Diseases & Conditions
Osteonecrosis of the Knee
Osteonecrosis of the knee (also known as avascular necrosis) is a painful condition that occurs when the blood supply to a section of bone in the femur (thighbone) or tibia (shinbone) is disrupted. Because bone cells need a steady supply of blood to stay healthy, osteonecrosis can ultimately lead to destruction of the knee joint and severe arthritis.
When osteonecrosis is diagnosed early, treatment may involve taking medications to relieve pain or limiting use of the affected knee. More advanced osteonecrosis, however, almost always requires surgery to prevent further damage to the bone and improve joint function.
Anatomy
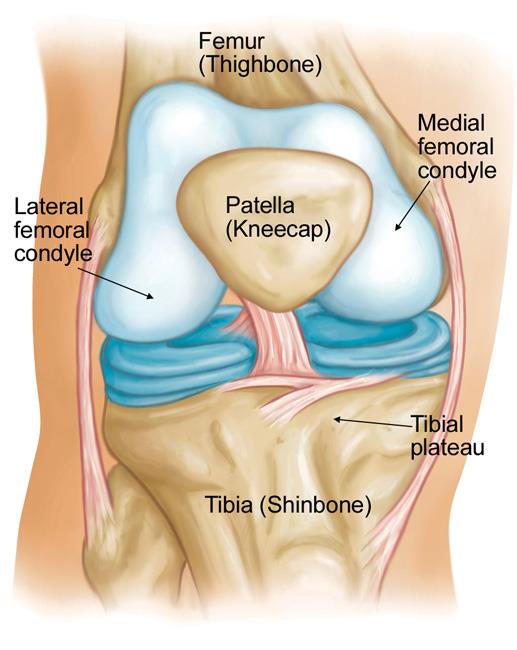
Your knee is the largest and strongest joint in your body. It is made up of the lower end of the femur (thighbone), the upper end of the tibia (shinbone), and the patella (kneecap). The ends of these three bones where they touch are covered with articular cartilage, a smooth, slippery substance that protects the bones and enables them to glide easily against each other as you move your leg.
Osteonecrosis of the knee most often occurs on the inside of the knee (medial femoral condyle). However, it may also occur on the outside of the knee (lateral femoral condyle) or on the flat top of the shinbone (tibial plateau).
Cause
Osteonecrosis develops when the blood supply to a segment of bone is disrupted. Without adequate nourishment, the affected portion of bone dies and gradually collapses. As a result, the articular cartilage covering the bone also collapses, leading to disabling arthritis.
Osteonecrosis of the knee can affect anyone, but it is more common in people over the age of 60. Woman are three times more likely than men to develop the condition.
Risk Factors
It is not always known what causes the lack of blood supply, but doctors have identified a number of risk factors that make someone more likely to develop osteonecrosis.
- Injury. A knee injury — such as a stress fracture or dislocation—combined with some type of trauma to the knee, can damage blood vessels and reduce blood flow to the affected bone.
- Oral corticosteroid medications. Many diseases, such as asthma and rheumatoid arthritis, are treated with oral steroid medications. Although it is not known exactly why these medications can lead to osteonecrosis, research shows that there is a connection between the disease and long-term steroid use. Steroid-induced osteonecrosis frequently affects multiple joints in the body.
- Medical conditions. Osteonecrosis of the knee is associated with medical conditions, such as obesity, sickle cell anemia, and lupus. Osteonecrosis is also commonly seen in patients with HIV due to the medications used for HIV treatment.
- Transplants. Organ transplantation, especially kidney transplant, is associated with osteonecrosis.
- Excessive alcohol use. Overconsumption of alcohol over time can cause fatty deposits to form in the blood vessels as well as elevated cortisone levels, resulting in a decreased blood supply to the bone.
Regardless of the cause, if osteonecrosis is not identified and treated early, it can develop into severe osteoarthritis.
