Diseases & Conditions
Arthritis of the Foot and Ankle
Arthritis is inflammation of one or more of your joints. It can cause pain and stiffness in any joint in the body and is common in the small joints of the foot and ankle.
There are more than 100 forms of arthritis, many of which affect the foot and ankle. All types can make it difficult to walk and perform activities you enjoy.
Although there is no cure for arthritis, there are many treatment options available to slow the progression (worsening) of the disease and relieve symptoms. With proper treatment, many people with arthritis are able to manage their pain, remain active, and lead fulfilling lives.
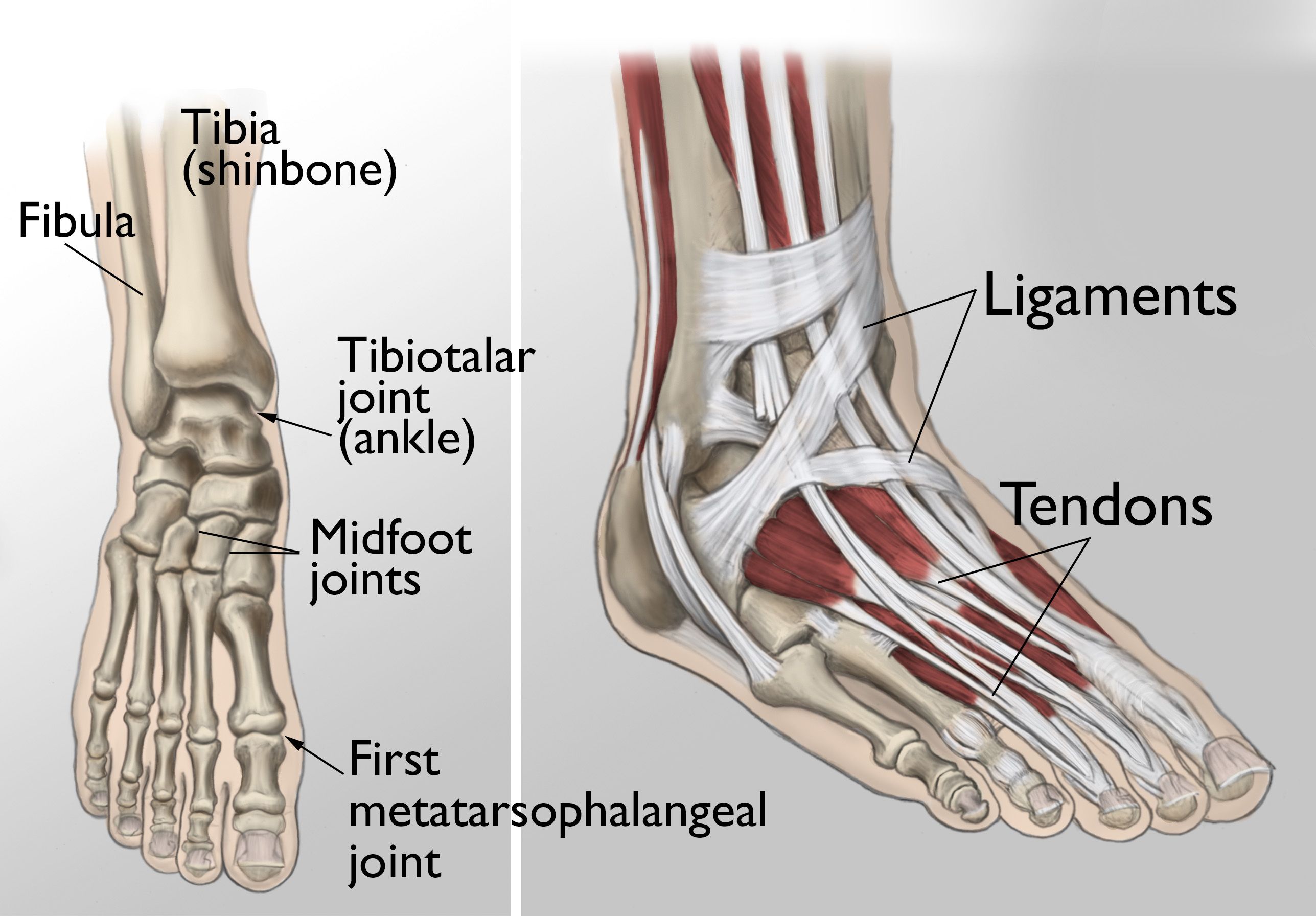
Anatomy
During standing, walking, and running, the foot and ankle provide support, shock absorption, balance, and several other functions that are essential for motion. Three bones make up the ankle joint, primarily enabling up and down movement. There are 28 bones in the foot, and more than 30 joints that allow for a wide range of movement.
