Diseases & Conditions
Ganglion Cyst of the Wrist and Hand
Ganglion cysts are the most common mass or lump in the hand. They are not cancerous and, in most cases, are harmless. They occur in many locations, but most often develop on the back of the wrist.
These fluid-filled cysts can quickly appear, disappear, and change size. Many ganglion cysts do not require treatment. However, if the cyst hurts, if it affects function, or if you are unhappy with how it looks, there are several treatment options available.
Description
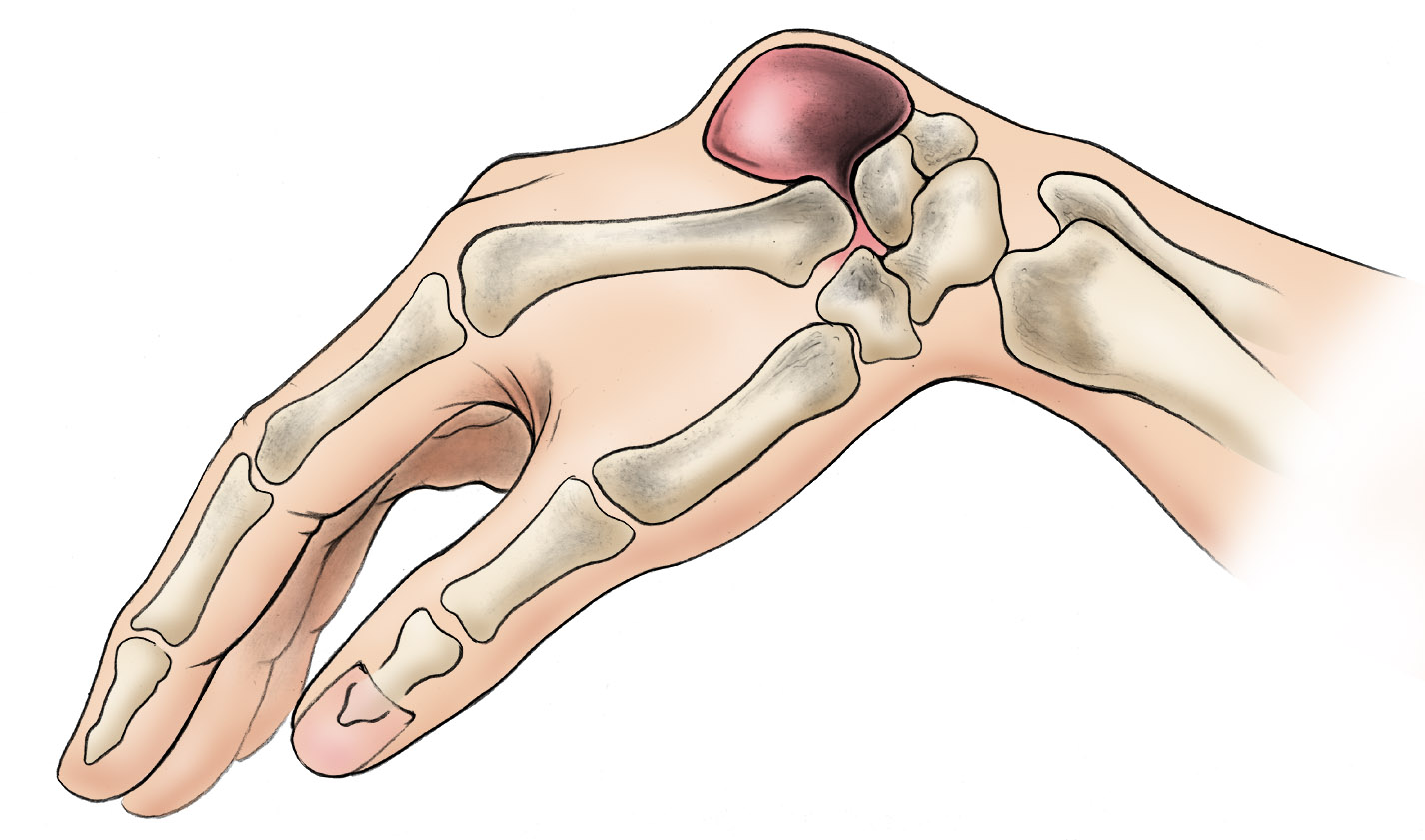
A ganglion arises out of a joint, like a balloon on a stalk. It grows out of the tissues surrounding a joint, such as ligaments, tendon sheaths, and joint linings. Inside the balloon is a thick, slippery fluid, similar to the fluid that lubricates your joints.
Ganglion cysts can develop in several of the joints in the hand and wrist, including:
- Both the top and underside of the wrist
- The end joint of a finger
- The base of a finger
They vary in size, and in many cases, grow larger with increased activity. With rest, the lump usually becomes smaller.
Cause
It is not known what triggers the formation of a ganglion.
- They are most common in younger people between the ages of 15 and 40
- Women are more likely to be affected than men.
- They are common among gymnasts, who repeatedly apply stress to the wrist.
