Diseases & Conditions
Acetabular Fractures
An acetabular fracture is a break in the socket portion of the "ball-and-socket" hip joint. These hip socket fractures are not common — they occur much less frequently than fractures of the upper femur or femoral head (the "ball" portion of the joint).
The majority of acetabular fractures are caused by some type of high-energy event, such as a motor vehicle collision. Often, patients will have additional injuries that require immediate treatment.
In a smaller number of cases, a low-energy incident, such as a fall from standing, may cause an acetabular fracture in an older person who has weaker bones. People with osteoporosis are at increased risk of acetabular fractures from low-energy incidents.
Treatment for acetabular fractures often involves surgery to restore the normal anatomy of the hip and stabilize the hip joint.
Anatomy
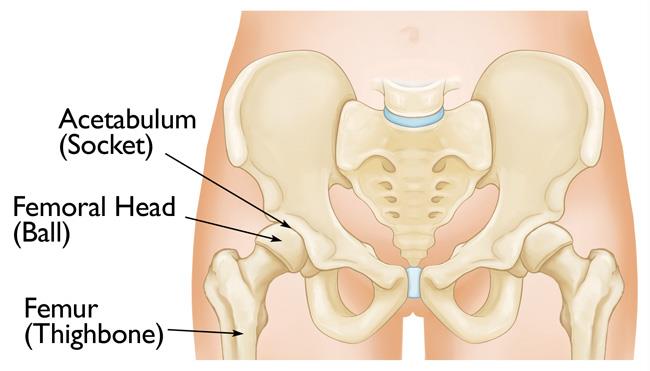
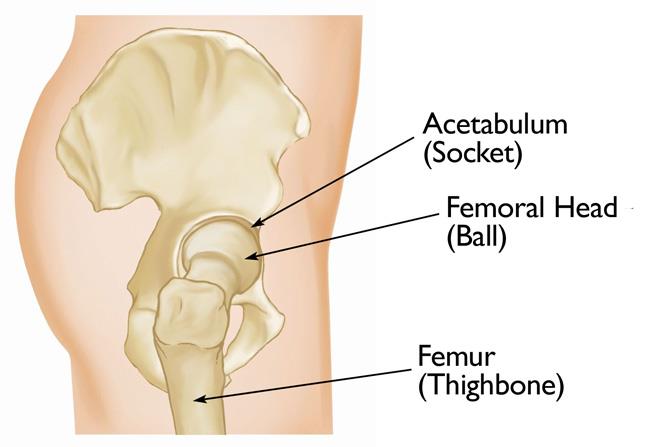
The hip is one of the body's largest joints. It is a "ball-and-socket" joint.
- The socket is formed by the acetabulum, which is part of the pelvis.
- The ball is the femoral head, which is the upper end of the femur (thighbone).
The bone surfaces of the ball and socket are covered with articular cartilage — a smooth, slippery substance that protects and cushions the bones and enables them to move easily.
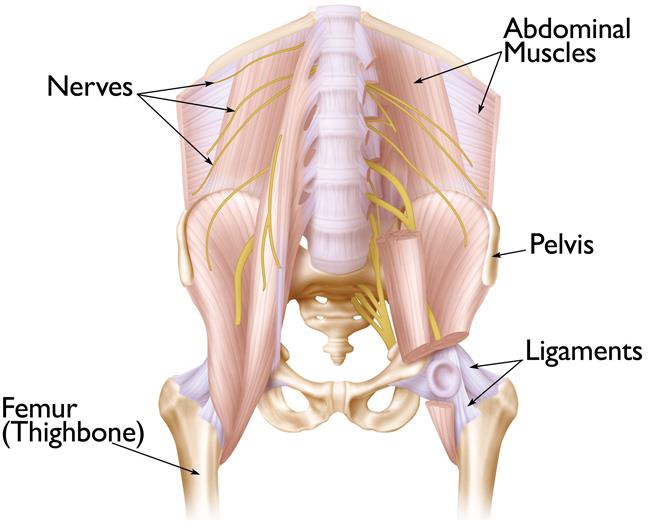
Bands of tissue called ligaments connect one bone to another. These ligaments help provide both function and stability to the hip joint, allowing it to move without falling out of the socket.
