Diseases & Conditions
Ankylosing Spondylitis
Anatomy
Ankylosing spondylitis can affect:
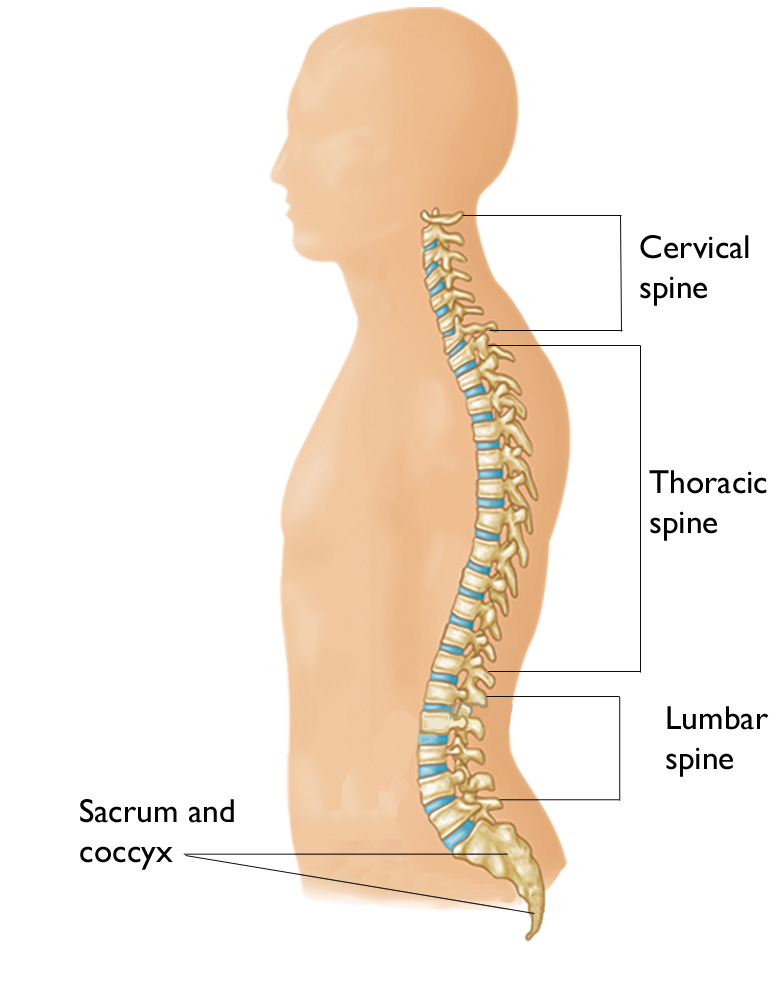
- The bones and tissues surrounding your spine and pelvis. The sacroiliac joint is one area where changes from the disease can be seen first. The sacroiliac joints connect the lower triangular base of the spine (the sacrum) to part of the pelvis (the ilium).
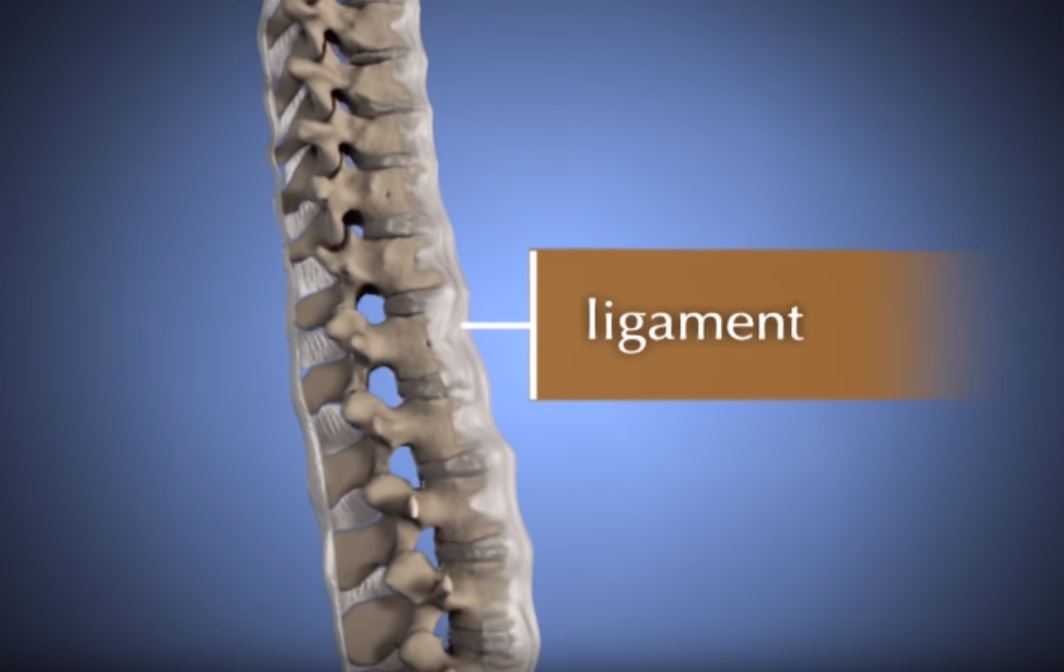
- The entheses. Entheses are the connecting points between bones and ligaments, tendons, or joints. These areas can become inflamed. For example, the Achilles tendon in the heel can hurt and become stiff.