In many of these joints, the ends of the bones are covered with articular cartilage — a slippery substance that helps the bones glide smoothly over each other during movement. Joints are surrounded by a thin lining called the synovium. The synovium produces a fluid that lubricates the cartilage and reduces friction.
Tough bands of tissue, called ligaments, connect the bones and provide stability to the joints. Muscles and tendons also support the joints and provide the strength to make them move.
Description
The major types of arthritis that affect the foot and ankle are osteoarthritis, rheumatoid arthritis, and posttraumatic arthritis.
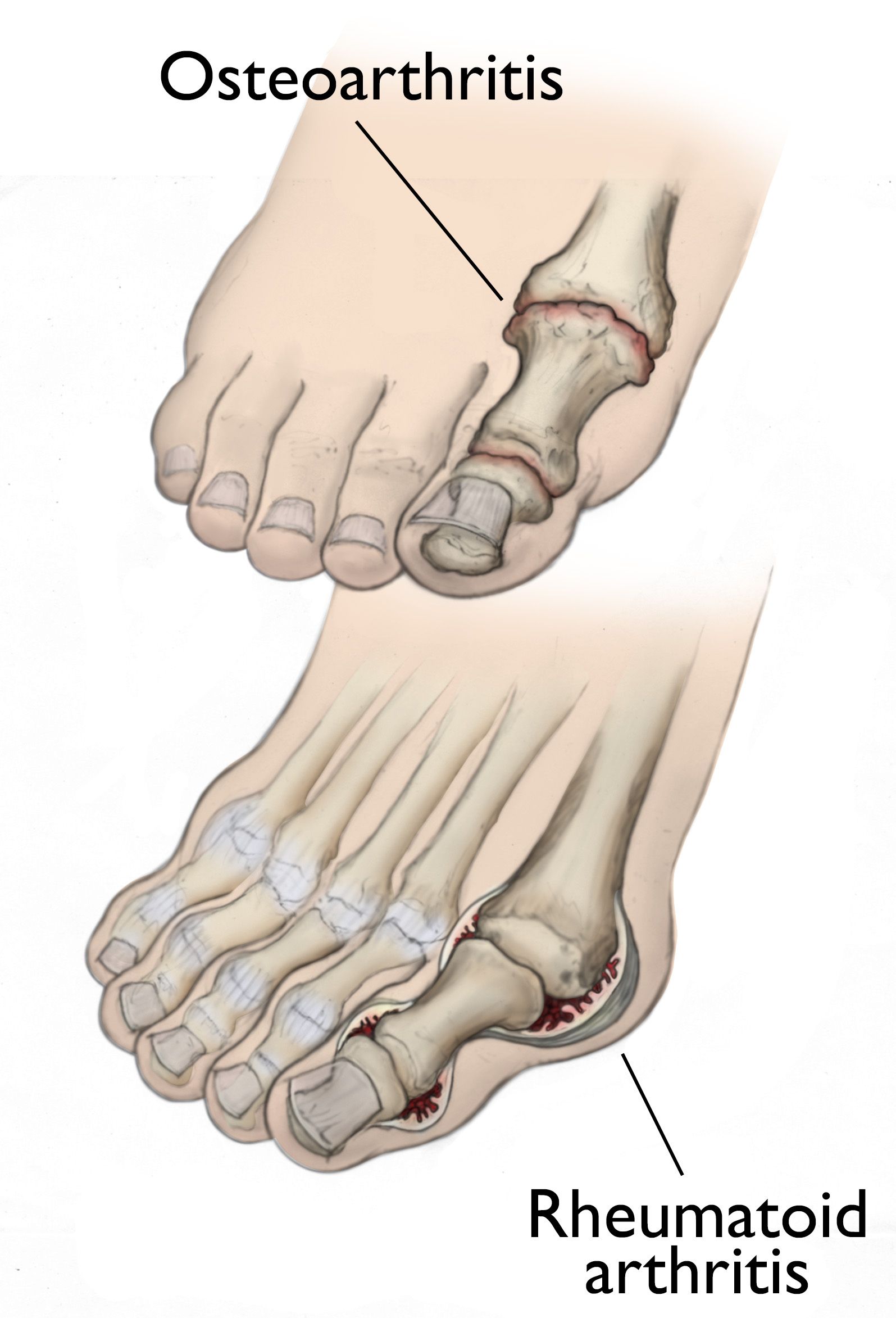
Osteoarthritis
Osteoarthritis, also known as degenerative or wear-and-tear arthritis, is a common problem for many people after they reach middle age, but it may occur in younger people, too.
