Diseases & Conditions
Osteonecrosis of the Hip
Osteonecrosis of the hip is a painful condition that occurs when the blood supply to the head of the femur (thighbone) is disrupted. Because bone cells need a steady supply of blood to stay healthy, osteonecrosis can ultimately lead to destruction of the hip joint and severe arthritis.
Osteonecrosis is also called avascular necrosis (AVN) or aseptic necrosis. Although it can occur in any bone, osteonecrosis most commonly affects the hip. More than 20,000 people each year enter hospitals for treatment of osteonecrosis of the hip. In many cases, both hips are affected by the disease.
Anatomy
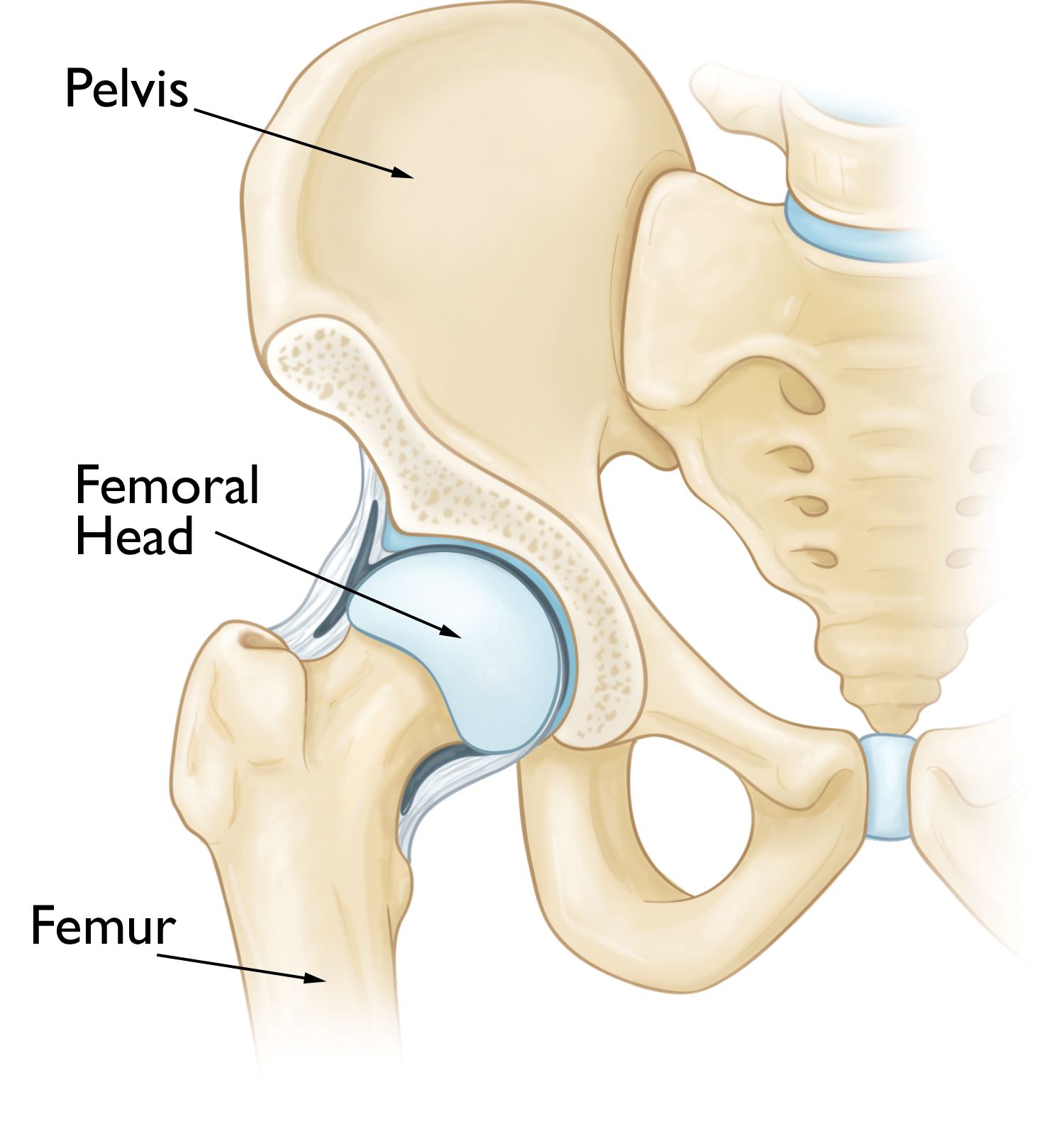
The hip is a ball-and-socket joint.
