Diseases & Conditions
Osteoarthritis
Osteoarthritis, also known as wear-and-tear arthritis, occurs when the cartilage that cushions and protects the ends of your bones gradually wears away. This leads to pain and stiffness that worsens over time, making it difficult to do daily activities.
Osteoarthritis is the most common form of arthritis. It develops slowly and most often occurs during middle and older age.
Although there is no cure for osteoarthritis, there are many treatment options available to help manage pain and keep people active.
Anatomy
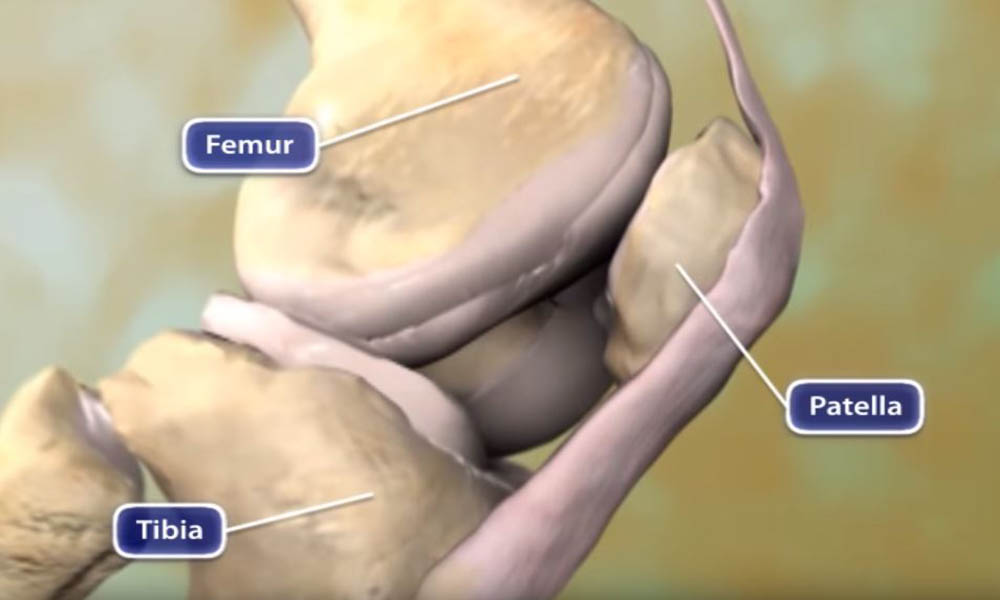
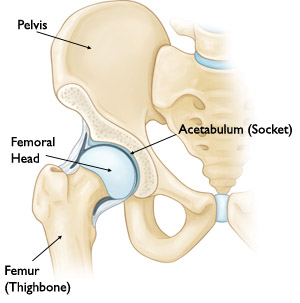
A joint is where the ends of two or more bones meet. For example:
- The hip joint is where the top of the thighbone (femoral head) meets a hollowed-out portion of the pelvis (acetabulum).
- The knee joint is formed between the thighbone (femur) and the bones of the lower leg (tibia and fibula).
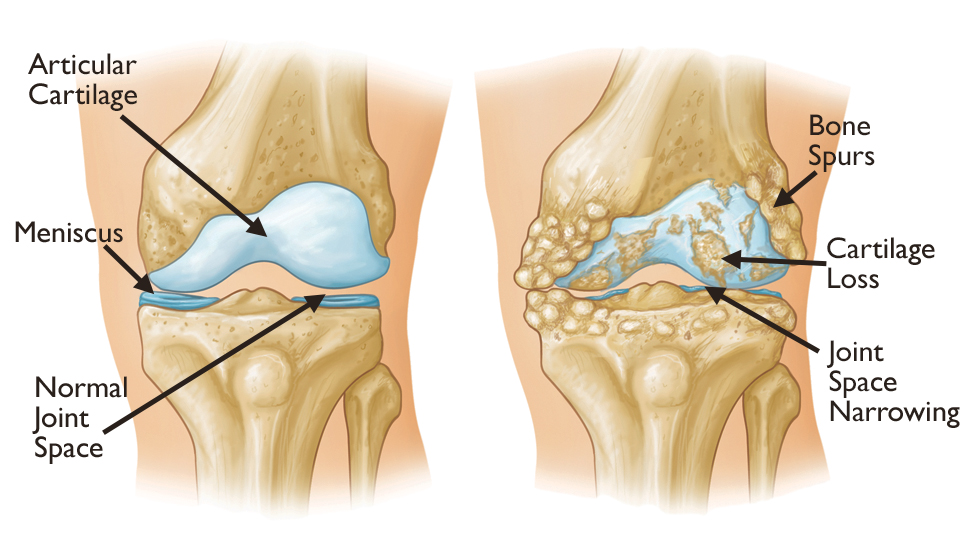
A healthy joint glides easily without pain because a smooth, elastic tissue called articular cartilage covers the ends of the bones that make up the joint.
Cause
With osteoarthritis, the articular cartilage that covers the ends of bones in the joints gradually wears away. Where there was once smooth articular cartilage that allowed the bones to glide easily against each other when the joint bent and straightened, there is now a frayed, rough surface. Joint motion along this exposed surface is painful.