- The eyes, in a condition called uveitis. This is when the immune system attacks the uvea, or the middle layer of the eye, including the iris. If the uvea is inflamed, it makes the eye red, painful, and sensitive to light.
Description
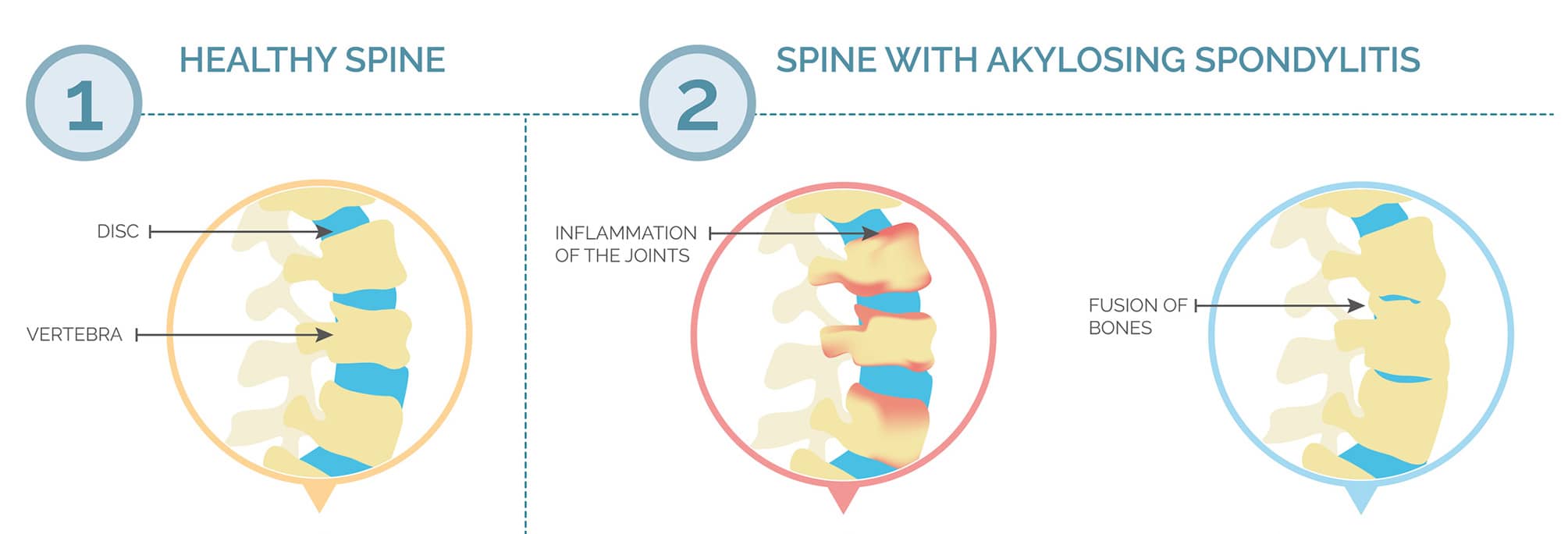
- At first, ankylosing spondylitis can cause small changes that show up on X-rays but do not cause symptoms.