- The socket is formed by the acetabulum, which is part of the large pelvis bone.
- The ball is the femoral head, which is the upper end of the femur (thighbone).
The surface of the ball and socket is covered with articular cartilage, a smooth, slippery substance that protects the bones and enables them to glide easily across each other.
Cause
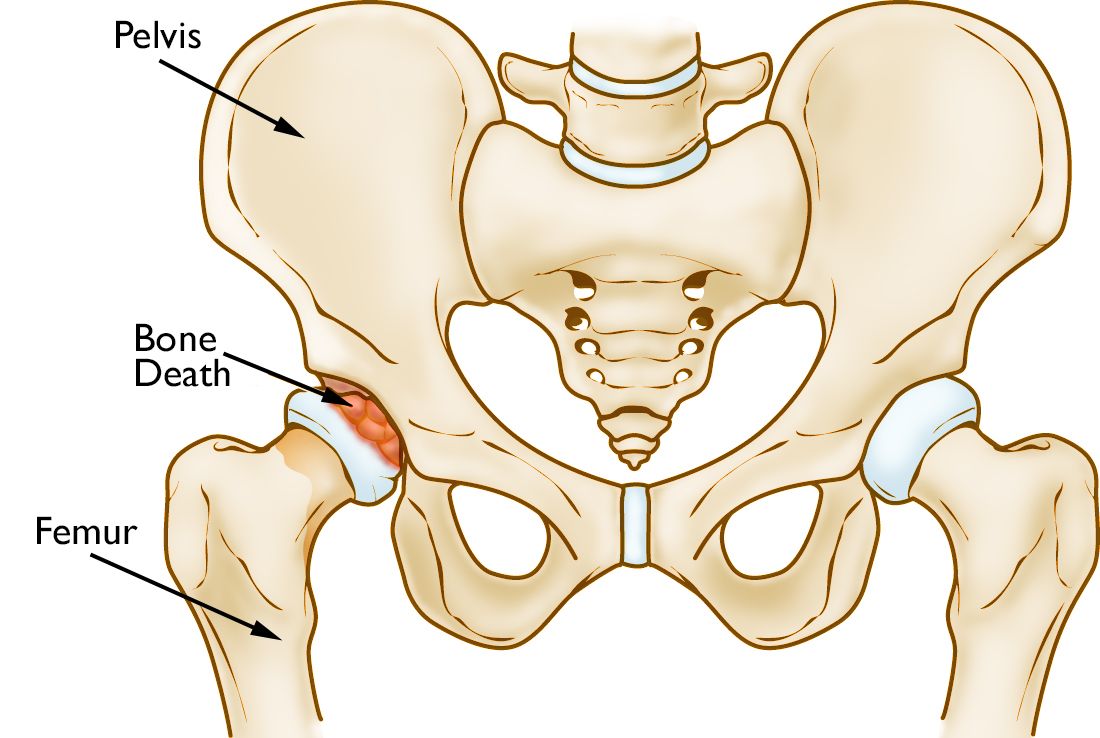
Osteonecrosis of the hip develops when the blood supply to the femoral head is disrupted. Without adequate nourishment, the bone in the head of the femur dies and gradually collapses. As a result, the articular cartilage covering the hip bones also collapses, leading to disabling arthritis.
Osteonecrosis can affect anyone, but it is more common in people between the ages of 40 and 65. Men develop osteonecrosis of the hip more often than women.
Risk Factors
It is not always known what causes the lack of blood supply, but doctors have identified a number of risk factors that can make someone more likely to develop osteonecrosis:
- Injury. Hip dislocations, hip fractures, and other injuries to the hip can damage the blood vessels and impair circulation to the femoral head.
- Excessive alcohol use. Overconsumption of alcohol over time can cause fatty deposits to form in the blood vessels and can elevate cortisone levels, resulting in a decreased blood supply to the bone.
- Corticosteroid medicines. Many diseases, including asthma, rheumatoid arthritis, and systemic lupus erythematosus, are treated with steroid medications. Although it is not known exactly why these medications can lead to osteonecrosis, research shows that there is a connection between the disease and long-term corticosteroid use.
