Diseases & Conditions
Lumbar Spinal Stenosis
Lumbar spinal stenosis is a common cause of low back and leg pain, or sciatica.
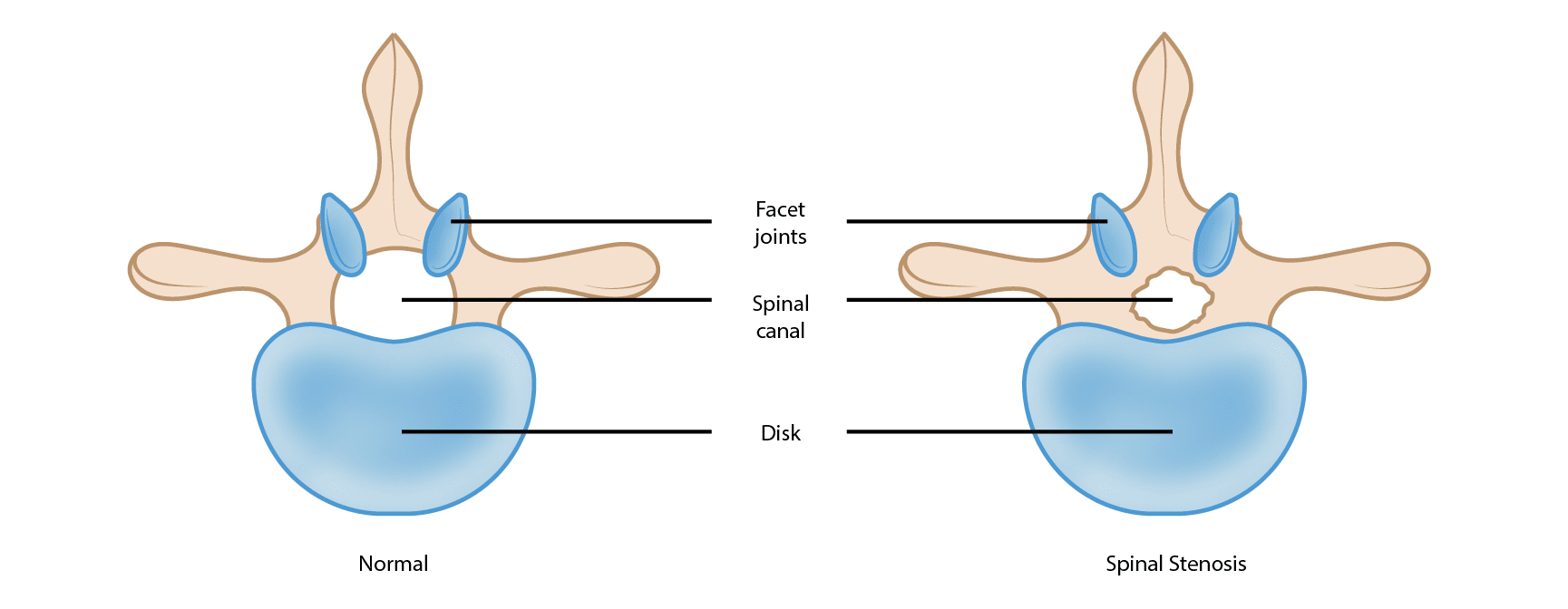
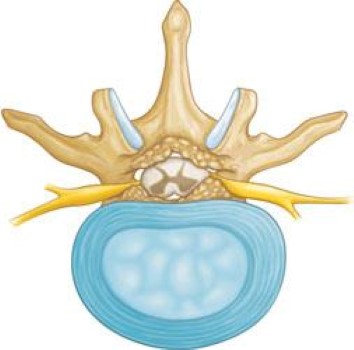
As we get older, the spine can slowly wear down. This wear and tear can make the space inside the spinal canal smaller. That space holds the spinal cord and spinal nerves, and when it gets too tight, these nerves can be squeezed. This is called spinal stenosis.
