Diseases & Conditions
Osteoid Osteoma
An osteoid osteoma is a benign (noncancerous) bone tumor that usually develops in the long bones of the body, such as the femur (thighbone) and tibia (shinbone).
Description
Osteoid osteomas:
- Tend to be small — less than 1.5 cm in size — and they do not grow. They do, however, typically cause reactive bone to form around them. They also make a new type of abnormal bone material called osteoid bone. This osteoid bone, along with the tumor cells, forms the nidus (center of the tumor), which is a clear spot seen on X-rays.
- May occur in any bone in the body, but are most often found in the bones of the leg. They are also found in the hands, fingers, and spine.
- Can occur at any age, but they are most common between the ages of 4 and 25 years old. Males are affected approximately three times more often than females.
- Are benign (noncancerous).
- Do not spread to other areas of the body (metastasize).
Cause
The cause of osteoid osteomas is not known.
Symptoms
- The osteoid osteoma releases a prostaglandin that causes inflammation and pain, which is usually relieved with nonsteroidal anti-inflammatory drugs (NSAIDs). The pain is dull, aching, and moderate in intensity, but it can worsen and become severe — especially at night. The pain is not usually related to activity.
- In some cases, a person will suffer the aching bothersome pain of an osteoid osteoma for years before seeing a doctor for diagnosis.
- Depending on the location of the tumor, there may also be swelling.
Doctor Examination
The doctor will perform a physical examination and use imaging and other tests to diagnose your or your child's tumor.
Imaging Tests
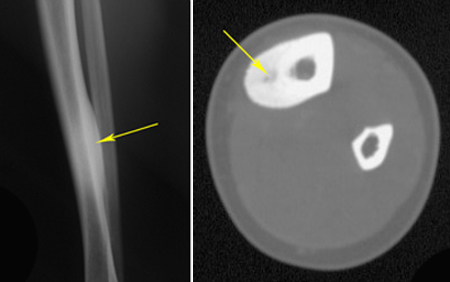
X-rays. X-rays create clear pictures of dense structures such as bone and are helpful in diagnosing an osteoid osteoma. An X-ray of the painful area may reveal thickened bone surrounding a small central core of lower density — a distinctive characteristic of the tumor.
Computerized tomography (CT) scan. A CT scan provides a cross-sectional image of your bone and can also be helpful in evaluating the lesion. A CT scan will commonly show the nidus, or center of the tumor.
Magnetic resonance imaging (MRI) scan. An MRI provides cross-sectional image of the bone and soft tissues. It may show the nidus and surrounding inflammation (swelling) and reactive bone. In pediatric patients, doctors often will start with an MRI to limit radiation exposure. A CT scan may still be needed.
Biopsy. A biopsy may be necessary to confirm the diagnosis of osteoid osteoma. In a biopsy, a tissue sample of the tumor is taken and examined under a microscope. The doctor may give you or your child a local anesthetic to numb the area and take a sample using a needle. A biopsy can also be performed as a small operation. If imaging studies are highly suggestive of an osteoid osteoma, the doctor may not perform a biopsy.
Other tests. To rule out other possible bone problems such as an infection or malignant tumor, the doctor may order additional imaging studies. Certain blood tests may also be used to rule out an infection.
Treatment
Nonsurgical Treatment
- The pain from osteoid osteomas will go away on its own over several years.
- For some patients, regular use of over-the-counter NSAIDs, such as ibuprofen and naproxen, provide excellent relief.
- Sometimes, prescription NSAIDs are recommended.
- There is no increased risk of fracture from an osteoid osteoma, so usually there are no activity restrictions for patients who are managing their tumors nonsurgically.
Surgical Treatment
For patients who do not get adequate pain relief with NSAIDs, cannot tolerate taking NSAIDs regularly, or do not want to wait years for the tumor to go away on its own, other options are available. In these cases, a patient or family may wish to consider surgery.
Radiofrequency ablation or Cryoablation. Ablation procedures are minimally invasive, meaning they do not require incisions or require a very small incision.
- Most commonly, orthopaedic surgeons or interventional radiologists use radiofrequency ablation. In this procedure, the tumor is heated and destroyed is heated and destroyed with a high-frequency electrical current.
- Another option is to freeze the tumor using a similar procedure called cryoablation.
There are pros and cons to both methods, which the doctor will discuss with you.
- Before the procedure, you or your child will be given either general anesthesia or a regional pain block with sedation.
- The doctor will identify the site of the tumor using a CT scan.
- A radiofrequency probe is then inserted into the tumor. The probe heats or freezes the tumor tissues, effectively killing them. There is minimal damage to healthy surrounding tissues.
Ablation cannot be used in certain locations in the spine and hand due to the risks of damaging surrounding structures like the spinal cord, nerves, or blood vessels.
In most patients, the tumor is adequately treated with one radiofrequency ablation treatment. The procedure is often done on an outpatient basis. Patients may go home with a mild pain reliever.
Curettage. One option for surgical treatment of an osteoid osteoma is to scrape or scoop out the entire tumor, particularly the nidus, or central core. The doctor will take great care to ensure that the entire tumor is removed; otherwise, it may grow back.
This is a traditional open procedure in which the surgeon makes an incision in the skin and soft tissues over the tumor site in order to reach the bone. In most cases, this type of surgery is highly successful. However, there are some possible risks — including infection, bleeding, damage to surrounding tissues, and risks associated with general anesthesia.
Recovery
The time it takes to return to daily activities depends on the procedure and the location of the tumor. In many cases, patients return to work or school in a few days with some restrictions. After radiofrequency ablation, most patients have resolution of their symptoms within 24 hours. The doctor will provide you with specific instructions to guide your or your child's recovery.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.