- Medical conditions. Osteonecrosis is associated with other diseases, including Caisson disease (diver's disease, or "the bends"), sickle cell disease, myeloproliferative disorders, Gaucher's disease, systemic lupus erythematosus, Crohn's disease, arterial embolism, thrombosis, and vasculitis.
Symptoms
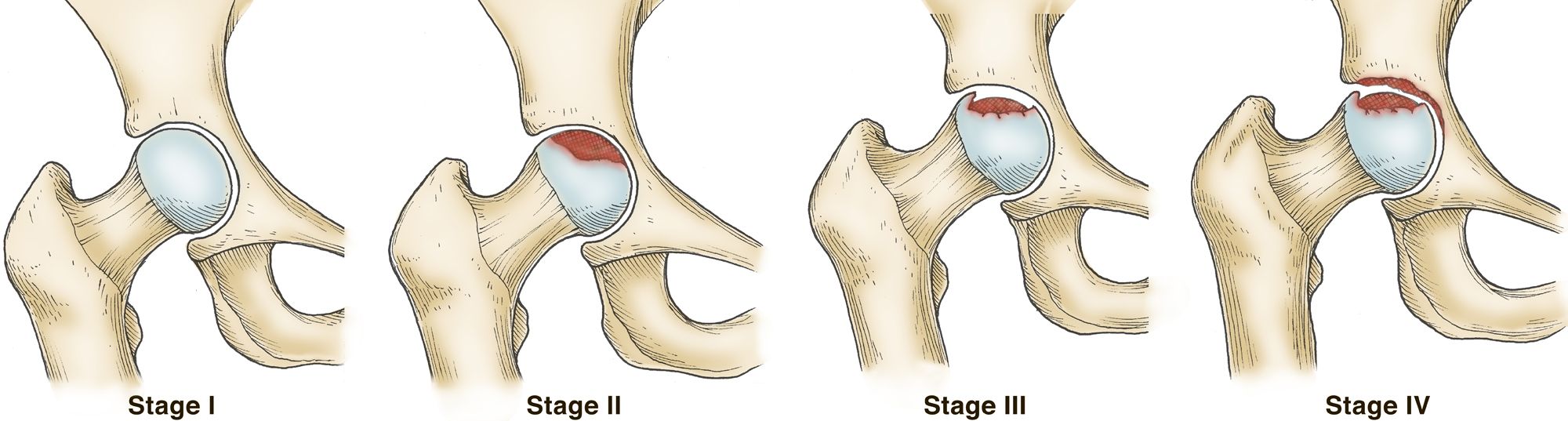
Osteonecrosis develops in stages. Hip pain is typically the first symptom. This may lead to a dull ache or throbbing pain in the groin or buttock area. As the disease progresses, it becomes more difficult to stand and put weight on the affected hip, and moving the hip joint is painful.
It may take from several months to over a year for the disease to progress. It is important to diagnose osteonecrosis early, because some studies show that early treatment is associated with better outcomes.
Doctor Examination
After discussing your symptoms and medical history, your doctor will examine your hip to discover which specific motions cause your pain.
Patients with osteonecrosis often have severe pain in the hip joint but relatively good range of motion. This is because only the femoral head is involved in the earlier stages of the disease. Later, as the surface of the femoral head collapses, the entire joint becomes arthritic. Loss of motion and stiffness can then develop.
Imaging Tests
Imaging studies will help your doctor confirm the diagnosis.
