Diseases & Conditions
Sternoclavicular (SC) Joint Disorders
This article was written and/or reviewed by a member of American Shoulder and Elbow Surgeons (ASES).
The sternoclavicular (SC) joint is one of the four joints that make up the shoulder. The joint is located in the spot where the clavicle (collarbone) meets the sternum (breastbone) at the base of the neck. Although not common, problems with the SC joint can arise from injury and other disorders.
- Injuries to the SC joint typically result from high-energy injuries, such as motor vehicle collisions, or contact sports like football. While these injuries can be painful, most are relatively minor and will heal well without surgery.
- Very rarely, a hard blow to the shoulder with an injury to the SC joint can damage the vital organs and tissues that lie nearby, such as the main blood vessels from the heart, the trachea (windpipe), and the esophagus (tube that connects the throat to the stomach). When this occurs, it is a serious injury that requires immediate medical attention.
- The SC joint can also be damaged over time, as the protective tissue that covers the ends of the bones gradually wears away. This is a type of arthritis that can lead to pain, stiffness, and reduced motion in the shoulder and arm.
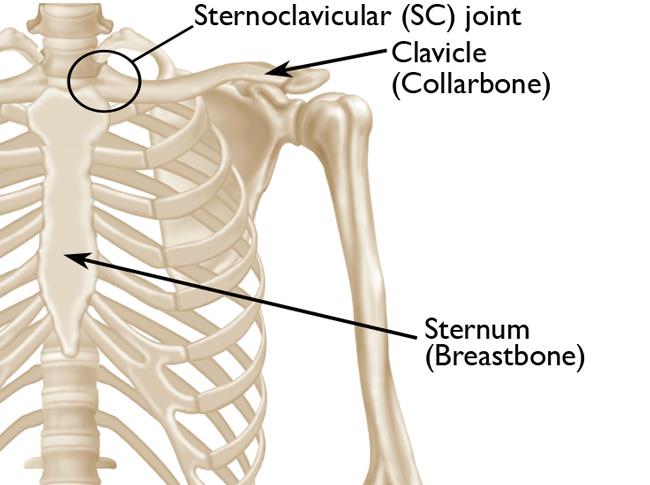
Anatomy
The sternoclavicular (SC) joint is the link between the clavicle (collarbone) and the sternum (breastbone). The SC joint supports the shoulder and is the only joint that connects the arm to the body.
Like the other joints in the body, the SC joint is covered with a smooth, slippery substance called articular cartilage. This cartilage helps the bones glide easily along each other as you move your arm and shoulder. Tough bands of connective tissue called ligaments surround the SC joint, giving it strength and stability.
Immediately behind the SC joint lie several important nerves and blood vessels, as well as other vital structures like the trachea (windpipe) and esophagus (tube that connects the throat to the stomach).
Description
Injuries and osteoarthritis are the most common disorders associated with the SC joint.
Injuries (Sprains, Fractures, and Dislocations)
Injuries to the SC joint can range from a mild sprain, in which the surrounding ligaments are stretched (the most commonly seen injury), to a fracture of the clavicle (collarbone) itself.
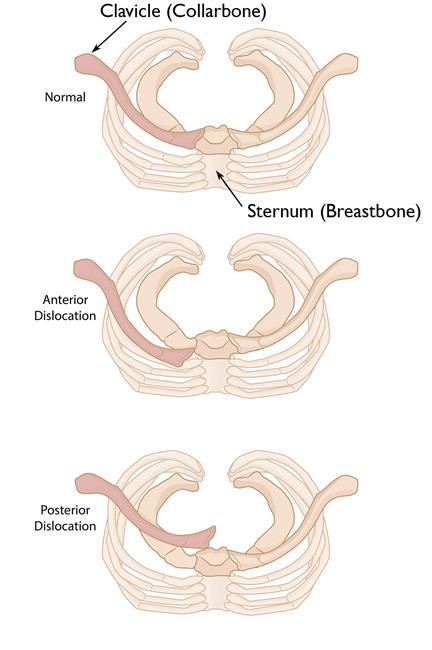
In rare cases, a strong blow to the shoulder can cause an injury in which the joint dislocates completely from its normal position. Joint dislocations are classified as either "anterior" (forward) or "posterior" (backward), depending on which direction the collarbone moves:
- Anterior — the end of the clavicle is pushed forward, in front of the sternum (breastbone)
- Posterior —the end of the clavicle is pushed backward, behind the sternum and deep into the upper chest
Although both kinds of dislocations are serious injuries, a posterior dislocation requires more urgent medical attention. In a posterior dislocation, the vital structures behind the SC joint can be compressed (squeezed), leading to life-threatening problems with breathing, choking, or blood flow from the heart to your arms or brain.
Causes of injury. The ligaments surrounding the SC joint are some of the strongest in the body, so it takes a great deal of force to cause an injury. Typically, injuries to the joint are caused by some type of high-impact event, such as a:
- Collision or hard fall during a contact sport like football or rugby
- Motor vehicle collision
Because of the significant force needed to cause an injury, patients may have additional injuries to the chest, airways, and extremities (arms and legs). In some cases, injury to the SC joint is overlooked at first because these other injuries require urgent attention.
Osteoarthritis
Osteoarthritis is a degenerative wear and tear type of arthritis that occurs most often in people 50 years of age or older, although it may occur in younger people, too.
In osteoarthritis, the smooth articular cartilage that covers the SC joint gradually wears away. As the cartilage wears away, it becomes frayed and rough, and the protective space between the bones decreases. This can result in pain from bone rubbing on bone and can also lead to the formation of a bone spur around the joint that can appear and feel prominent (like it is bulging or sticking out).