In osteoarthritis, the cartilage in the joint gradually wears away. As the cartilage wears away, it becomes frayed and rough, and the protective space between the bones decreases. This can result in bone rubbing on bone and produce painful osteophytes (bone spurs).
In addition to age, other risk factors for osteoarthritis include obesity and family history of the disease.
Osteoarthritis develops slowly, causing pain and stiffness that worsen over time.
Rheumatoid Arthritis
Rheumatoid arthritis is a chronic disease that can affect multiple joints throughout the body, and often starts in the foot and ankle. It is symmetrical, meaning that it usually affects the same joint on both sides of the body.
Rheumatoid arthritis is an autoimmune disease. This means that the immune system attacks its own tissues. In rheumatoid arthritis, immune cells attack the synovium covering the joint, causing it to swell. Over time, the synovium invades and damages the bone and cartilage, as well as ligaments and tendons, and may cause serious joint deformity and disability.
The exact cause of rheumatoid arthritis is not known. Although it is not an inherited disease, researchers believe that some people have genes that make them more susceptible. There is usually a trigger, such as an infection or environmental factor, which activates the genes. When the body is exposed to this trigger, the immune system begins to produce substances that attack the joints.
Posttraumatic Arthritis
Posttraumatic arthritis can develop after an injury to the foot or ankle. Dislocations and fractures — particularly those that damage the joint surface — are the most common injuries that lead to post-traumatic arthritis. Like osteoarthritis, posttraumatic arthritis causes the cartilage between the joints to wear away. It can develop many years after the initial injury.
An injured joint is about seven times more likely than an uninjured joint to become arthritic, even if the injury is properly treated. In fact, following an injury, your body may actually secrete (release) hormones that stimulate the death of cartilage cells.
Symptoms
The symptoms of arthritis vary depending on which joint is affected. In many cases, an arthritic joint will be painful and inflamed. Generally, the pain develops gradually over time, although sudden onset is also possible. There can be other symptoms, as well, including:
- Pain with motion
- Pain that flares up with vigorous activity
- Tenderness when pressure is applied to the joint
- Joint swelling, warmth, and redness
- Increased pain and swelling in the morning, or after sitting or resting
- Difficulty walking due to any of the above symptoms
Doctor Examination
Physical Examination
Your doctor will:
- Discuss your overall health and medical history
- Ask about any medications you may be taking
- Examine your foot and ankle for tenderness and swelling
- Ask questions to understand more about your symptoms. such as:
- When did the pain start?
- Where exactly is the pain? Does it occur in one foot or in both feet?
- When does the pain occur? Is it continuous, or does it come and go?
- Is the pain worse in the morning or at night? Does it get worse when walking or running?
- Ask whether you have had an injury to your foot or ankle in the past
- If you have had a past injury, discuss your injury, including when it occurred and how it was treated
- Examine your shoes to determine whether there is any abnormal or uneven wear and to ensure that the shoes are providing sufficient support for your foot and ankle
Gait analysis
During the physical examination, your doctor will closely observe your gait (the way you walk). Pain and joint stiffness will change the way you walk. For example, if you are limping, the way you limp can tell your doctor a lot about the severity and location of your arthritis.