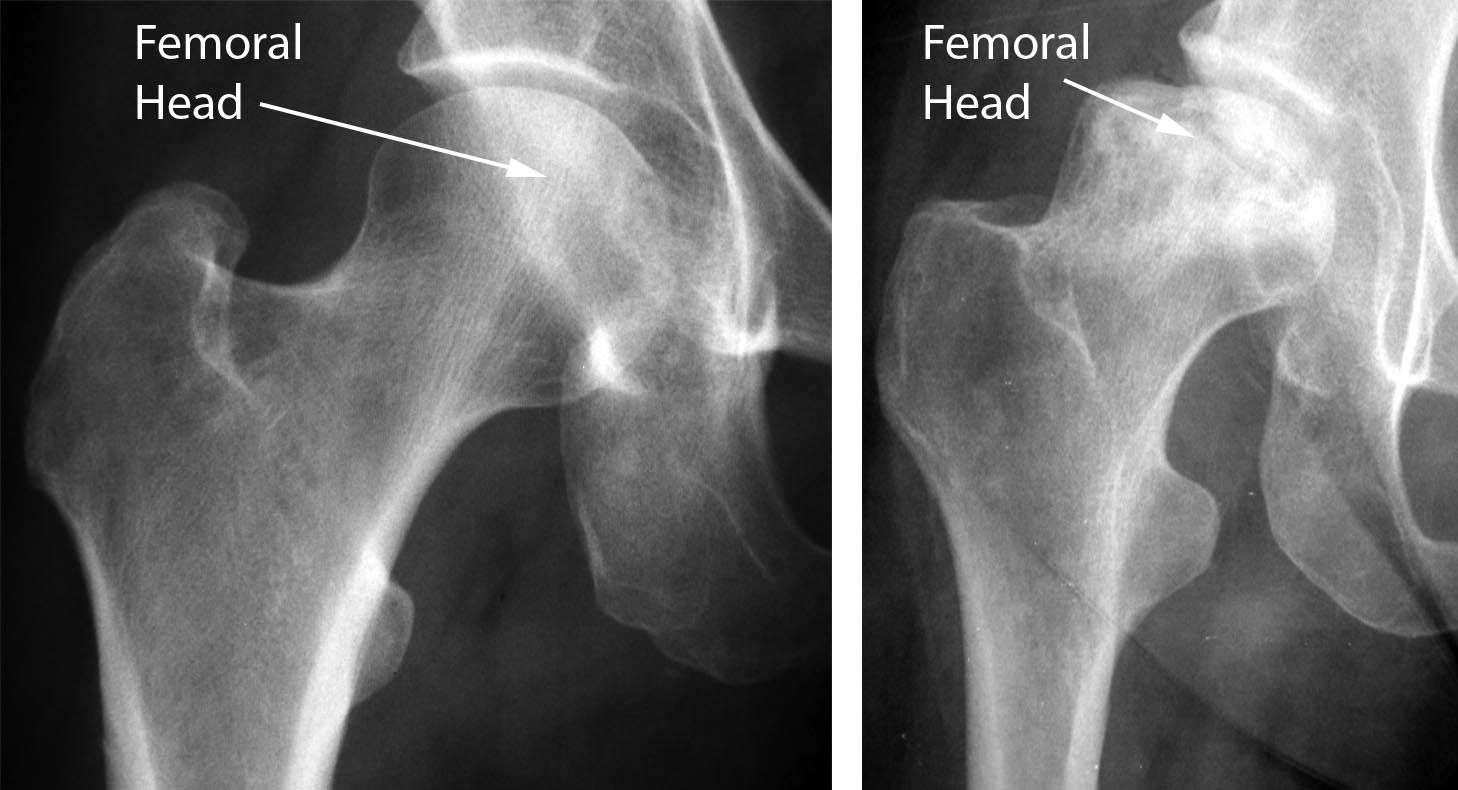
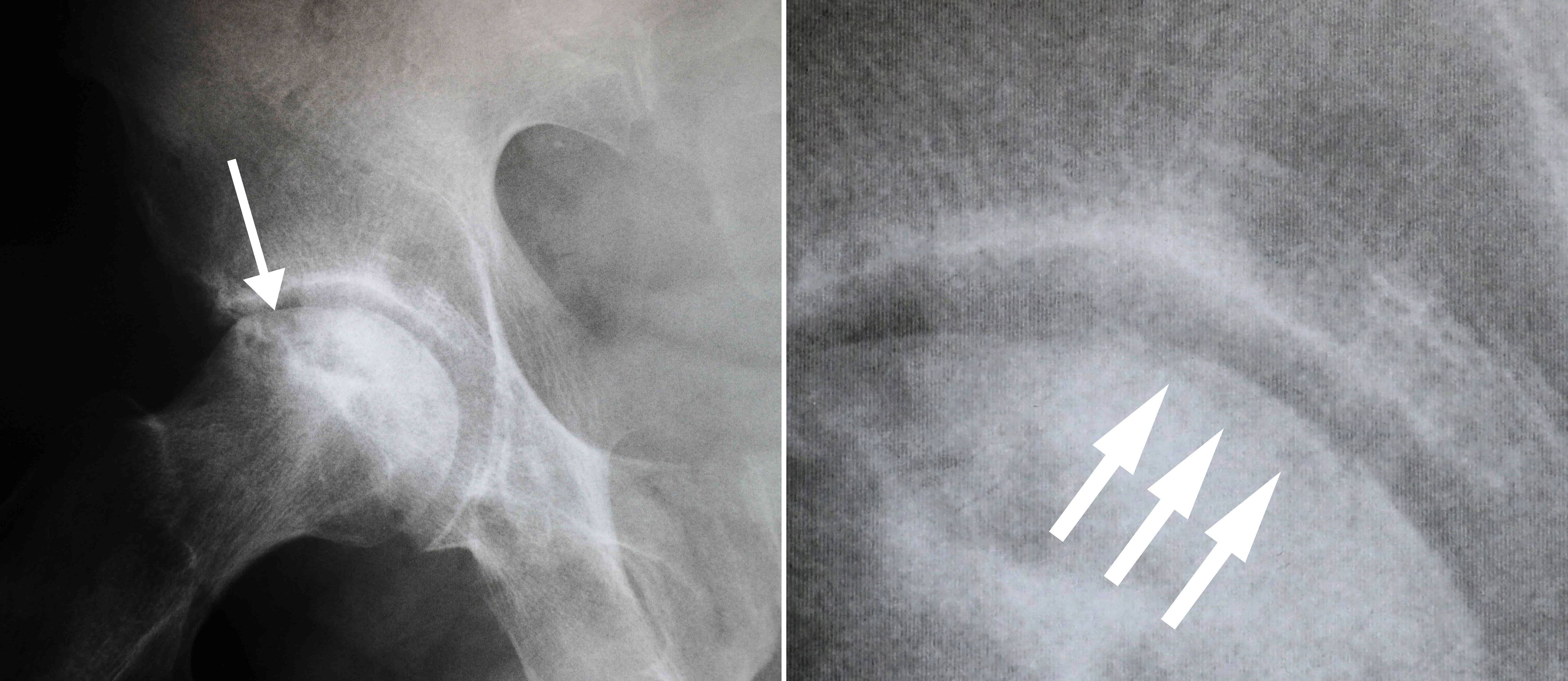
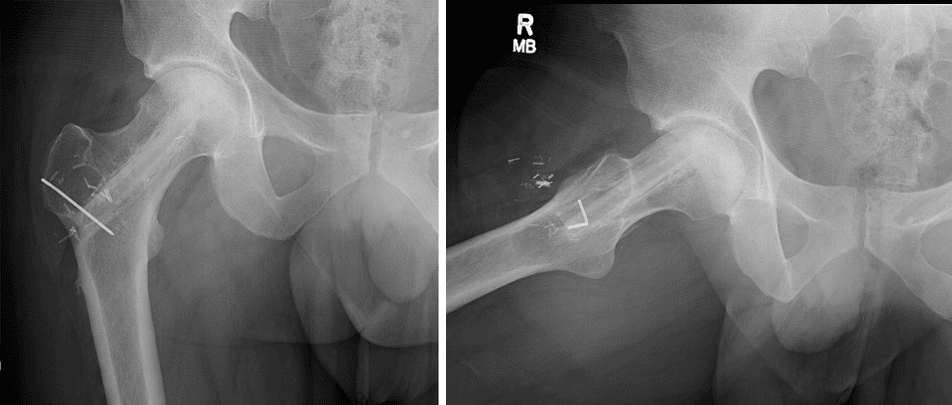
X-rays. X-rays provide images of dense structures, such as bone. X-rays are used to determine whether the bone in the femoral head has collapsed and to what degree.
Osteonecrosis is typically seen as a wedge-shaped area with a dense whitish sclerotic (hardened) border in the superior lateral portion of the femoral head. On the lateral view, a line called a “crescent sign” can often be seen just below the surface of the femoral head.