Description
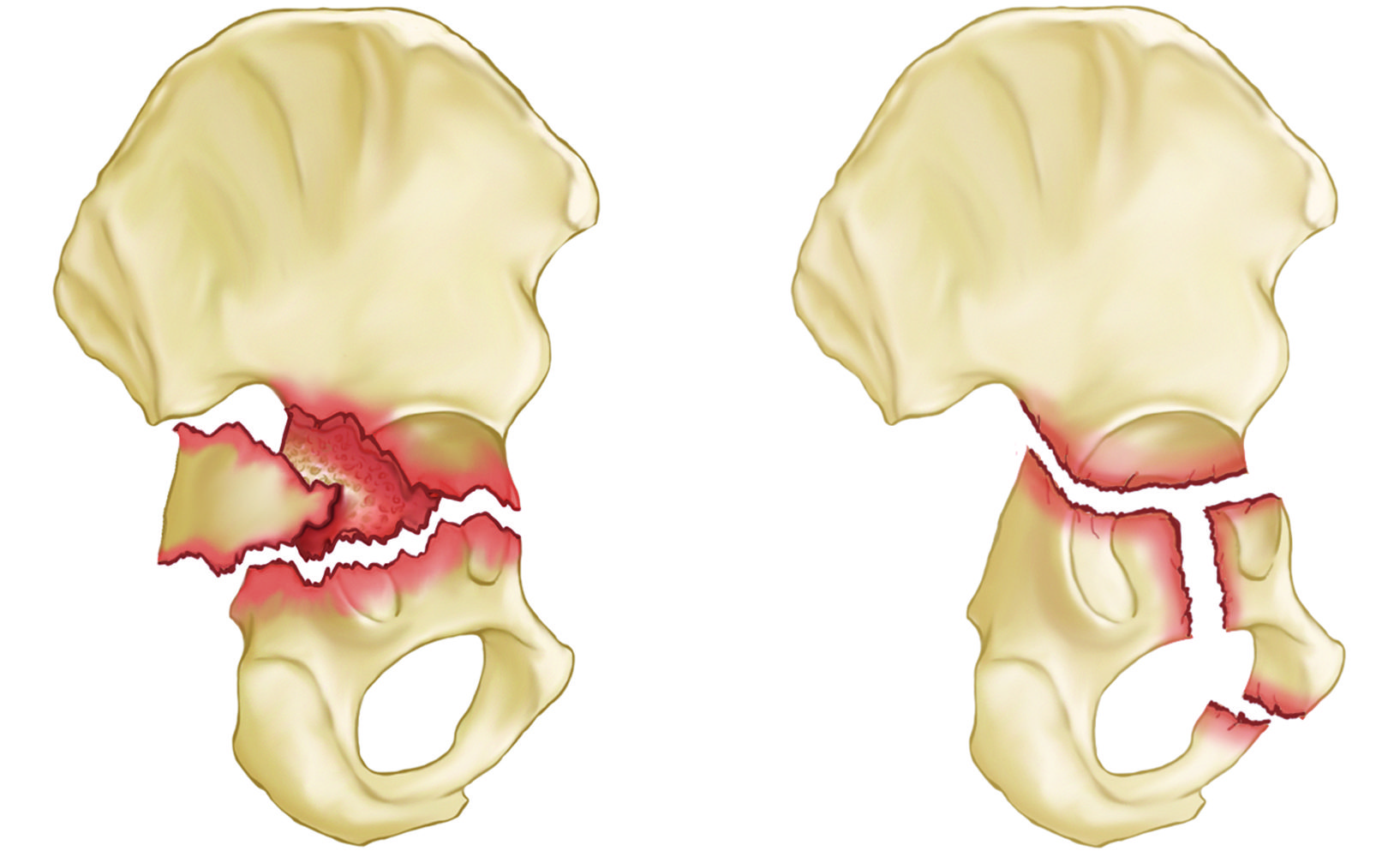
Acetabular fractures vary. For example, the bone can break straight across the socket or shatter into many pieces. When the acetabulum is fractured, the femoral head may no longer fit firmly into the socket, and the cartilage surface of both bones may be damaged.
If the joint remains irregular or unstable, ongoing cartilage damage to the surfaces may lead to arthritis.