- Ganglion cysts that develop at the end joint on the nail side of a finger — also known as mucous cysts — are typically associated with arthritis in the finger joint and are more common in women between the ages of 40 and 70.
Symptoms
Most ganglions form a visible lump; however, smaller ganglions can remain hidden under the skin (occult ganglions). Although many ganglions produce no other symptoms besides the appearance of a mass, if a cyst puts pressure on the nerves that pass across the joint, it can cause pain, tingling, and muscle weakness.
If you have a large cyst, even if it is not painful, you may feel anxious or unhappy simply because of how it looks.
Doctor Examination
Medical History and Physical Examination
During the initial appointment, your doctor will discuss your medical history and symptoms. They may ask you:
- How long you have had the ganglion
- Whether it changes in size
- Whether it is painful
Your doctor may apply pressure to the cyst to test for tenderness or discomfort. Because a ganglion is filled with fluid, it is translucent (almost transparent). Your doctor may shine a penlight up to the cyst to see whether light shines through. This can help confirm that the mass is truly a cyst and not a solid tumor.
Imaging Tests
X-rays. X-rays create clear pictures of dense structures, like bone. Although X-rays will not show a ganglion cyst, they can be used to rule out other conditions, such as arthritis of the hand, arthritis of the wrist, or a bone tumor.
Magnetic resonance imaging (MRI) scans or ultrasounds. MRI scans and ultrasounds can better show soft tissues, like a ganglion, than X-rays. Sometimes, an MRI or ultrasound is needed to find an occult ganglion that is not visible, or to distinguish the cyst from other tumors. However, further imaging is often not needed prior to treatment.
Treatment
Nonsurgical Treatment
Initial treatment of a ganglion cyst is nonsurgical.
Observation. If you have no pain or other symptoms, your doctor may recommend just waiting and watching to make sure that no unusual changes occur. This is typically safe because ganglions are not cancerous and may disappear on their own in time.
Immobilization. Activity often causes the ganglion to increase in size, which may increase pressure on surrounding nerves, causing pain. A wrist brace or splint may relieve symptoms and cause the ganglion to decrease in size. As pain decreases, your doctor may prescribe exercises to strengthen the wrist and improve range of motion.
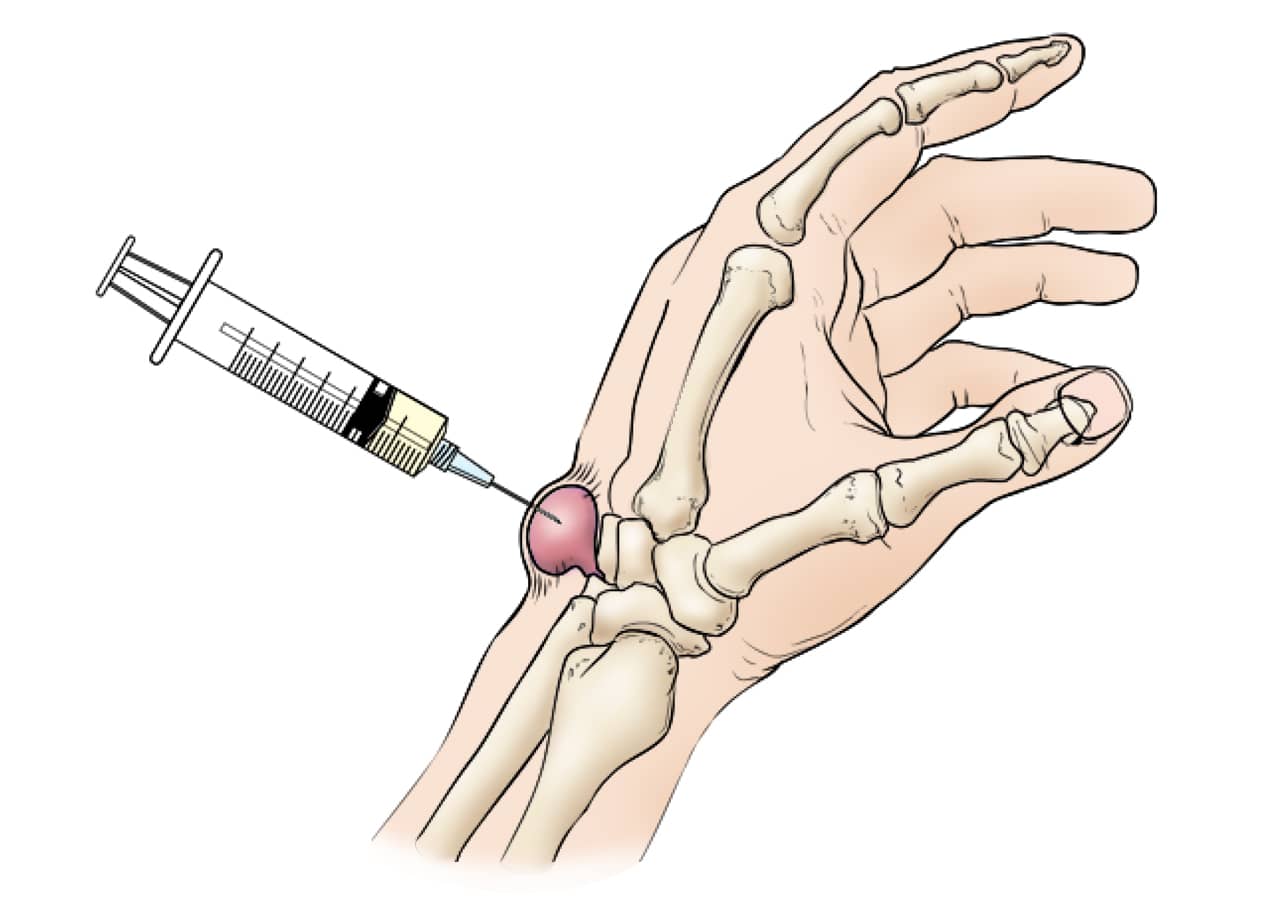
Aspiration. If the ganglion causes a great deal of pain or severely limits activities, the fluid may be drained from it. This procedure is called an aspiration.