Symptoms
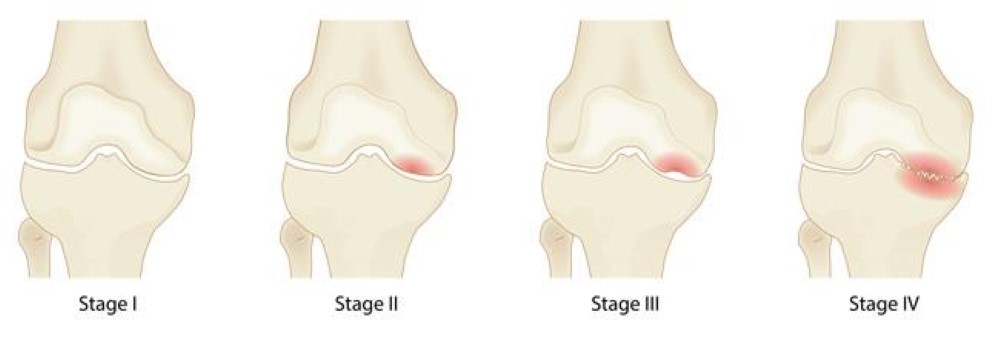
Osteonecrosis develops in stages.
- The first symptom is typically pain on the inside of the knee. This pain may occur suddenly and be triggered by a specific activity or minor injury.
- As the disease progresses, it becomes more difficult to stand and put weight on the affected knee, and moving the knee joint is painful.
Other symptoms may include:
- Swelling over the front and inside of the knee
- Sensitivity to touch around the knee
- Limited range of motion in the joint
It may take several months to more than a year for the disease to progress. It is important to diagnose osteonecrosis early, because some studies show that early treatment is associated with better outcomes.
Doctor Examination
Physical Examination
Your doctor will talk with you about your general health and medical history and ask you to describe your symptoms. They will then perform a careful examination of your knee, looking for:
- Joint swelling, warmth, or redness
- Tenderness
- Range of passive (assisted) and active (self-directed) motion
- Instability of the joint
- Pain when weight is placed on the knee
- Any signs of injury to the muscles, tendons, and ligaments surrounding the knee
Imaging tests will help your doctor confirm the diagnosis.
Imaging Tests
X-rays. X-rays provide images of dense structures, such as bone. Your doctor may order X-rays to look for changes that occur in bone in the later stages of osteonecrosis. In the early stages of the disease, X-rays usually appear normal.
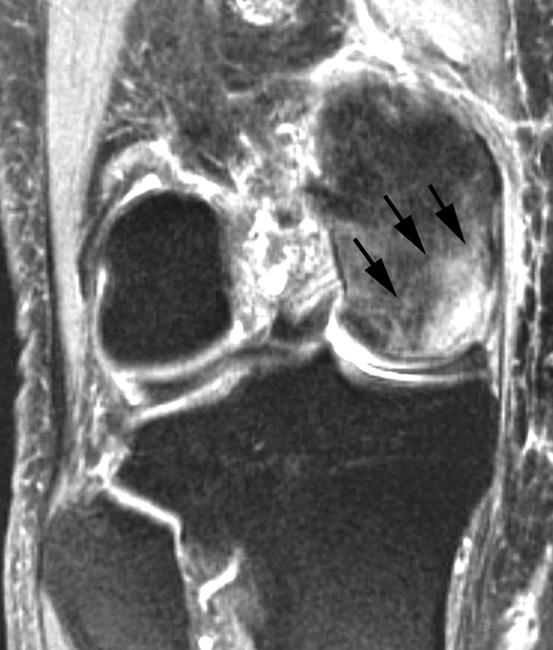
Magnetic resonance imaging (MRI) scans. Early changes in the bone that may not show up on an X-ray can be detected on an MRI.
- MRI scans are used to evaluate how much of the bone has been affected by the disease.
- An MRI scan may also show early osteonecrosis that has yet to cause symptoms — for example osteonecrosis that may be developing in the opposite knee joint.