By age 50, up to 95% of people have some wear and tear — or “degenerative changes” — in their spine. Spinal stenosis happens most often in adults over 60 and affects men and women equally.
A small number of people are born with back problems that develop into lumbar spinal stenosis. This is known as congenital spinal stenosis. Typically, this occurs in people who are born with a smaller spinal canal. Because there is less space within the canal, degeneration — wear and tear due to arthritis — can affect them sooner.
Congenital spinal stenosis occurs most often in men. People usually first notice symptoms of congenital spinal stenosis between the ages of 30 and 50.
Anatomy
The spine is made up of small bones, called vertebrae. These bones are stacked on top of each other. Muscles, ligaments, nerves, and soft intervertebral disks are additional parts of your spine.
Understanding your spine and how it works can help you better understand spinal stenosis. Learn more about spine anatomy: Spine Basics
Description
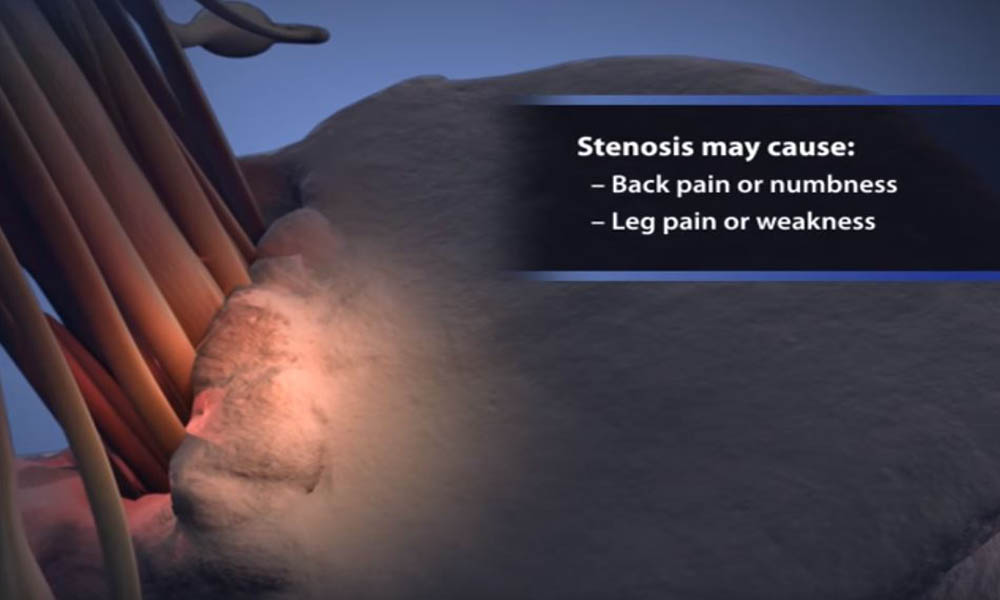
Spinal stenosis happens when the space around the spinal cord and spinal nerves gets smaller. This puts pressure on the spinal cord and the spinal nerve roots, and may cause pain, numbness, or weakness in the legs.
Cause
Arthritis is the most common cause of spinal stenosis. Arthritis is when joints wear down and refers to degeneration of any joint in the body.
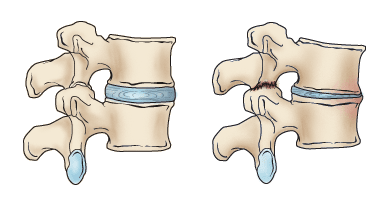
In the spine, arthritis can develop when disks dry out and shrink. When we are young, disks are full of water and act like cushions. As we age, they lose water and get smaller. This problem causes settling, or collapse, of the disk spaces and loss of disk space height.
As the disks shrink and the spine settles, two things occur.
- First, more pressure is placed on nearby joints, called facet joints. This pressure can cause arthritis in these joints, too.