Severity
The severity of the injury depends on several factors, including:
- The number and size of the fracture fragments
- The amount each piece is out of place (displaced) — in some cases, the broken ends of bones line up adequately; in more severe fractures, there may be a large gap between the broken pieces, or the fragments may overlap each other
- The damage to the cartilage surfaces of both the acetabulum and the head of the femur
- The damage to surrounding muscle, tendons, nerves, and skin
Pattern of Injury
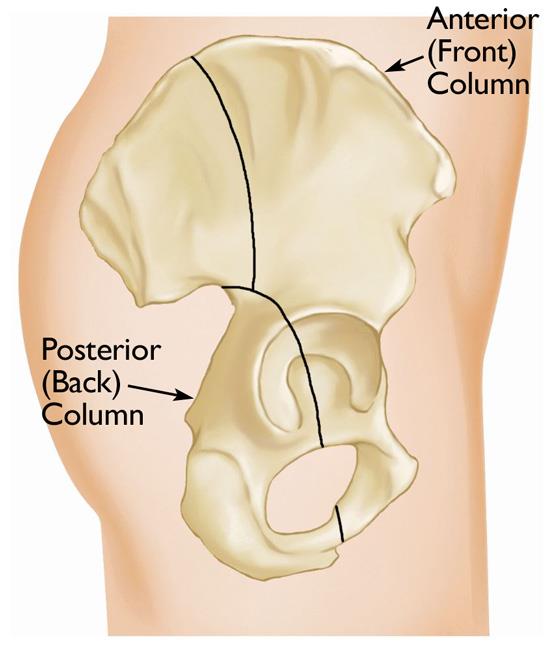
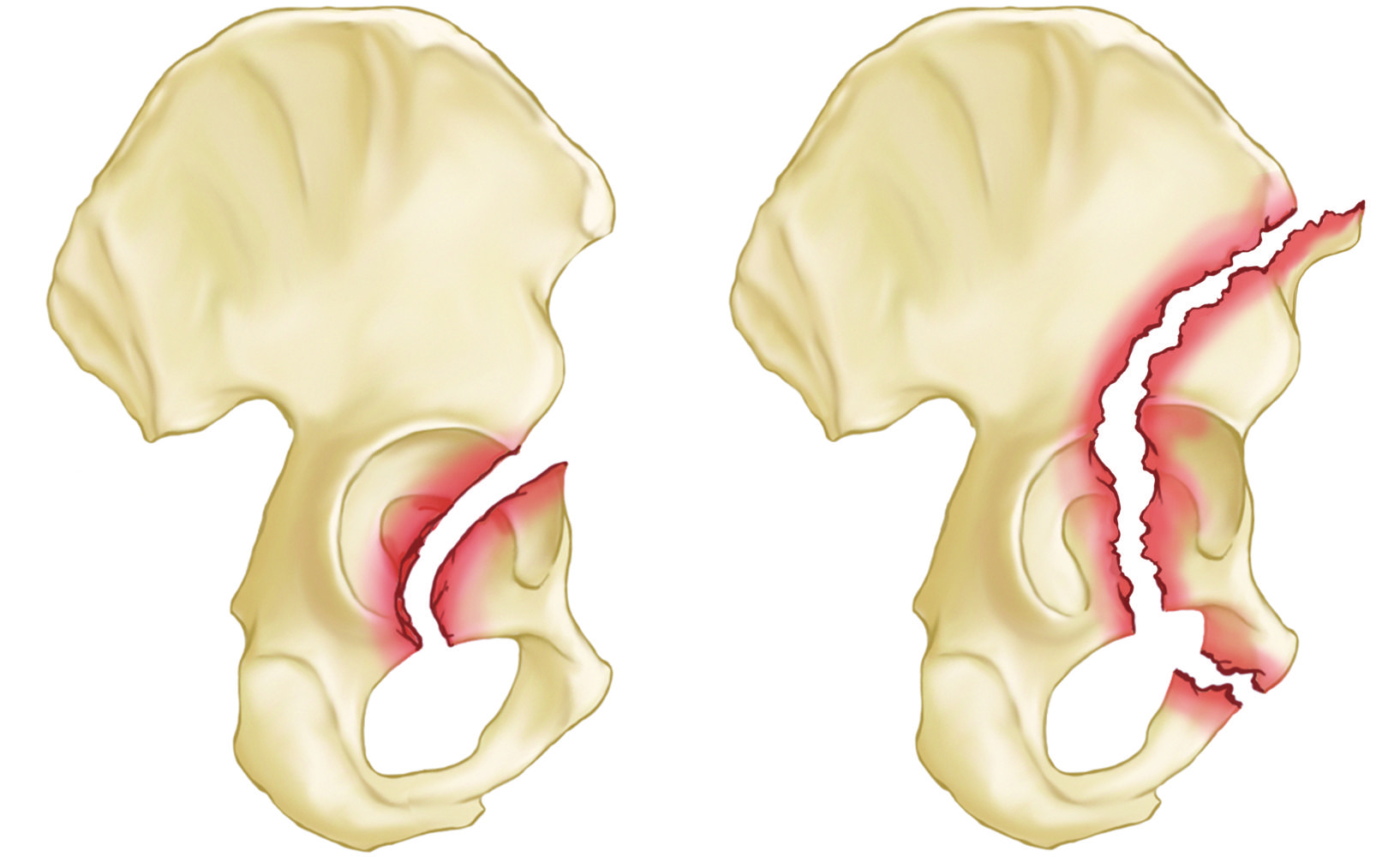
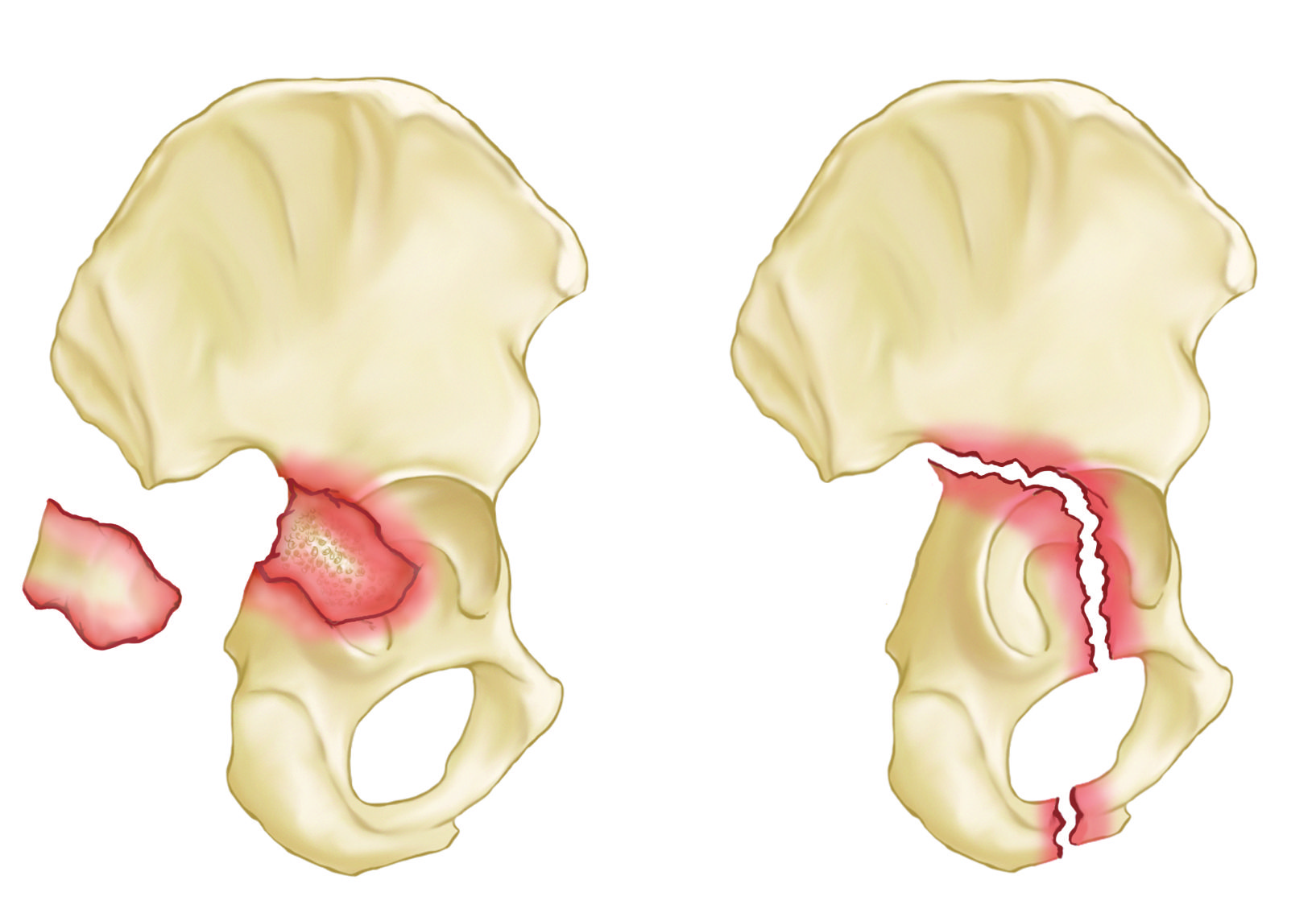
The anatomy of the pelvis provides bony support for both the front (anterior) and back (posterior) of the hip socket. Orthopaedic surgeons have identified a number of different acetabular fracture patterns. These fracture patterns are based on:
- Location — such as a break in the anterior (front) or posterior (back) column of the bone or the area around the bony rim (wall) of the acetabulum
- Orientation — such as a break that is straight across the bone