The area around the ganglion cyst is numbed and the cyst is punctured with a needle so that the fluid can be withdrawn.
Unfortunately, aspiration often fails to eliminate the ganglion because the root or connection to the joint or tendon sheath is not removed. A ganglion can be like a weed which will grow back if the root is not addressed. Thus, in many cases, the ganglion cyst returns after an aspiration procedure.
Aspirations are most often used for ganglions located on the top of the wrist. Ganglions on the palm side of the wrist can be tricky to aspirate because they are near major vessels and nerves.
Surgical Treatment
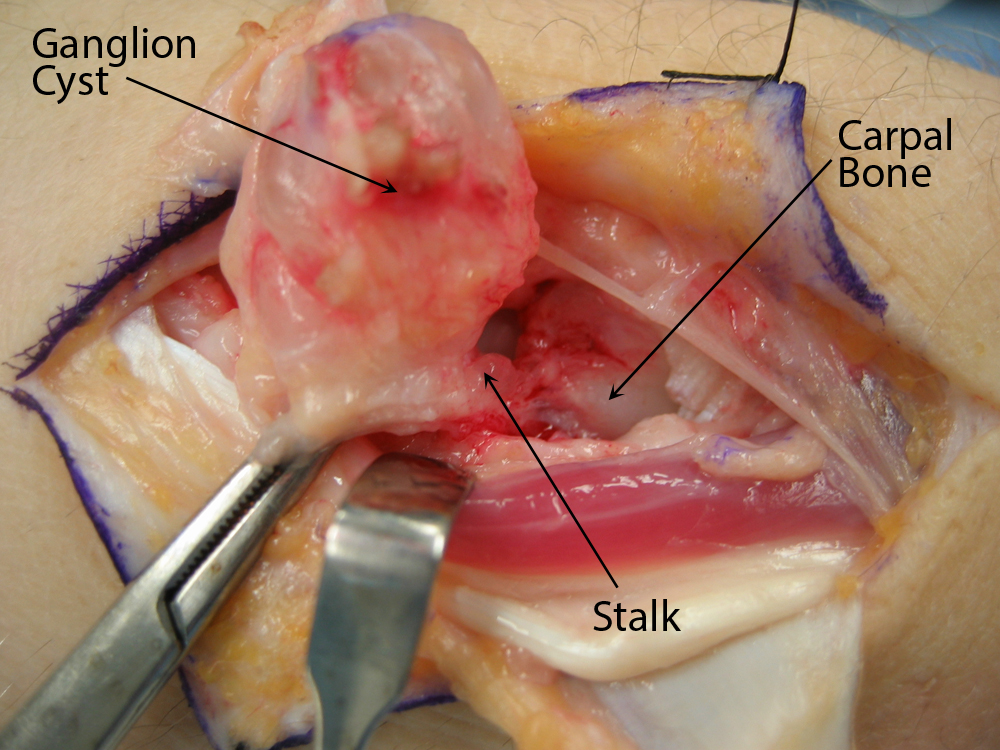
Your doctor may recommend surgery if your symptoms are not relieved by nonsurgical methods, or if the ganglion returns after aspiration. The procedure to remove a ganglion cyst is called an excision.
Surgery involves removing the cyst as well as addressing the stalk from which the cyst arises. This may mean removing part of the involved joint capsule or tendon sheath to ensure removal of the root of the cyst. Even after excision, there is a small chance the ganglion will return.
Excision is usually an outpatient procedure, meaning patients go home the day of surgery after a period of observation in the recovery area. There may be some tenderness, discomfort, and swelling after surgery. You are usually able to resume normal activities 2 to 6 weeks after the procedure.
Outcomes
Ganglion cysts rarely, if ever, cause permanent disability. Cysts that do not go away on their own and cause symptoms almost always respond to surgery. In the rare case that a ganglion comes back after surgery, a revision surgery can be performed to remove the cyst again. After removal, most patients experience relief of symptoms.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.