Diseases & Conditions
Infections After Fracture
Most fractures (broken bones) do not lead to infections. When infections do occur after fractures, the treatment and recovery can be prolonged and complicated.
Cause
- Infections typically occur after fractures because bacteria enter the body during the traumatic event.
- Although uncommon, bacteria can also enter the body during surgery to set the broken bones or later, after the injury has healed.
Open Fractures
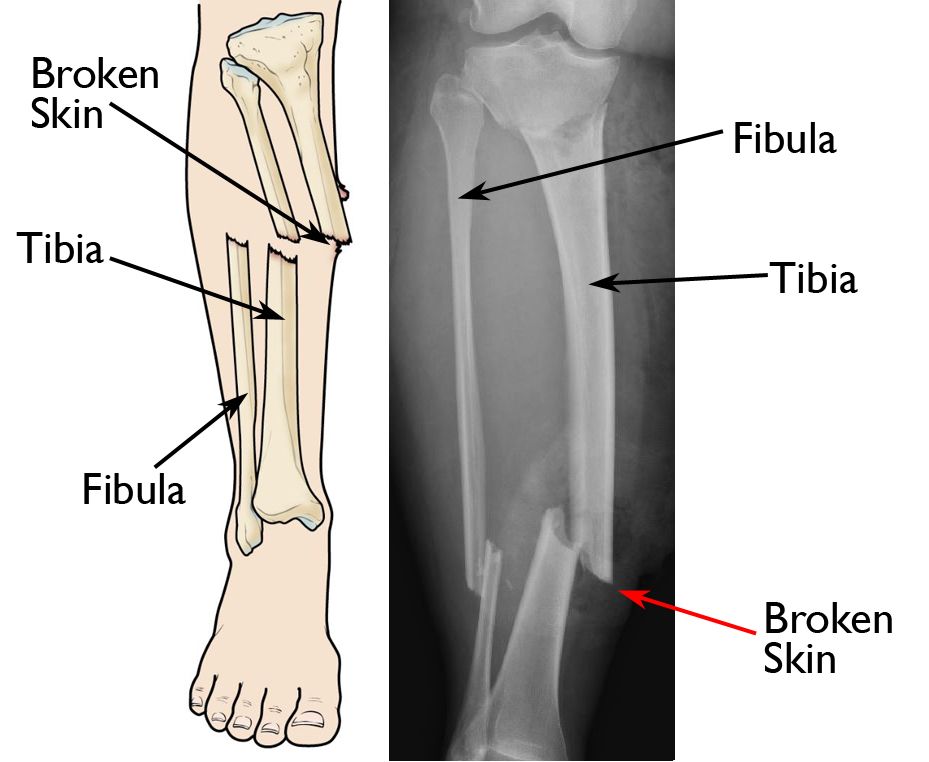
When a bone breaks in such a way that bone fragments stick out through the skin or a wound penetrates down to the bone, it is called an open or compound fracture.
The skin normally acts as a barrier to outside contaminants, including bacteria. When the skin is broken, bacteria can easily travel down to the broken bone, and this can lead to infection.
Surgery
During surgery to fix a fracture, the surgeon cuts through skin and other tissues to reach the broken bone. The risk for developing an infection in this setting is quite low, usually less than 2 to 3% in healthy individuals, although this varies depending on the injury and the operation performed. Preventive antibiotics are given before surgery to lower the risk of infection.
Less commonly, an infection can occur at the surgical site even long after the injury has healed. This occurs when bacteria enter the body during another procedure (such as a tooth extraction or root canal) and make their way through the bloodstream to the implants used to treat the fracture.
Risk Factors
Chronic diseases that lower your immune system may put you at greater risk for infection after fracture. These include:
- Diabetes mellitus
- Immune deficiencies (such as HIV)
- Rheumatoid arthritis
You may also be at greater risk because of the lifestyle choices you make. These include:
- First and foremost, smoking and using nicotine products
- Morbid obesity
- Poor nutrition
- Poor hygiene
Symptoms
- An infection after fracture will usually cause increased pain, warmth, redness, and swelling around the affected area — more than what is considered normal.
- You may experience persistent pain that does not improve when you rest and elevate the injured limb.
- A pus pocket may form; if it bursts, pus will drain from the injury.
- You may have a fever, chills, and night sweats.
- If the infection is near a joint, such as your knee or shoulder, the joint may be painful and difficult to move.
Tests
Even if an infection appears obvious, your doctor may order an X-ray if you have not had one recently. Blood tests may also be used to help diagnose the infection. These may include:
- White blood cell count (WBC)
- Sedimentation rate (ESR)
- C-reactive protein (CRP)
If these tests do not confirm the infection, your doctor may order additional tests, such as a computerized tomography (CT) scan, tagged white blood cell scan, or magnetic resonance imaging (MRI) scan, although this is rare.
If the suspected infection is near a joint, your doctor may use a needle to draw fluid from the joint. This fluid will then be analyzed to determine if bacteria are present.
Because a healing fracture may show the same positive test results as an infection, it is often hard for doctors to firmly diagnose an infection after a fracture. It is often up to the knowledge and experience of the doctor to determine whether there is an infection.
Treatment
An open fracture is a surgical emergency.
- You will be started on antibiotics as soon as possible in the emergency room.
- Your doctor will then clean the wound and remove as much contamination as possible from the skin, other tissues, and bone. This procedure, called debridement and irrigation, is performed in an operating room. It is suggested that people with open fractures undergo debridement and irrigation as soon as is reasonable, ideally within 24 hours of sustaining the injury.
- Depending on the severity of your injury, you may require several debridement and irrigation procedures.
If you have an infection after surgery, your doctor may initially treat it with antibiotics alone. In some cases, additional surgery to clean out the infection may be necessary.
During surgery:
- Your doctor will either swab or take samples of the infected tissue to find out what type of bacteria is causing the infection. This stage of treatment may require more than one surgery.
- Special drains may be placed in the wound to help drain the infection.
- Antibiotic delivery systems, like antibiotic beads, may also be used to provide higher concentrations of antibiotics.
Once the type of bacteria is identified, your doctor can choose the most effective antibiotics to treat the infection. An infectious disease specialist may work with your doctor to determine the appropriate antibiotics. Most patients will have to take antibiotics for 6 to 12 weeks.
A bone infection can be hard to eliminate. It may require long-term antibiotic treatment, as well as several surgeries. Occasionally, a patient may need to take antibiotics for the rest of their life.
Amputation
In very rare cases, when infection persists and becomes life threatening, amputation of the infected limb may be considered. Amputation is typically considered in only the most severe cases.
Outcome
An infection after a fracture may require multiple trips to the operating room, long-term antibiotic treatment, and a long period of healing.
If an infection is successfully treated, however, patients have a high likelihood of recovering without serious, ongoing problems.
To help doctors prevent and treat infections — including surgical site infections — the American Academy of Orthopaedic Surgeons has conducted research to provide some useful guidelines. These are recommendations only and may not apply to every case. For more information: Surgical Site Infections - Clinical Practice Guideline (CPG) | American Academy of Orthopaedic Surgeons (aaos.org)
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.