- Over time, ankylosing spondylitis can make the bones in your back grow together, called fusion, which can make it hard to move.
Cause
- Sex. Men get ankylosing spondylitis about twice as often as women do.
- Family history. Having a close relative with ankylosing spondylitis makes it more likely that you might develop AS also. Immediate family (parents, siblings, and children) with AS have the most impact on your risk of developing AS, while other family members like grandparents, aunts, and uncles have a smaller impact on your risk. Ankylosing spondylitis is probably passed down between families through a gene called HLA-B27. There are more than 100 other genes that are also linked to ankylosing spondylitis. However, not everyone with these genes will end up with ankylosing spondylitis. Scientists think this is because several risk factors add together to determine whether you develop ankylosing spondylitis.
- Tobacco use. Smoking (including e-cigarettes/vaping) puts you at risk of developing ankylosing spondylitis. Learn more: Smoking and Musculoskeletal Health
- Physically demanding work. People with ankylosing spondylitis who have more physically demanding jobs may have more pain and faster changes in their spine than people with less physical jobs.
- Vitamin D. People who have higher levels of vitamin D may have a lower chance of getting ankylosing spondylitis. Learn more: Vitamin D for Good Bone Health
- Gut microbiome. Bacteria in your gut may also affect your risk of developing ankylosing spondylitis. This may be a way to treat ankylosing spondylitis in the future as doctors and scientists better understand the role gut bacteria may play in disease development.
Symptoms
- Back pain and stiffness. This pain usually starts in early adulthood (before age 45). People with ankylosing spondylitis typically have back pain and stiffness that is worse in the morning and may wake them up at night. This pain gets better with exercise.
- Neck pain and stiffness. Similar to back pain, this can be worse first thing in the morning (right after waking up) and get better with exercise.
- Fatigue. Many people with ankylosing spondylitis have overwhelming tiredness that can come and go.
- Less flexibility in the spine . Moving the spine can be harder because of pain and stiffness in the back and hips. The vertebrae in the spine can fuse together. This can make it harder to bend over or for the spine to move.
- Pain in areas outside of the back. The hips, knees, or shoulders can sometimes be affected.
- Enthesitis. Pain and stiffness may develop at attachment points for tendons, ligaments, and joint capsules (for example, the heel, knee, hip, elbow, and spine).
- Red, painful, and sensitive eyes. Some people with ankylosing spondylitis can develop anterior uveitis. This is a condition where the immune system attacks the middle layer of the eye, including the iris.
- Digestive symptoms. People with AS can develop diarrhea or constipation, blood in stools, abdominal pain, cramping pain, heartburn, or other digestive symptoms. About 5 to 10% of people with ankylosing spondylitis have inflammatory bowel disease (IBD) as well.
- Broken vertebrae and neurologic complications. Ankylosing spondylitis often causes osteoporosis since the inflammation can wear away healthy bone over time. This makes it more likely for people with AS to have fractures in their spine and sometimes severe problems with the nervous system.
- Heart problems. In rare cases, inflammation caused by AS can affect the heart. This can lead to high blood pressure, problems with the aorta or aortic valves, or problems with the electric signals to the heart (such as an abnormal heartbeat, or arrhythmia).
Doctor Examination
Medical History and Physical Examination
Imaging Tests
Treatment
Nonsurgical Treatment
- TNF inhibitors sometimes cause cough, stomach pain, or fatigue.
- IL-17 inhibitors sometimes cause diarrhea or make inflammatory bowel disease worse.
- All these medications can increase your risk of infections since they affect the immune system.
- You may need to be tested for tuberculosis before beginning these medications, since these medications can cause tuberculosis to become active again in people who already have tuberculosis.
