Diseases & Conditions
Osteofibrous Dysplasia and Adamantinoma
Osteofibrous dysplasia (OFD) and adamantinoma are rare bone tumors that are most often found in the tibia (shinbone).
Osteofibrous dysplasia is a noncancerous tumor that typically develops during childhood. It does not spread to other parts of the body and many cases are treated conservatively with careful observation over time.
An adamantinoma is a cancerous tumor that is capable of spreading and requires surgery to remove. It usually appears in adolescents and young adults, after the bones have stopped growing.
Doctors and researchers believe that OFD and adamantinoma are related based on several similarities between the tumors, including location, age of patient, and appearance in x-ray images and under a microscope. In addition, doctors have identified a third similar tumor — an OFD-like adamantinoma or "differentiated adamantinoma" — that includes a mix of cancerous and noncancerous tumor cells, but is not known to spread to other parts of the body.
Although these three tumors are understood to occur along a range of disease — with OFD and adamantinoma at either end and OFD-like adamantinoma in the middle — existing evidence does not show that OFD can progress to adamantinoma.
Description
Osteofibrous Dysplasia (OFD)
Osteofibrous dysplasia makes up less than 1% of all tumors that originate in bone. It usually develops in people younger than 20 years of age, and stabilizes when the bones are no longer growing.
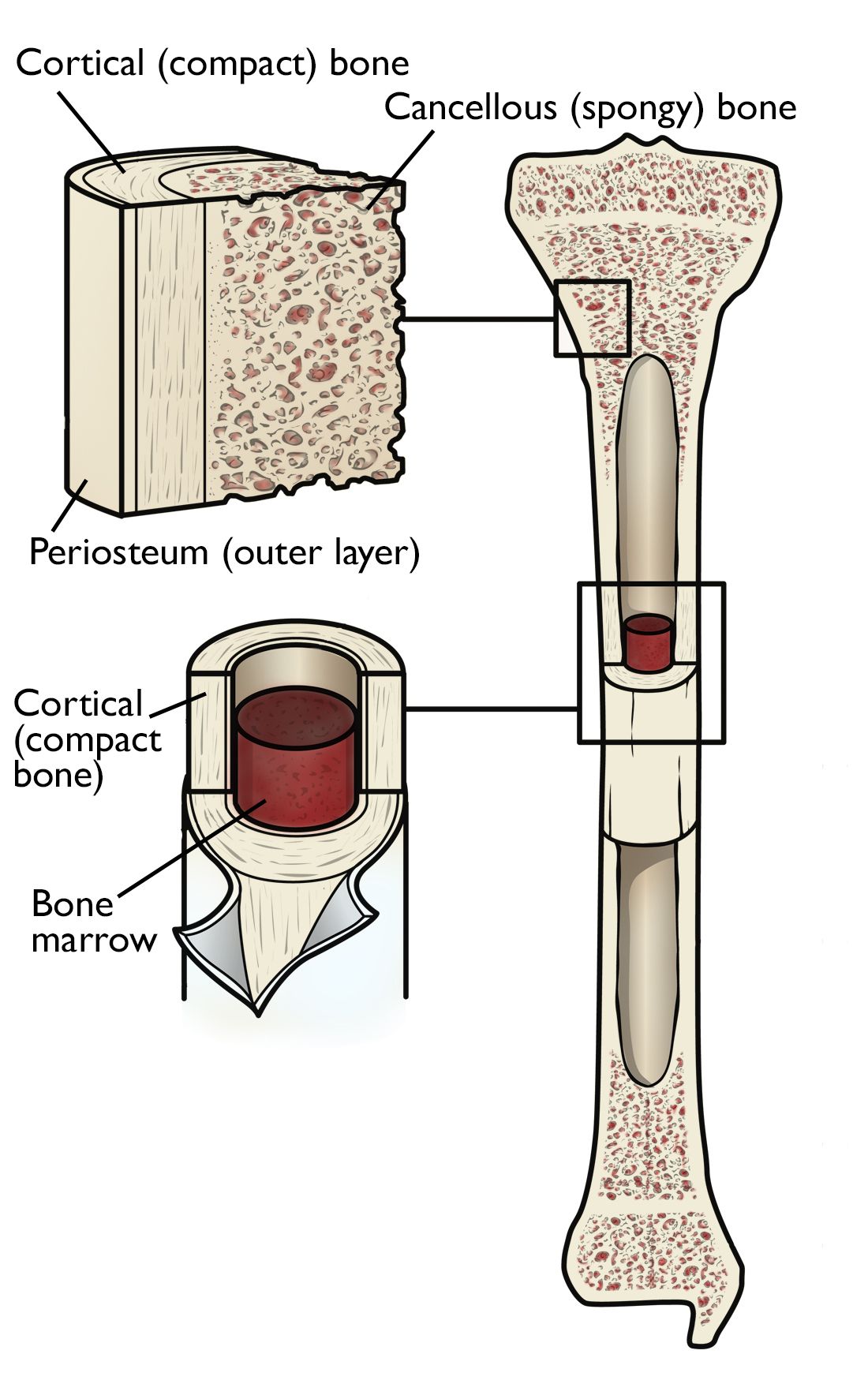
Almost all OFD tumors occur in the long middle part of the tibia, with a few, rare reports of occurrences in the fibula (the smaller bone in the calf), as well as the long bones in the arm (humerus, radius, and ulna). OFD grows within the hard, cortical bone that makes up the outer portion of these bones.
Adamantinoma
Like OFD, adamantinoma is very rare. Fewer than 1% of all cancerous tumors that begin in the bone are adamantinomas.
