Diseases & Conditions
Rotator Cuff Tears: Frequently Asked Questions
What is the rotator cuff, and what does it do?
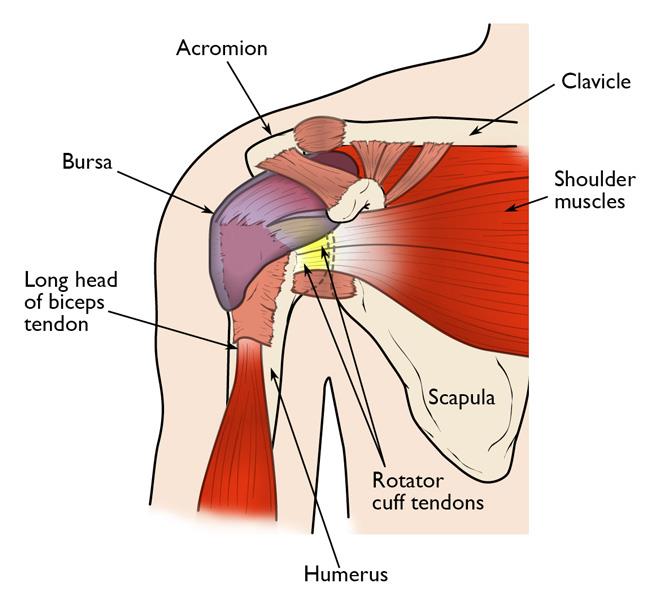
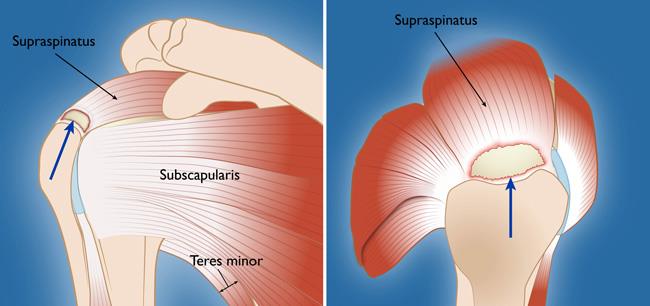
The rotator cuff is a group of four muscles that come together as tendons to form a "cuff," or cover, over the head of the humerus (upper arm bone).
The four muscles — supraspinatus, infraspinatus, subscapularis and teres minor — originate from the scapula (shoulder blade). The rotator cuff tendons attach to the head of the humerus in bony spots referred to as the greater and lesser tuberosities.
The rotator cuff helps to lift and rotate the arm and to stabilize the ball of the shoulder within the joint.
What causes a rotator cuff tear, and how would I know if I have one?
A rotator cuff tear may result from an acute injury, such as a fall, or may be caused by normal aging-related wear and tear with degeneration of the tendon.
- Typically, you will feel pain in the front of your shoulder that radiates down the side of your arm. It may be present with overhead activities such as lifting or reaching (e.g., serving in tennis, painting a ceiling).
- You may feel pain when you try to sleep on the affected side.
- You may note weakness of your arm and difficulty with routine activities such as combing your hair or reaching behind your back.
- If the tear occurs with injury, you may experience acute pain, a snapping sensation, and immediate weakness of the arm.
If I have a painful rotator cuff and keep using it, will this cause further damage?
A rotator cuff tear can extend or get larger over time. This can occur normally over time, or with repetitive use or a re-injury. It is common for patients with known rotator cuff disease to have acute pain and weakness following a minor injury. This likely represents extension of an existing tear.
If you know you have a rotator cuff tear, worsening pain and decreasing strength may mean the tear is getting larger.
When should I see a doctor for a rotator cuff tear?
If you have injured your shoulder or have chronic shoulder and arm pain, it is best to see an orthopaedic surgeon. They can then make a diagnosis and begin treatment. Your doctor may recommend a diagnostic imaging study such as a magnetic resonance imaging (MRI) scan or ultrasound to confirm the diagnosis.
Early diagnosis and treatment of a rotator cuff tear may prevent symptoms such as loss of strength and loss of motion from setting in.
If your primary physician has already made the diagnosis, an orthopaedic surgeon can review both surgical and nonsurgical options and start treatment.
Can a rotator cuff tear be healed or strengthened without surgery?
The majority of rotator cuff tears can be treated nonsurgically using one or more of these treatments:
- Anti-inflammatory medications
- Steroid (cortisone) injections
- Physical therapy
The goals of treatment are to relieve pain and restore strength to the involved shoulder.
Even though most tears cannot heal on their own, you can often achieve good function without surgery.
If, however, you are active or use your arm for overhead work or sports, surgery is most often recommended because many tears will not heal without surgery.
At what point does a rotator cuff tear require surgery to fix it?
Surgery is recommended:
- If you have persistent pain or weakness in your shoulder that does not improve with nonsurgical treatment. Frequently, patients who require surgery will report pain at night and difficulty using the arm for lifting and reaching. Many will report ongoing symptoms despite several months of medication and limited use of the arm.
- In active individuals who use the arm for overhead work or sports. Pitchers, swimmers, and tennis players are common examples.
Additionally, surgery may be recommended for complete tears that are acute and due to a trauma.
What options are available for surgical repair?
The type of repair performed is based on the findings at surgery.
- A partial tear may require only a trimming or smoothing procedure called a débridement.
- A full-thickness tear, which usually means the tendon is torn from its insertion on the humerus (the most common injury), is repaired directly to bone.
Three techniques are used for rotator cuff repair:
- Traditional open repair
- Mini-open repair
- Arthroscopic repair
Your orthopaedic surgeon can recommend which technique is best for you.
How important is rehabilitation in the treatment of a rotator cuff tear?
Rehabilitation plays a critical role in both the nonsurgical and surgical treatment of a rotator cuff tear.
When a tear occurs, there is frequently atrophy of the muscles around the arm and loss of motion of the shoulder. An exercise or physical therapy program is necessary to regain strength and improve function in the shoulder.
After surgery, the repair must be protected from certain activities that may put healing at risk. As such, a therapist can provide a safe and progressive therapy program.
Even though surgery repairs the defect in the tendon, the muscles around the arm remain weak, and a strong effort at rehabilitation is necessary for the procedure to succeed. Complete rehabilitation after surgery may take several months or even up to a year.
Your orthopaedic surgeon can prescribe an appropriate program based on your needs and the findings at surgery.
Last Reviewed
June 2022
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.