- Second, the tunnels through which the nerves exit (the foramen) become smaller.
As the facet joints experience increased pressure, they also begin to degenerate and develop arthritis, just like the wear-and-tear arthritis that commonly occurs in the hip or knee joint.
As the facet joint wears down, the body responds by forming bone spurs to stabilize the joint. In addition, the ligaments around the joints that typically connect the bones together (called the ligamenta flava) increase in size. The combination of bone spurs and thickened ligaments crowds the space for the nerves, resulting in stenosis.
Symptoms
- Back pain. People with spinal stenosis may or may not have back pain, depending on the degree of arthritis that has developed.
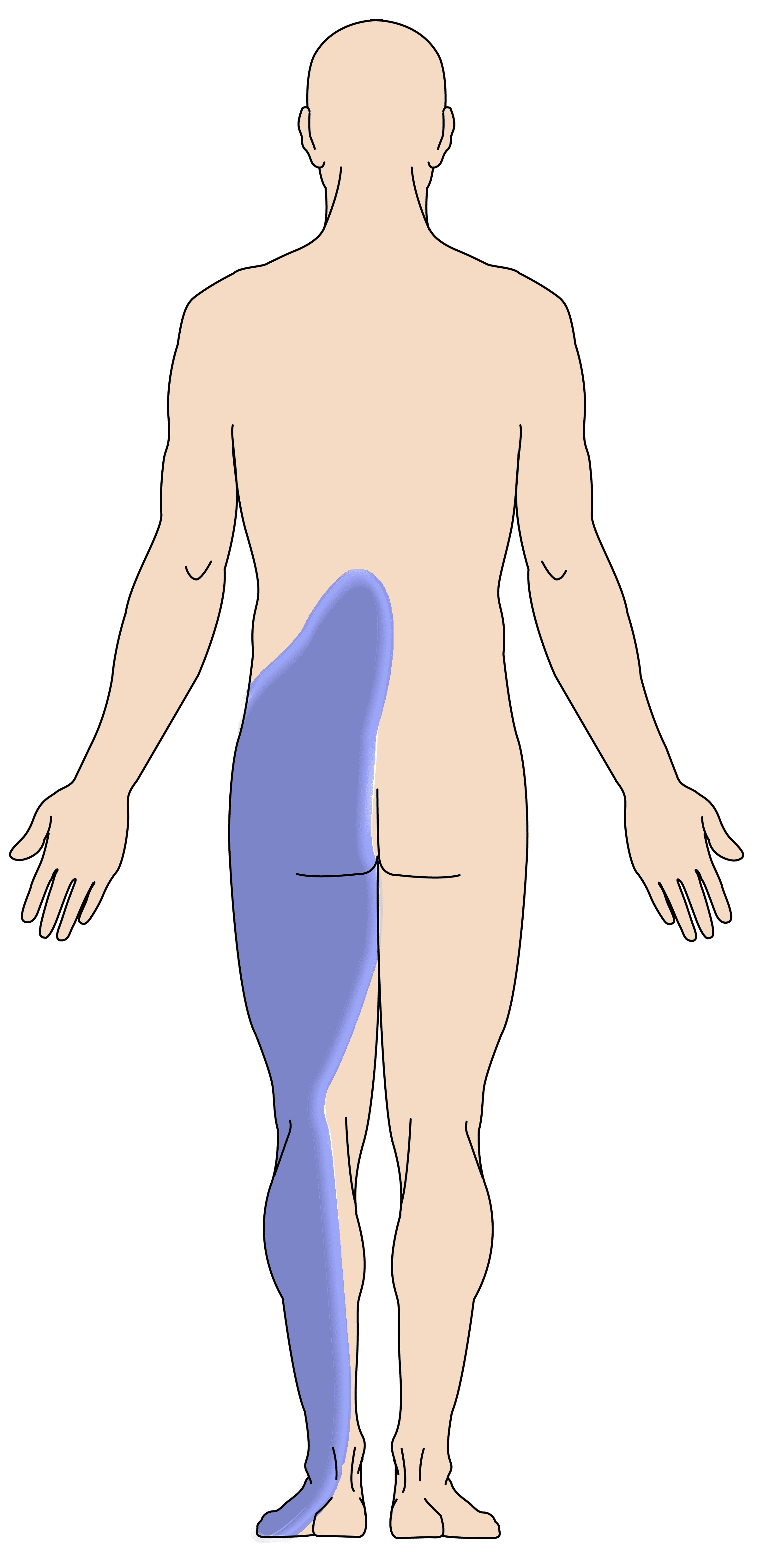
- Burning pain in buttocks or legs (sciatica). Pressure on spinal nerves can result in pain in the areas that the nerves supply. The pain may be described as an ache or a burning feeling. It typically starts in the area of the buttocks and moves down the leg, sometimes reaching the foot.