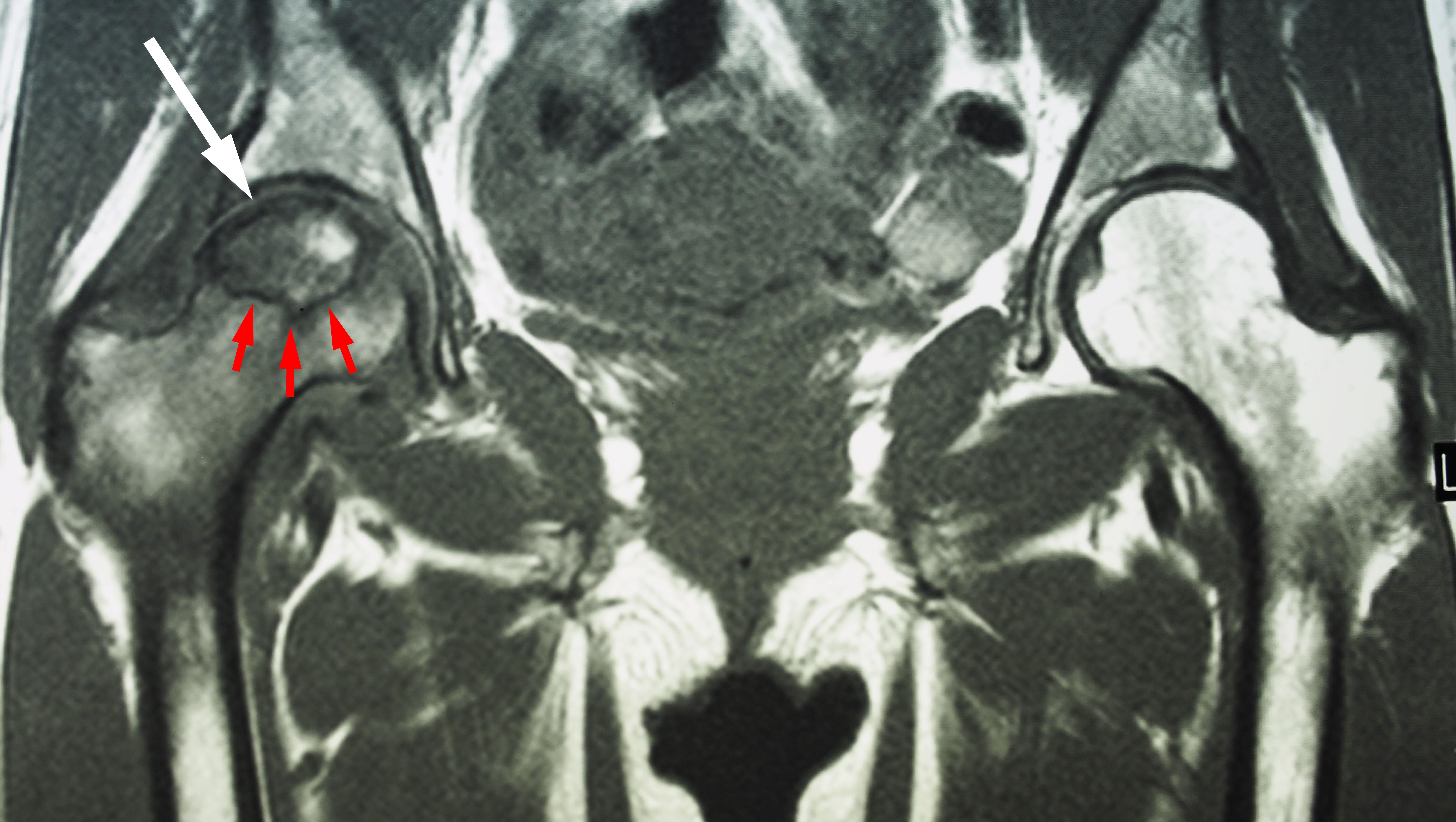
Magnetic resonance imaging (MRI) scans. Early changes in the bone that may not show up on an x-ray can be detected with an MRI scan. These scans are used to evaluate how much of the bone is affected by the disease. An MRI may also show early osteonecrosis that has yet to cause symptoms (for example — osteonecrosis that may be developing in the opposite hip joint).
Treatment
Although nonsurgical treatment options — such as anti-inflammatory medications, activity changes, and using crutches — can help relieve pain and slow the progression of the disease, the most successful treatment options are surgical. Patients with osteonecrosis that is caught in the very early stages (before the femoral head collapses) are potential candidates for hip-preserving procedures.
There are several different surgical procedures used to treat osteonecrosis of the hip.