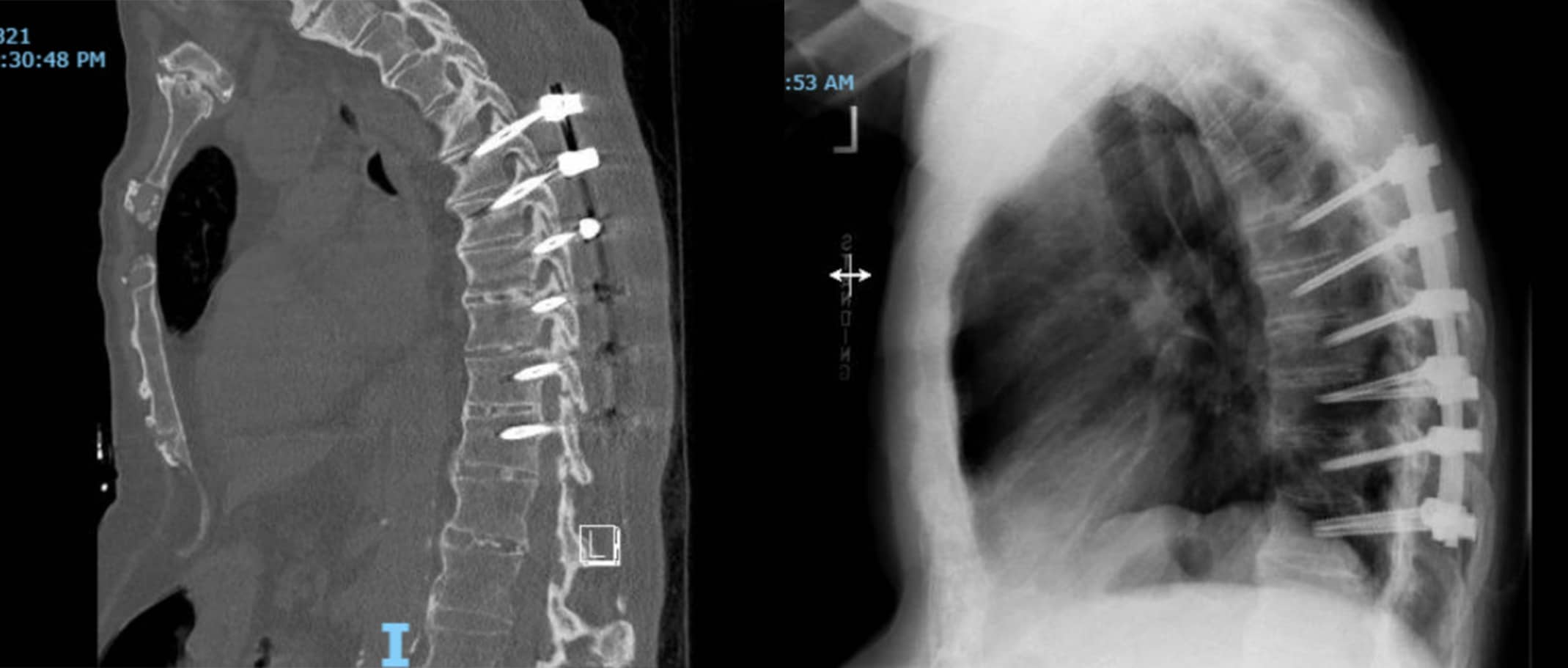
Surgical Treatment
- Surgery is important if the bones in the spine become unstable, press on a nerve, or cause severe curves in your spine.
- Likewise, surgery is important if you begin to experience difficulty breathing or swallowing.
- Another reason surgery may be performed is if you have severe pain that stops you from being able to do your daily tasks and other therapies do not help.
Conclusion
- While there is not a cure for AS, most people with AS are able to have a good quality of life and continue to do the things that are important to them.
- Early nonsurgical treatments, such as anti-inflammatory medications, physical therapy, and lifestyle changes, can make a big impact on how your symptoms change over time. Focus on eating a well-balanced diet, managing stress, getting regular exercise, and getting enough sleep. And if you smoke or vape, take steps to quit.
- Your doctor may prescribe medications, such as biologics, to help keep you active and control symptoms.
- Surgical treatments are usually not necessary, but surgery may be a good option if you have severe problems with your spine.
- With the treatments available today, a person with AS typically has the same life expectancy as someone without the disease. However, some life-threatening problems can arise with AS, such as cardiovascular disease and spinal fractures, so it is important to get regular medical care in addition to managing your AS symptoms.
Managing a chronic disease is not easy. Be open with your treatment team about the symptoms you are experiencing and seek support from loved ones and/or a support group.
Reference for Risk Factors of Ankylosing Spondylitis: Hwang MC, Ridley L, Reveille JD. Ankylosing spondylitis risk factors: a systematic literature review. Clin Rheumatol. 2021 Aug;40(8):3079-3093.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.