These slow-growing tumors most often occur in the middle part of the tibia, and in many cases, the fibula bone is also affected. Although uncommon, adamantinomas have also been found in the bones of the arm, rib, pelvis, foot, and spine. Adamantinoma tumors are more aggressive, and can destroy the outer cortex or spread into the central canal of the bone. In many cases, adamantinomas affect the muscles and other soft tissues surrounding the bone, as well.
Unlike OFD, in about 15% of cases, adamantinomas metastasize (spread) to other areas of the body — most often the lungs, lymph nodes, as well as other bones. There have been reports of metastasis occurring years after the first diagnosis and subsequent treatment.
Although adamantinomas can develop in anyone at any age, teenage boys and young men are most often affected.
Cause
The cause of OFD and adamantinoma is unknown. There has been no proven connection between the development of these bone tumors and exposure to chemicals, radiation, or any particular activities.
Symptoms
In many cases of both OFD and adamantinoma, patients do not have symptoms and the condition is discovered in an x-ray obtained for other reasons. When symptoms do occur, they tend to vary among individuals. The most common symptoms of both OFD and adamantinoma include:
- Swelling over the tumor site
- Pain in the area of the tumor
- A break due to the tumor weakening the bone
- When the tumor develops in the tibia, the lower leg may have deformed appearance due to curving (bowing) of the bone.
Doctor Examination
Medical History and Physical Examination
Before a physical examination, your doctor will talk with you about your general health and your symptoms in order to get a good history of the problem. During the physical examination, your doctor will look for tenderness over the bone, swelling, or a mass in the area of your symptoms.
Tests
The signs and symptoms of OFD and adamantinoma are similar to many other types of bone tumor. Your doctor may use several tests to distinguish between different tumors and make an accurate diagnosis.
- X-rays. These tests provide clear pictures of dense structures like bone, and are very helpful in diagnosing bone tumors. Different types of tumors have different characteristics on x-ray. For example, an OFD has very obvious borders and can look like one big tumor or several smaller areas of tumor. An adamantinoma has a "soap bubble" appearance in x-rays.
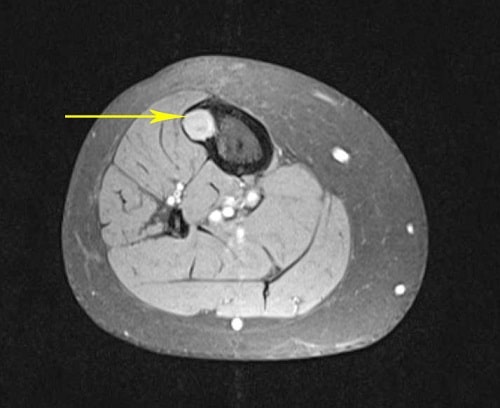
- Other imaging scans. More imaging studies may be needed to further evaluate these tumors. Your doctor may also request computerized tomography (CT) scans, magnetic resonance imaging (MRI) scans, or bone scans to help further define the tumor. These scans can provide more detail, especially of soft tissues. They can also provide cross-sectional images.
A CT scan or MRI scan will show your doctor more precisely where the tumor is located and what its specific characteristics are. For example, in a CT scan, your doctor can see if the adamantinoma tumor has broken through an area of the bone.
-
Biopsy. A biopsy may be necessary to confirm whether the tumor is OFD, an adamantinoma, or an OFD-like adamantinoma. In a biopsy, a tissue sample of the tumor is taken and examined under a microscope. Your doctor may give you a local anesthetic to numb the area and take a sample using a needle. Biopsies can also be performed as a small operation.
If your doctor diagnoses the tumor as adamantinoma, you may require some additional testing to determine whether the disease has spread to other areas, such as a CT scan of your chest or a bone scan.
Treatment
Nonsurgical Treatment
Because OFD is not cancerous and usually will not grow after the patient reaches skeletal maturity, treatment typically involves observation. Your doctor will monitor the tumor with regular x-rays taken every few months. An OFD-like adamantinoma is treated in the same manner.
If the tumor is weakening the bone enough to cause it to bow or change shape, your doctor may recommend wearing a brace. This may also prevent the tumor from causing the bone to break.
Surgical Treatment
In cases in which OFD or an OFD-like adamantinoma causes serious bone deformity or fractures, surgery is often recommended to remove the tumor and stabilize the bone.
Adamantinomas always require surgery. They do not respond to other cancer treatments, such as chemotherapy and radiation.
- Limb salvage surgery. In this procedure, your doctor removes the section of bone where the tumor is located, as well as some healthy tissue surrounding it. The hole is filled with a bone graft — this is bone taken from a cadaver (allograft) or from another bone in your body (autograft) — to stabilize the bone and promote healing with new bone growth. Sometimes, the hole requires reconstruction with a metallic implant (prosthesis) to stabilize the bone.
- Amputation. If the adamantinoma cannot be completely removed with limb salvage surgery, or nerves and blood vessels are involved, all or part of the limb may need to be removed. Your surgeon will talk with you about the benefits of limb salvage versus amputation.
- Recovery. After surgery, your doctor may take more x-rays and other imaging studies to confirm that the tumor has been completely removed.
How long it will take to return to daily activities will vary, depending on how large the tumor was and where it was located. Your doctor will provide you with specific instructions to guide your rehabilitation.
Regular doctor visits and tests every few months may be needed.
Conclusion
An OFD is a benign tumor that has not been shown to become cancerous. Adamantinomas are cancerous, and in many cases return to the same bone location, sometimes many years later. Long-term monitoring of adamantinoma by your doctor is necessary because of this risk of recurrence.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.