Core Decompression and Grafting
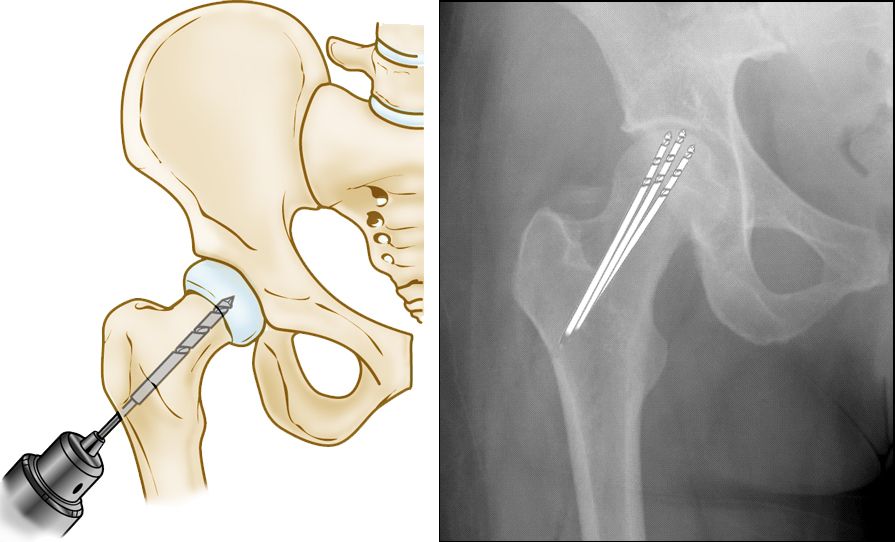
This procedure involves drilling one large hole or several smaller holes into the femoral head to relieve pressure in the bone and create channels for new blood vessels to nourish the affected areas of the hip.
When osteonecrosis of the hip is diagnosed early, core decompression is sometimes successful in preventing collapse of the femoral head and the development of arthritis.
Core decompression is often combined with bone and cartilage grafting to help regenerate healthy bone and support cartilage at the hip joint. A bone graft is healthy bone tissue that is transplanted to an area of the body where it is needed. The tissue may be taken from a donor (allograft) or from another bone in your body (autograft).
There are also several synthetic bone grafts available today. Sometimes, your own bone marrow cells may be mixed together with the graft substitute to help in the bone regeneration process. It is important to speak with your surgeon about the available options that may be used for your procedure.
Vascularized Fibula Graft
Another surgical option is a vascularized fibula graft. In this procedure, a segment of bone is taken from the small bone in your leg (fibula) along with its blood supply (an artery and vein). This graft is transplanted into a hole created in the femoral neck and head, and the artery and vein are reattached to help heal the area of osteonecrosis.
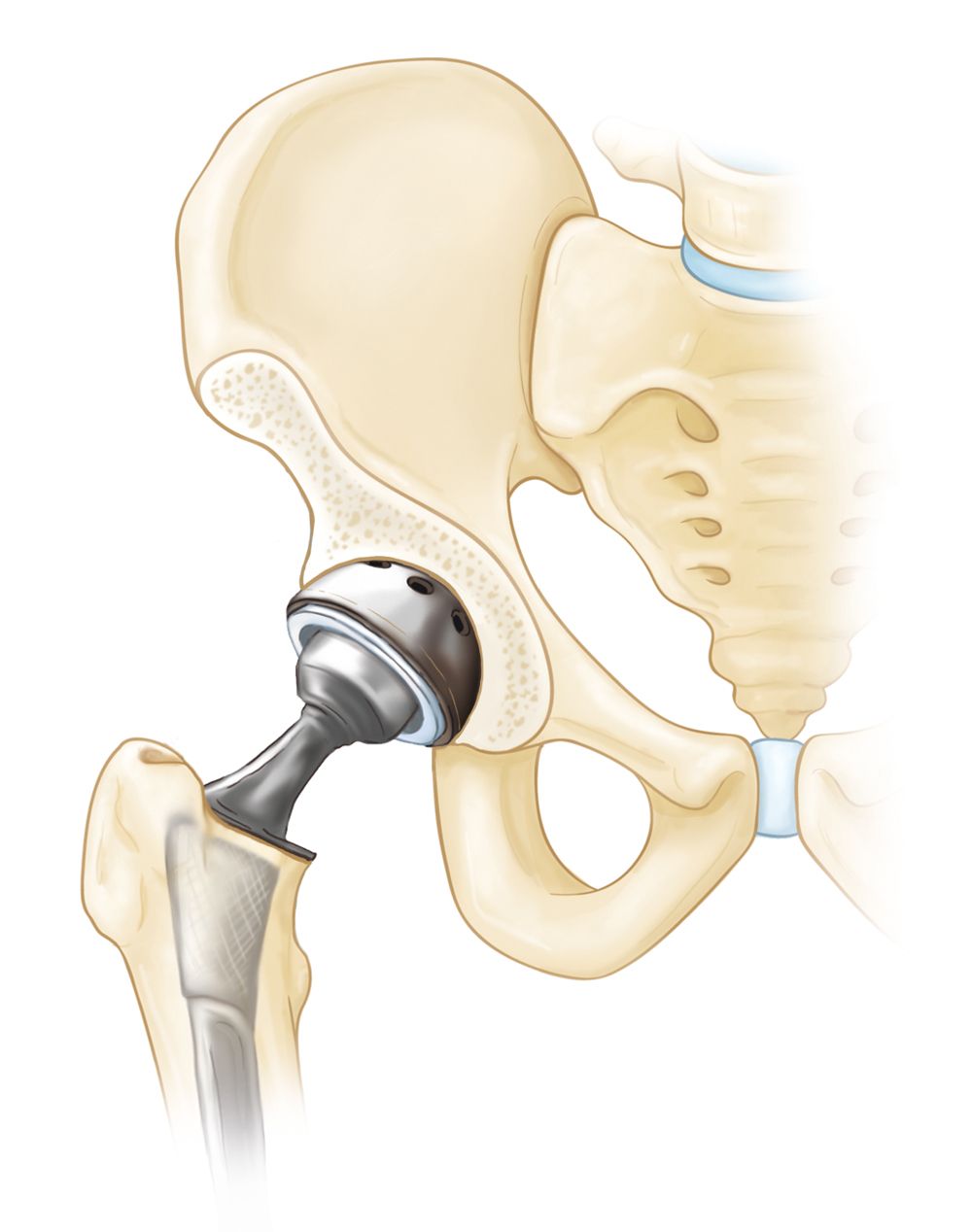
Total Hip Replacement
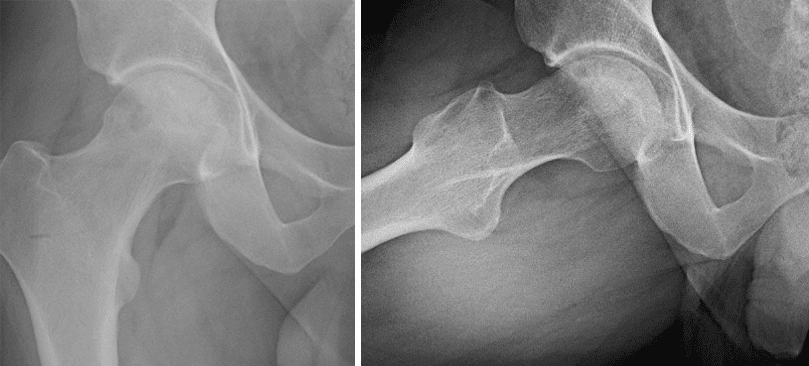