- Numbness or tingling in buttocks or legs. As pressure on the nerve increases, numbness and tingling often accompany the burning pain, although not all patients will have both burning pain and numbness/tingling.
- Weakness in the legs or foot drop (difficulty lifting the front part of the foot). Once the pressure reaches a critical level, weakness can occur in one or both legs. Some patients will have a "foot drop," or the feeling that their foot slaps on the ground while walking.
- Acute cauda equina syndrome. This rare condition is considered a medical emergency that requires prompt treatment. If the compression of the nerves is severe, you can experience numbness in your private area and lose control of your bowel and/or bladder function. You may also lose strength in your legs and not be able to walk. If these symptoms occur, you may need emergency surgery.
People with spinal stenosis often feel better when they lean forward or sit down. Standing up straight or walking usually make the pain worse. Studies of the lumbar spine show that leaning forward can increase the space available for the nerves.
Some people note that they can ride a stationary bike or walk while leaning on a shopping cart. Walking more than 1 or 2 blocks, however, may bring on severe sciatica or weakness.
Doctor Examination
Medical History and Physical Examination
After discussing your symptoms and medical history, your doctor will examine your back. This will include looking at your back and pushing on different areas to see if it hurts. Your doctor may have you bend forward, backward, and side-to-side to look for limitations or pain.
Imaging Tests
Other tests that may help your doctor confirm your diagnosis include:
X-rays. Although they only visualize bones, X-rays can help determine if you have spinal stenosis. They will show aging-related changes, like loss of disk height or bone spurs.
X-rays taken while you lean forward and backward can show instability in your joints. X-rays can also show when there is too much mobility in your spine. This is called spondylolisthesis.
Magnetic resonance imaging (MRI). An MRI helps doctors visualize soft tissues, such as muscles, disks, nerves, and the spinal cord.
Additional tests. Computed tomography (CT) scans can create cross-section images of your spine and show the bony structures better than X-rays. Your doctor may also order a CT myelogram. In this procedure, dye is injected into the spine to make the nerves show up more clearly. It can help your doctor determine whether the nerves are being compressed.
Nonsurgical Treatment
Nonsurgical treatment options focus on restoring function and relieving pain. Although nonsurgical methods do not improve the narrowing of the spinal canal, many people report that these treatments do help relieve symptoms.
- Physical therapy. Stretching exercises, massage, and lumbar and back/abdominal core strengthening often help manage symptoms.
- Lumbar traction. Although it may be helpful in some patients, traction offers very limited results. There is no scientific evidence of its effectiveness.
- Anti-inflammatory medications. Because stenosis pain is caused by pressure on a spinal nerve, reducing inflammation (swelling) around the nerve may relieve pain. Non-steroidal anti-inflammatory drugs (NSAIDs) initially provide pain relief. When used over the course of 5 to 10 days, they can also have an additional anti-inflammatory effect.