Acetabular fractures can also occur in a combination of patterns. Knowing the severity and specific pattern of your fracture will help your doctor determine the most appropriate treatment.
Common acetabular fracture patterns include:
Cause
An acetabular fracture occurs when a force drives the head of the femur against the acetabulum. This force can be transmitted:
- From the knee (such as hitting the knee against the dashboard in a head-on car collision)
- From the side (such as falling off a ladder directly onto the hip).
Depending on the direction of the force, the head of the femur is sometimes pushed out of the hip socket, an injury called hip dislocation.
When the fracture is caused by high-energy impact, patients may have other serious injuries that require urgent attention.
Acetabular fractures are sometimes caused by weak or insufficient bone. This is most common in older patients whose bones have become weakened by osteoporosis. Although these patients do not often have other injuries, they may have complicating medical problems, such as heart disease or diabetes.
Symptoms
A fractured acetabulum is almost always painful. The pain is typically localized (limited) to the groin or hip area and is worsened with movement.
If nerve damage has occurred with the injury, the patient may feel numbness, weakness, or a tingling sensation down the leg.
Doctor Examination
Emergency Stabilization
Patients with fractures caused by high-energy trauma will almost always go or be brought to an emergency room for initial treatment because of the severity of their symptoms.
Additionally, patients with these injuries often have other injuries, including those to the head, chest, abdomen, or legs.
Physical Examination
Your doctor will:
- Perform a thorough examination of your pelvis, hips, and legs.
- Check to see if you can move your ankles and toes, and whether you feel sensation on the bottom of your feet. In some cases, nerves may be injured at the same time that the acetabulum is fractured.
- Carefully examine the rest of your body to determine if you have any other injuries.
Imaging Tests
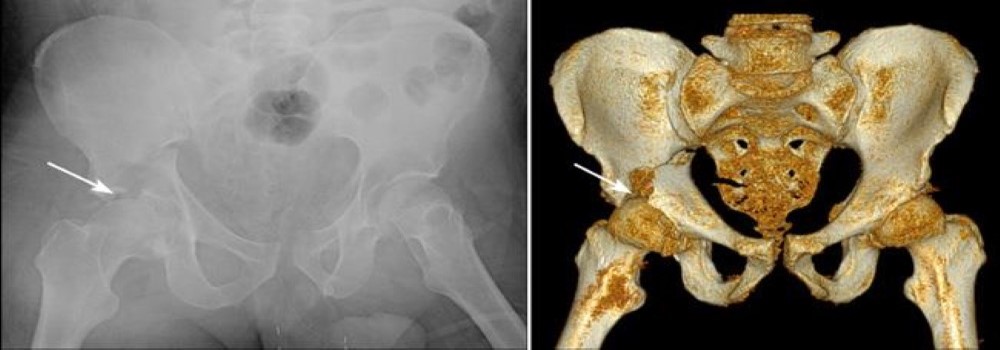
X-rays. X-rays provide images of dense structures, such as bones. X-rays of acetabular fractures are taken from a number of different angles to show the pattern of the fracture and how out of place (displaced) the bones are.