During the gait analysis, your doctor will:
- Assess how the bones in your leg and foot line up when you walk
- Measure your stride
- Test the strength of your ankles and feet
Tests
X-rays. X-rays provide detailed pictures of dense structures such as bone. An X-ray of an arthritic foot may show:
- Narrowing of the joint space between bones (a sign of cartilage loss),
- Changes in the bone (such as fractures)
- The formation of bone spurs
Weightbearing X-rays are taken while you stand. They are the most valuable additional test for diagnosing the severity of arthritis and noting any joint deformity associated with it. In arthritic conditions, if X-rays are taken when the patient is not standing, it is difficult to assess how much arthritis is present, where it is located in the joint, and how much deformity is present. So, it is very important that, when possible, X-rays are taken with the patient standing.
Other imaging tests. In some cases, a bone scan, computerized tomography (CT) scan, or magnetic resonance imaging (MRI) scan may be needed to determine the condition of the bone and soft tissues.
Laboratory tests. Your doctor may also recommend blood tests to determine which type of arthritis you have. With some types of arthritis, including rheumatoid arthritis, blood tests are important for an accurate diagnosis.
Your doctor may refer you to a rheumatologist if they suspect rheumatoid arthritis. Although your symptoms and the results from a physical examination and tests may be consistent with rheumatoid arthritis, a rheumatologist will be able to determine the specific diagnosis. There are other less common types of inflammatory arthritis that will be considered.
Treatment
There is no cure for arthritis, but there are a number of treatments that may help relieve the pain and disability it can cause.
Nonsurgical Treatment
Initial treatment of arthritis of the foot and ankle is usually nonsurgical. Your doctor may recommend a range of treatment options.
Lifestyle modifications. Some changes in your daily life can help relieve the pain of arthritis and slow the progression (worsening) of the disease. These changes include:
- Minimizing activities that aggravate the condition.
- Switching from high-impact activities (like jogging or tennis) to lower impact activities (like swimming or cycling) to lessen the stress on your foot and ankle.
- Losing weight to reduce stress on the joints, resulting in less pain and increased function.
Physical therapy. Specific exercises can help increase range of motion and flexibility, as well as help strengthen the muscles in your foot and ankle. Your doctor or a physical therapist can help develop an individualized exercise program that meets your needs and lifestyle.
Although physical therapy often helps relieve stress on the arthritic joints, in some cases it may worsen joint pain. This occurs when movement creates increasing friction between the arthritic joints. If your joint pain is aggravated by physical therapy, your doctor will stop this form of treatment.
Assistive devices. Wearing a brace — such as an ankle-foot orthosis (AFO) — may help improve mobility.
In addition, wearing shoe inserts (orthotics) or custom-made shoes with stiff soles and rocker bottoms can help minimize pressure on the foot and decrease pain. If deformity is present, a shoe insert may tilt the foot or ankle back into a straight position, creating less pain in the joint.
Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, can help reduce swelling and relieve pain.
A cortisone shot, or steroid injection, is a simple in-office procedure in which a steroid, like triamcinolone or methylprednisolone, is injected into a joint in combination with an anesthetic, like lidocaine or bupivacaine. Although it can provide pain relief and reduce inflammation for foot and ankle arthritis, the effects of a cortisone shot are often temporary.
Surgical Treatment
Your doctor may recommend surgery if your pain causes disability and is not relieved with nonsurgical treatment. The type of surgery will depend on the type and location of the arthritis and the impact of the disease on your joints. In some cases, your doctor may recommend more than one type of surgery.
Arthroscopic debridement. This surgery may be helpful in the early stages of arthritis. Debridement is a procedure to remove loose cartilage, inflamed synovial tissue, and bone spurs from around the joint.
During arthroscopy, your surgeon inserts a small camera, called an arthroscope, into your foot or ankle joint. The camera displays pictures on a monitor, and your surgeon uses these images to guide miniature surgical instruments. Because the arthroscope and surgical instruments are thin, your surgeon can use very small incisions, rather than the larger incision needed for a traditional, open surgery.