If osteonecrosis has advanced to the point where the femoral head has already collapsed, the most successful treatment is total hip replacement. In this procedure, your doctor removes the damaged bone and cartilage, then positions new metal or plastic joint surfaces to restore the function of your hip.
Outcome
Core decompression prevents osteonecrosis from progressing to severe arthritis and the need for hip replacement in some cases. This depends upon the stage and size of the osteonecrosis at the time of the procedure.
Core decompression achieves the best results when osteonecrosis is diagnosed in its early stages, before the bone collapses. In some of these cases, the bone heals and regains its blood supply after core decompression. It takes a few months for the bone to heal and, during this time, you will need to use a walker or crutches to avoid putting stress on the damaged bone.
Patients with successful core decompression procedures typically return to walking unassisted in about 3 months and may have complete pain relief.
Vascularized fibular grafting is an invasive procedure that requires several months of healing. Typically, you are non-weightbearing for the first several weeks; you will then gradually start weightbearing with an ambulatory assistive device (walker or cane). If a vascularized fibular graft is performed prior to femoral head collapse, the clinical outcomes are usually favorable.
When osteonecrosis is diagnosed after collapse of the bone, core decompression is not usually successful in preventing further collapse. In this situation, the patient is best treated with a total hip replacement. Total hip replacement is successful in relieving pain and restoring function in the majority of patients with osteonecrosis.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.