Most people are familiar with nonprescription NSAIDs, such as aspirin, ibuprofen, and naproxen. Whether over-the-counter or prescription strength, these medicines must be used carefully. They can lead to gastritis, stomach ulcers, and kidney problems. If you develop acid reflux or stomach pains while taking an anti-inflammatory, be sure to talk to your doctor.
- Steroid injections, also known as epidural steroid injections. Cortisone is a powerful anti-inflammatory drug. Cortisone injections around the nerves or in the "epidural space" can decrease swelling, as well as pain. They also reduce numbness, but not weakness, in the legs. Patients should receive no more than three injections per year. Learn more: Spinal Injections
- Acupuncture. Acupuncture can be helpful in treating some of the pain in less severe cases of lumbar stenosis. Although it can be very safe, long-term success with this treatment has not been proven scientifically.
- Chiropractic manipulation. Chiropractic manipulation is generally safe and can help with some of the pain from lumbar stenosis. Take care, however, if you have osteoporosis or a herniated disk. Manipulation of the spine in these cases can worsen symptoms or cause other injuries.
Surgical Treatment
Surgery for lumbar spinal stenosis is generally reserved for people who have poor quality of life due to pain and weakness, including difficulty walking for extended periods of time. This is often the reason that people consider surgery.
There are two main surgical options to treat lumbar spinal stenosis: laminectomy and spinal fusion. Both options can result in excellent pain relief. Be sure to discuss the advantages and disadvantages of both with your doctor.
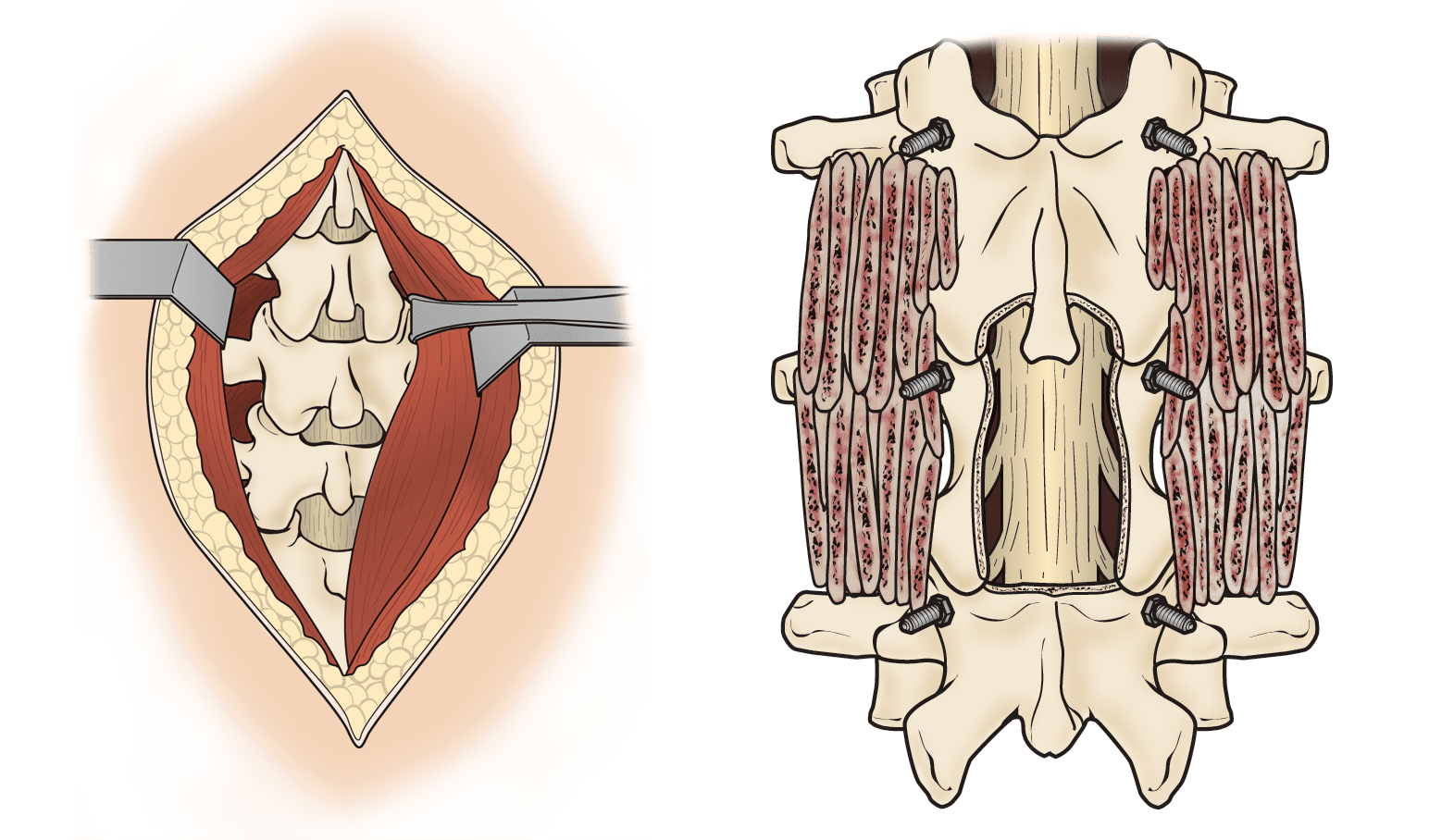
Laminectomy. This procedure involves removing the bone, bone spurs, and ligaments that are compressing the nerves. Laminectomy can be performed as open surgery, in which your doctor uses a single, larger incision to access your spine. The procedure can also be done using a minimally invasive method, where several smaller incisions are made. Your doctor will discuss the right option for you.
Spinal fusion. If arthritis has progressed to spinal instability, your surgeon may recommend a combination of decompression and stabilization or spinal fusion.
Rehabilitation