Arthroscopic surgery is most effective when pain is due to contact between bone spurs and the arthritis has not yet caused significant narrowing of the joint space between the bones. Arthroscopy can make an arthritic joint deteriorate more rapidly. Removing bone spurs may increase motion in the joint, causing the cartilage to wear away faster.
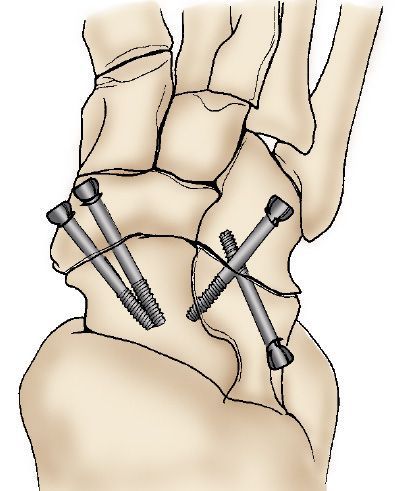
Arthrodesis (fusion). Arthrodesis fuses the bones of the joint completely, making one continuous bone out of two or more bones. The goal of the procedure is to reduce pain by eliminating motion in the arthritic joint.
During arthrodesis, the surgeon removes the damaged cartilage and then uses pins, plates and screws, or rods to fix the joint in a permanent position. Over time, the bones fuse, or grow together, just like two ends of a broken bone grow together as it heals. Since the bones no longer move, there should not be any more pain.
Arthrodesis is typically quite successful, although there can be complications.
- In some cases, the joint does not fuse together (nonunion), and the hardware may break. While the broken hardware does not cause pain, the nonunion of the fusion can lead to pain and swelling. If nonunion occurs, a second operation to place bone graft and/or new hardware may be needed. However, repeated fusions are not as likely to be successful, so it is best to closely follow your doctor's guidelines during the recovery period of your original operation.
- A small percentage of patients have problems with wound healing, but these problems can usually be addressed by local wound care (dressing changes) or by an additional surgery.
- In some cases, loss of motion after a fusion causes the joints around the one that is fused to bear more stress than they did before the surgery. This can lead to arthritis in the nearby joints years after the surgery.
Total ankle replacement (arthroplasty). In total ankle replacement, your surgeon removes the damaged cartilage and bone, then positions new metal or plastic joint surfaces to restore the function of the joint.
Although total ankle replacement is not as common as total hip or total knee replacement, advances in implant design have made it a viable option for many people.
Ankle replacement is most often recommended for patients who have:
- Advanced arthritis of the ankle
- Arthritis that has destroyed the ankle joint surfaces
- Ankle pain that interferes with daily activities
Ankle replacement relieves the pain of arthritis and offers patients more mobility and movement than fusion. In addition, being able to move the formerly arthritic joint means that less stress is transferred to the adjacent (nearby) joints. This decreases the chance of developing adjacent joint arthritis.
As in any type of joint replacement, an ankle implant may loosen or fail over the years. If the implant failure is severe, the replaced joint can be exchanged for a new implant — this procedure is called a revision surgery.
Another option is to remove the implant and fuse the joint. This type of fusion is more difficult than when fusion is done as the initial procedure. When the implant is removed, there is space in the bone that must be filled with bone graft to maintain the length of the leg. Because the new bone may not be as strong, the risk of nonunion is greater.
Recovery
In most cases, surgery relieves the pain of arthritis and makes it easier to perform daily activities. Full recovery can take 4 to 9 months, depending on the severity of your condition before surgery and the complexity of your procedure.
Foot and ankle surgery can be painful. While you should expect to feel some discomfort, advances in pain control now make it easier for your doctor to manage and relieve pain. Immediately after surgery, you will be given medication for pain relief. If needed, your doctor will provide you with a pain reliever that you can take for a short time while you are home.
Your doctor will most likely apply a cast after surgery to limit movement in your foot and ankle and to prevent nonunion. To reduce swelling, it is important to keep your foot elevated above the level of your heart for 1 to 2 weeks after surgery.
Later in your recovery, your doctor may recommend physical therapy to help you regain strength in your foot or ankle and to restore range of motion.
In most cases, you will be able to resume your daily activities in 3 to 4 months, although, you may need to wear supportive shoes or a brace for a period of time.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.