on your injured leg to avoid problems.
In some cases, doctors will allow patients to put as much weight as possible on the leg right after surgery. However, you may not be able to put full weight on your leg until the fracture has started to heal. Be sure to follow your doctor's instructions carefully.
When you begin walking, you will probably need to use crutches or a walker for support.
Physical Therapy
Because you will likely lose muscle strength in the injured area, exercises during the healing process are important. Physical therapy will help to restore normal muscle strength, joint motion, and flexibility. It can also help you manage your pain after surgery.
A physical therapist will most likely begin teaching you specific exercises while you are still in the hospital. The therapist will also help you learn how to use crutches or a walker.
Complications
Complications from Tibial Shaft Fractures
Tibial shaft fractures can cause further injury and complications, including the following:
- The ends of broken bones are often sharp and can cut or tear surrounding muscles, nerves, or blood vessels.
- Acute compartment syndrome may develop. This is a painful condition that occurs when pressure within the muscles builds to dangerous levels. This pressure can decrease blood flow, which prevents nourishment and oxygen from reaching nerve and muscle cells. This is a surgical emergency. Unless the pressure is relieved quickly, permanent disability may result. During the procedure, your surgeon makes incisions in your skin and the muscle coverings to relieve pressure.
- Open fractures expose the bone to the outside environment. Even with good surgical cleaning of the bone and muscle, the bone can become infected. Bone infection is difficult to treat and often requires multiple surgeries and long-term antibiotics.
Complications from Surgery
In addition to the risks of surgery in general, such as blood loss and problems related to anesthesia, complications of surgery may include:
- Infection
- Injury to nerves and blood vessels
- Blood clots (these may also occur without surgery)
- Malalignment or the inability to correctly position the broken fragments
- Delayed union or nonunion (when the fracture heals slower than usual or not at all)
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.