Computed tomography (CT) scan. Because of the complex anatomy of the pelvis, a CT scan is commonly ordered for acetabular fractures. The CT scan will provide your doctor with a more detailed, cross-sectional image of your hip and can be helpful in preoperative planning.
Treatment
Your orthopaedic surgeon will consider several things when planning your treatment, including:
- The specific pattern of the fracture
- How much the bones are out of position (displaced)
- Your overall health condition, including whether you have osteoporosis or any other medical conditions, such as heart disease or diabetes
Nonsurgical Treatment
Nonsurgical treatment may be recommended for
- Stable fractures in which the bones are not too far out of position (displaced).
- Patients who are at higher risk of surgical complications. For example, patients with severe osteoporosis, heart disease, diabetes, or other medical concerns may not be able to tolerate surgery.
Nonsurgical treatment may include:
- Walking aids. To avoid bearing weight on your leg, your doctor may recommend that you use crutches or a walker for up to 3 months — or until your bones are fully healed.
- Positioning aids. If your doctor is concerned about joint instability — the ball of your hip sliding within or popping out of the socket — they may restrict the position of your hip, limiting how much you are allowed to bend it. A leg-positioning device, such as an abduction pillow or knee immobilizer, can help you maintain these restrictions.
- Medications. Your doctor may prescribe medication to relieve pain, as well as an anti-coagulant (blood thinner) to reduce the risk of blood clots forming in the veins of your legs.
Surgical Treatment
Most acetabular fractures are treated with surgery. Because acetabular fractures damage the cartilage surface of the bone, an important goal of surgery is to restore a smooth, gliding hip surface by piecing the broken bones back together. This type of reconstruction is called open reduction internal fixation.
In some cases, rather than putting the bones back together, a better treatment option may be a hip replacement.
While you are in the hospital and prior to surgery, your surgeon may place your leg in skeletal traction to immobilize the fracture and prevent additional injury or damage to the hip socket.
In skeletal traction, a metal pin is temporarily placed through the femur or tibia bone. Weights attached to the pin gently pull on the leg, keeping the broken bone fragments in as normal a position as possible. For many patients, skeletal traction also provides some pain relief.
Open Reduction and Internal Fixation
During surgery, the displaced bone fragments are first repositioned (reduced) into their normal alignment. Your surgeon will then attach metal plates and screws to the outer surfaces of the bone to hold the fragments together while they heal.
Depending on the location of your fracture, your surgeon will make an incision along the front, side, or back of your hip. Occasionally, a combination of approaches or an alternative approach is used.
Total Hip Replacement
In some cases, the acetabulum is so damaged that repair or reconstruction is unlikely to be successful. In this situation, your surgeon may recommend total hip replacement. In this procedure, the damaged bone and articular cartilage are removed and replaced with artificial parts (prosthesis).
- Whenever possible, the surgeon will reposition the bones into their normal alignment using screw and plate fixation before performing the total hip replacement.
- However, if this is not possible, the surgeon may delay the procedure for a period of time to allow the fracture to first heal in its unaligned position. They will then perform the total hip replacement — replacing the irregular hip socket with the total hip prosthesis.
Your surgeon will consider many factors, including your age and activity level, in determining whether total hip replacement is the most appropriate treatment.
Recovery
Pain Management
After surgery, you will feel some pain. This is a natural part of the healing process. Your doctor and nurses will work to reduce your pain, which can help you recover from surgery faster.
Medications are often prescribed for short-term pain relief after surgery. Many types of medicines are available to help manage pain, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics. Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids.
Be aware that although opioids help relieve pain after surgery, they are narcotics and can be addictive. Opioid dependency and overdose have become critical public health issues in the U.S. It is important to use opioids only as directed by your doctor and to stop taking them as soon as your pain begins to improve. Talk to your doctor if your pain has not begun to improve within a few days of your surgery.
Weightbearing
Most patients require crutches or a walker for a period of time and will be limited in the ability to put full weight on the injured leg. This restriction can be for up to 3 months, depending on the severity of the injury. You may require the use of a cane or a walking aid for a longer period of time.
It is important to follow your doctor's specific instructions for weightbearing. Walking on your injured leg prior to healing or participating in physical activities too soon may cause the fracture to shift. This can lead to unevenness in the hip socket or recurrent instability in the hip joint.