After surgery, you may stay in the hospital for a short time, depending on your health and the procedure performed. Healthy people who undergo decompression alone may go home the same or next day and may return to normal activities after only a few weeks. Fusion generally adds 2 to 3 days to the hospital stay.
Your surgeon may give you a brace or corset to wear for comfort. They will likely encourage you to begin walking as soon as possible. Most people need some physical therapy to strengthen their backs.
Your physical therapist may show you exercises to help you build and maintain strength, endurance, and flexibility for spinal stability. Some of these exercises will help strengthen your abdominal muscles, which help support your back. Your physical therapist will create an individualized program, taking into consideration your health and history.
Most people can go back to a desk job within a few days to a few weeks after surgery. They may return to normal activities after 2 to 3 months. Older patients who need more care and assistance may be transferred from the hospital to a rehabilitation facility for a period of time before going home.
Pain Medication After Surgery
A short course (a few weeks) of opioids is typical after a laminectomy. After a fusion procedure, the duration may be longer. If you did not take strong pain medicine (opioids) before surgery, you might only need them for a few weeks afterward. If you were already on opioids, you may need them longer after surgery because your body is used to the pain medication.
Surgical Risks
There are minor risks associated with every surgical procedure. These include bleeding, infection, blood clots, and reaction to anesthesia. These risks are usually very low.
Elderly people, overweight people, diabetics, smokers, and those with multiple medical problems have higher rates of complications from surgery.
Specific complications from surgery for spinal stenosis include:
- Tear of the sac covering the nerves (dural tear)
- Failure of the bone fusion to heal if a fusion is performed
- Failure of screws or rods if a fusion is performed
- Nerve injury
- Need for further surgery
- Failure to relieve symptoms
- Return of symptoms
Surgical Outcomes
Overall, the results of laminectomy with or without spinal fusion for lumbar stenosis are good to excellent in the majority of patients. Patients tend to see more improvement of leg pain than back pain, and most people can resume a normal lifestyle after a period of recovery from surgery.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.