Bone scan. In some cases, the doctor may order a bone scan. During this test, a very small amount of radioactive dye is injected into your vein. Osteonecrosis may cause an increased uptake of the radioactive material in the bone due to bone activity.
Treatment
Treatment for osteonecrosis depends on a number of factors, including:
- The stage of the disease
- The amount of bone affected
- The underlying cause of the disease
Nonsurgical Treatment
In the early stages of osteonecrosis, treatment is nonsurgical. If the affected area of the knee is small, nonsurgical treatment may be all that is needed.
Nonsurgical treatment may include:
- Medications
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, can help reduce pain and swelling in your knee.
- Your doctor may also talk to you about bisphosphonates for treatment, especially if you are at a younger age when you are diagnosed.
- Reduced weightbearing. For some patients, removing weight from the affected knee can slow the damage caused by osteonecrosis and allow healing. Your doctor may recommend using crutches for a period of time to take weight off your knee. In some cases, wearing an "unloader" brace can help relieve pressure on the joint surface by shifting weight away from the affected portion of the knee.
- Exercise. Your doctor or a physical therapist may provide you with an exercise program designed to help strengthen your thigh muscles and maintain range of motion in the affected joint. In some cases, water exercise may be recommended to avoid stress on your knee joint.
- Activity modification. Your doctor may recommend that you avoid certain activities that bring on painful symptoms.
Surgical Treatment
If a large portion of the bone surface is affected, or if your pain does not improve with nonsurgical treatment, your doctor may recommend surgery. There are several different procedures used to treat osteonecrosis of the knee.
Arthroscopic debridement and microfracture. In debridement (cleansing), your doctor uses a small camera and miniature surgical instruments to remove loose bits of bone or damaged cartilage from inside the joint space. For small lesions, the surgeon may also drill multiple holes, or microfractures, in the underlying bone to help promote blood flow and induce a healing reaction
Core decompression. This procedure involves drilling one larger hole or several smaller holes into the bone to relieve pressure on the bone surface and create channels for new blood vessels to nourish the affected areas of the knee.
When osteonecrosis of the knee is diagnosed early, core decompression is often successful in preventing collapse of the bone and the development of arthritis.
Osteochondral (bone and cartilage) grafting. Core decompression is often combined with bone and cartilage grafting to help regenerate healthy bone and support cartilage at the knee joint. A bone graft is healthy bone tissue that is transplanted to an area of the body where it is needed. The tissue may be taken from a donor (allograft) or from another bone in your body (autograft).
There are also several synthetic bone grafts available today.
Autologous chondrocyte implantation (ACI). This is a two-stage procedure. In the first stage, your doctor performs an arthroscopic procedure to remove a small number of cartilage-producing cells (chondrocytes) from your knee. These chondrocytes are sent to a lab where they are cultured (multiplied) for up to 6 weeks to obtain more cells.
In the second stage, your doctor performs another procedure to implant the chondrocytes into the area of your knee with cartilage loss. The cells then grow in the joint, replacing the damaged cartilage with healthy cartilage.
Osteotomy. In an osteotomy, either the tibia (shinbone) or femur (thighbone) is cut and then reshaped. The surgeon will either remove a portion or bone or insert a wedge of bone graft or synthetic bone to help shift weight off the damaged area of your knee. Shifting your weight off the damaged side of the joint will help relieve pain and improve function.
Total knee replacement or unicompartmental (partial) knee replacement. If the disease has advanced to the point where the bone has already collapsed, you may need surgery to replace the damaged parts of your knee. In knee replacement, your doctor removes the damaged bone and cartilage, and then positions new metal or plastic joint surfaces to restore the function of your knee.
Outcome
For most patients, treatment for osteonecrosis is successful in relieving pain and improving function. Outcomes vary, however, depending on the stage of the disease at diagnosis and the type of treatment. Your doctor will talk with you about the expected outcome of treatment in your specific situation.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.