Physical Therapy
Despite weightbearing restrictions, your doctor may encourage early movement. This means getting up out of bed and doing as much as possible within specific weightbearing limitations. In many cases, a physical therapist will provide instructions on how to safely begin moving and use crutches or a walker.
Over time, you will learn other exercises to help you build strength and endurance so that you are better able to perform your daily activities.
Sports and Fitness Activities
If your goal is to resume sports or fitness activities, your doctor will guide you in a gradual progression to more vigorous activities. It is important to be aware that due to the complicated nature of many acetabular fractures, many patients are not able to return to pre-injury levels of activity.
Your doctor will tell you when it is safe to begin low-impact activities, such as swimming and/or riding a stationary bicycle. However, it can take 6 to 18 months to return to more vigorous sports activities, such as running.
Complications
Even when surgery is successful, some patients will experience complications that may lead to the need for additional surgery.
Infection
Although advances in treatment and sterile surgical techniques continue to help prevent infections following surgery, surgical site infections do sometimes occur.
These infections may develop near the skin surface around an incision or deep in the surgical wound.
- Surface infections are typically treated with antibiotics for 1 to 2 weeks.
- Deeper infections can cause further healing complications and may lead to infections that are difficult to cure. They usually require a surgical procedure to thoroughly cleanse the wound as well as a longer course (usually 4 to 6 weeks) of antibiotics.
Blood Clots
Your mobility after surgery will be limited. This can slow the normal blood flow in your legs and increase your risk for a blood clot. In some cases, a blood clot can break free from the vein wall and travel to the lungs. This is called a pulmonary embolism, and it can be life-threatening.
Your doctor may prescribe a blood thinner to help prevent blood clots from forming in the deep veins of your legs.
Learn more about steps your surgical team takes to prevent blood clots after orthopaedic surgery.
Posttraumatic Arthritis
Even when treated successfully, acetabular fractures can damage the smooth surface of the joint, making it more likely that hip arthritis will develop during recovery or even years after an injury. Over time, the articular cartilage that protects the joint wears away, leading to increasing pain and stiffness.
- Posttraumatic arthritis can be treated like other forms of osteoarthritis — with physical therapy, walking aids, medications, and lifestyle changes.
- In severe cases that limit activity, a total hip replacement may be the best option to relieve symptoms.
Sciatic Nerve Injury
The sciatic nerve is a large nerve that passes near the back of the hip socket. It supports motion and sensation in the leg and foot. The sciatic nerve can be injured or damaged during the initial injury or during surgery.
Most often, injury to the sciatic nerve results in "foot drop," a condition in which the patient is not able to lift the ankle or toes from the floor when walking. Nerve injuries can range in severity, and the amount of recovery can vary.
Heterotopic Ossification
A rare problem that may occur after surgery is the growth of bone in the muscles, tendons, and ligaments around the hip socket. This is called heterotopic ossification.
When this happens, bone grows where it should not be. This can cause stiffness not directly related to the condition of the hip socket cartilage. If the amount of extra bone is great enough to interfere with hip flexibility and function, your doctor may recommend surgery to remove it.
Avascular Necrosis (Osteonecrosis)
Blood flow to the bone can be disrupted at the time of the injury. Even with successful surgical repair, if the normal blood flow and nutrition necessary to keep bone healthy is disrupted, the bone cells will die. This condition is called avascular necrosis, or osteonecrosis.
An acetabular fracture can lead to avascular necrosis in the femoral head as well as the acetabulum. As the bone cells die, the bone gradually crumbles and collapses, along with the smooth cartilage protecting it. Without this smooth cartilage, bone rubs against bone, leading to increased pain, arthritis, and loss of motion and function.
Outcomes
It typically takes 9 to 12 months for an acetabular fracture to completely heal. The outcomes of treatment will vary from patient to patient, depending on:
- The pattern and severity of the fracture.
- Other injuries associated with the trauma.
- The patient's age and bone quality.
- The patient's general health, including whether they smoke. Research indicates that smoking can slow down bone healing and increase the risk for other complications. Learn more: Smoking and Musculoskeletal Health
Due to the serious nature of acetabular fractures — as well as the likelihood of developing long-term complications — many patients are not able to return to the same level of activity they had before their injury.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.