Osteoarthritis usually develops after many years of use. It affects people who are middle-aged or older. Other risk factors for osteoarthritis include obesity, previous injury to the affected joint, and family history of osteoarthritis.
Symptoms
Osteoarthritis can affect any joint in the body including the joints of the spine. Symptoms may range from mild to disabling.
Without cartilage, bones rub directly against each other as the joint moves. A joint affected by osteoarthritis may be stiff, painful, and inflamed,
- Pain or a dull ache will develop gradually over time.
- Pain may be worse in the morning and feel better with activity.
- Vigorous activity may cause pain to flare up.
- The joint may stiffen and look swollen, enlarged, or "out of joint."
- A bump may develop over the joint.
Joint movements such as bending, straightening, and rotating may become more difficult. Loss of motion may follow.
Loose fragments of cartilage can interfere with the smooth motion of a joint. The joint may lock or stick. It may creak, click, snap, or make a grinding noise (crepitus). An arthritic joint may weaken and weight bearing joints such as a knee or ankle may buckle and give way.
Although osteoarthritis cannot be cured, early diagnosis and treatment can help maintain joint mobility, relieve pain and improve function.
Doctor Examination
When you visit your doctor, they will:
- Do a complete medical history
- Perform a physical examination
- Order X-rays and possibly laboratory tests
Medical History
Your doctor will want to know:
- Whether the joint has ever been injured
- When the joint pain began
- The nature of the pain
- Is it continuous, or does it come and go?
- Does it occur in other parts of the body?
- Does it cause nighttime symptoms?
- Does it occur only with activity or at rest as well?
- Whether there are any things that make the pain better
Physical Examination
Your doctor will then examine the affected joint in various positions to see if there is pain or restricted motion. They will look for:
- Creaking or grinding noises (crepitus) that indicate bone-on-bone friction
- Muscle loss (atrophy)
- Signs that other joints are involved
- Signs of injury to muscles, tendons, and ligaments
X-rays
X-rays are taken in different positions to show the extent of joint deterioration, including:
- Narrowing of joint space
- Thinning or erosion of bone
- Bone spurs or other abnormalities
X-rays can also help your doctor distinguish between various forms of arthritis.
Laboratory Tests
Sometimes laboratory tests, such as blood tests, can help rule out other diseases that cause symptoms similar to osteoarthritis.
Treatment
Nonsurgical Treatment
Early, nonsurgical treatment can help maintain joint mobility, improve strength, and relieve pain. Most treatment programs combine lifestyle modifications, medication, and physical therapy.
Lifestyle Changes
Your doctor may recommend rest or a change in activities to avoid provoking osteoarthritis pain. This may include:
- Modifications in work activities
- Switching from high-impact activities (such as aerobics, running, jumping, or competitive sports) to low-impact exercises (such as stretching, walking, swimming, or cycling)
- A weight loss program, if needed, particularly if osteoarthritis affects weight-bearing joints (such as the spine, hip, knee, or ankle)
Medications
- Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can help reduce inflammation.
- Sometimes, your doctor may recommend strong anti-inflammatory agents called corticosteroids, which are injected directly into the joint. Corticosteroids provide short term relief of pain and swelling.
You should check with your primary care doctor before starting any new medication to avoid any potential interactions with your other medications.
Dietary supplements called glucosamine and chondroitin sulfate may help relieve pain from osteoarthritis. (Caution: The U.S. Food and Drug Administration does not test or analyze dietary supplements. Always consult your primary care doctor before taking dietary supplements.)
Physical Therapy
A balanced fitness program, physical therapy, and/or occupational therapy may improve flexibility, increase range of motion, reduce pain, and strengthen the joint.
Other Non-Operative Treatments
Supportive or assistive devices (such as a brace, splint, elastic bandage, cane, crutches, or walker) may be needed.
You may need to apply ice or heat to the affected joint for short periods, several times a day.
Surgical Treatment
If non-operative treatments do not stop the pain or lose their effectiveness, surgery may be considered. The decision to treat surgically depends on:
- Your age and activity level
- The condition of the affected joint
- The extent to which osteoarthritis has progressed
Surgical options for osteoarthritis include:
Arthroscopy
A surgeon uses a pencil-sized, flexible, fiberoptic instrument (arthroscope) to make two or three small incisions to remove bone spurs, cysts, damaged lining, or loose fragments in the joint.
Learn more: Knee Arthroscopy
Learn more: Hip Arthroscopy
Osteotomy
The long bones of the arm or leg are realigned to take pressure off the affected portion of the joint.
Learn more: Osteotomy of the Knee
Joint fusion
A surgeon eliminates the joint by fastening together the ends of bone (fusion). Pins, plates, screws, or rods may hold bones in place while they heal. This procedure eliminates the joint's flexibility.
Fusion is most commonly performed in the spine, hand, and foot.
Learn more: Spinal Fusion
Joint replacement
A surgeon removes parts of the bones and creates an artificial joint with metal or plastic components (total joint replacement or arthroplasty).
Learn more: Total Joint Replacement
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.