Osteoarthritis develops slowly, and the pain and stiffness it causes get worse and worse over time.
Other Disorders
Other disorders associated with the SC joint include:
- Inflammatory conditions, such as rheumatoid arthritis
- Infection
In addition, some patients may experience slight movement or popping of the bone out of place even without some type of trauma. This condition is called subluxation and seems to be limited to those people who are considered "loose jointed."
Symptoms
The most common symptom of an SC joint disorder is pain in the area where the clavicle meets the sternum. This pain will be present with a sprain or arthritis but will be much sharper in the case of a fracture or dislocation — especially when you try to move your arm.
These are some other common signs and symptoms:
- You may have swelling, bruising, or tenderness over the joint.
- You may hear/feel a crunching or grinding sound (crepitus) when you try to move your arm.
- You may have limited range of motion of the arm and shoulder.
- With an inflammatory condition, such as rheumatoid arthritis, you may have simultaneous (at the same time) pain in other joints in your body.
- With a joint infection, there may be redness over the joint and you may have fever, chills, or night sweats. If you experience any of the symptoms of a joint infection, it is important to seek medical attention right away.
Doctor Examination
Physical Examination
Your doctor will:
- Talk with you about your medical history and general health
- Ask about your symptoms, including when your pain began
- Ask whether there is a history of injury or accident
- Look for visible signs of deformity or a bump over the joint.
- Perform a careful examination of your shoulder area to:
- Look for swelling, bruising, or redness over the joint
- Measure range of motion of your arm
- Palpate (feel) the clavicle and joint to see if it is painful or tender to the touch, if it moves easily, or if it is warm/hot to the touch, which may indicate an inflammatory arthritis or infection
- Check your pulse at the wrist and elbow to ensure there is good blood flow to your hand and fingers
- Check the sensation in your arm, hand, and fingers to ensure the nerves to your arm are not compressed (being squeezed)
Imaging Tests
X-rays. X-rays provide images of dense structures, such as bone. Your doctor will order X-rays of your chest and shoulder from a number of different angles to help confirm the diagnosis and rule out other underlying (contributing) shoulder conditions.
Computerized tomography (CT) scan. This imaging study is more detailed than a plain X-ray. Your doctor may order a CT scan to better evaluate your injury and to help differentiate a sprain from a dislocation or a fracture.
Other imaging tests. Depending on your specific problem, your doctor may order additional imaging tests, such as a magnetic resonance imaging (MRI) scan or bone scan.
Treatment
Nonsurgical Treatment
In most cases, disorders of the SC joint can be treated without surgery. Nonsurgical treatment may include:
Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, can help reduce pain and swelling in the joint.
If you have osteoarthritis or an inflammatory condition, your doctor may also recommend strong anti-inflammatory agents called corticosteroids, which are injected directly into the joint. Corticosteroids can provide temporary relief of pain and swelling. Learn more: Cortisone Shot (Steroid Injection)
Immobilization. If you have an injury, your doctor may recommend that you wear a shoulder sling to restrict arm movement and allow for healing. The length of time you will need to wear the sling depends on the type of your injury and how serious it is.
Activity modification. The doctor may recommend that patients with SC joint osteoarthritis avoid the activities that bring on painful symptoms.
For patients who experience nontraumatic dislocation of the joint (subluxation), the doctor may also recommend avoiding the activities that make the joint "pop."
Closed reduction. If you have a joint dislocation, your doctor may try to manipulate (move) the clavicle back into place without making an incision in the skin (see photo below). This procedure is called a closed reduction. A closed reduction is usually performed in the operating room. You may be given either general anesthesia or a muscle relaxant with mild sedation.
Some anterior (forward) dislocations can "pop" back out after closed reduction. If this is not recognized until several days or even months after the injury, the anterior dislocation is left alone and most patients report no pain and normal shoulder function — although there may be a deformity or bump over the joint.
Because a posterior (backward) dislocation can compress (squeeze) the vital structures behind the joint, it usually requires urgent reduction. Getting the joint back into the proper position is important. During closed reduction for a posterior dislocation, a thoracic surgeon may be on hand to address potential complications involving the structures in the chest.
Surgical Treatment
Open reduction. In some cases, closed reduction for an anterior or posterior dislocation is not successful. In this situation, your doctor may need to perform an open reduction of the SC joint.
To do this, the surgeon will make an incision and put the joint back in place under direct vision (direct vision means the surgeon can clearly see the joint through the open incision).
In rare cases, the SC joint may dislocate repeatedly (again and again) after reduction. These patients may require reconstructive surgery to stabilize the joint. A reduction means using a tendon from a tissue bank (called an allograft) or from your own body (called an autograft) to rebuild the ligaments that are injured and prevent the joint from dislocating again.
Surgery for osteoarthritis can also be performed, although it is rarely required. If your pain and stiffness cannot be managed with nonsurgical treatment, however, your doctor may perform a procedure to remove bone from the arthritic and painful end of the clavicle. This will allow more space for movement and prevent the rough bone ends from rubbing against each other (which causes pain).
Other procedures. For patients with an infection in the SC joint, an immediate operation is usually required to open the joint and drain the infection. This will be followed by a course of antibiotics.
Recovery
After a fracture or dislocation of the SC joint, your arm may be immobilized (held still) in a sling for a period of about 6 weeks, or sometimes longer.
Even when the sling is removed, you will still have restrictions on lifting. For example, you may be restricted from lifting anything more than a glass of water (or another type of drink) for up to several months. These restrictions hold true after surgery as well. Immobilizing and not using your arm allow the healing process to take place.
As your recovery progresses (moves along), specific exercises will help restore movement and strengthen your shoulder. Your doctor may provide you with a home therapy plan or recommend that you work with a physical therapist.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.