Diseases & Conditions
Heat Injury and Heat Exhaustion
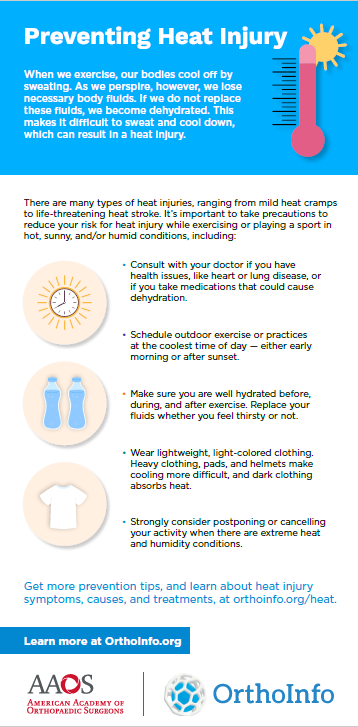
There are many types of heat injury, ranging from mild heat cramps to life-threatening heat stroke.
A growing number of children and young adults are playing sports during late summer and early fall. According to the Centers for Disease Control and Prevention, heat illness during practice or competition is a leading cause of death and disability among U.S. high school athletes. As more people exercise in warm conditions, it's essential to take proper precautions.
Heat-related illnesses are preventable. Prevention begins with understanding the causes of heat illness, and making sure to stay cool and hydrated during hot weather. In addition, knowing the signs of heat injury and being able to treat it immediately will reduce the number of severe cases.
Cause
When we exercise, our bodies cool off by sweating. As we perspire, we lose necessary body fluids. If we do not replace these fluids, we become dehydrated. This makes it difficult to sweat and cool down, which can result in a heat injury.
During regular exercise, 70 to 90% of the energy our bodies produce is released by heat. Many factors can hinder heat release and perspiration. These include:
- Environment. Air temperature, combined with humidity, wind speed, and sun affect how well our bodies cool themselves. Humidity influences how easily sweat can evaporate. High humidity (greater than 60%) makes sweat evaporation very difficult.
- Clothing. Dark clothing absorbs heat. This can dramatically increase the chance of heat stress. Full body clothing, heavy pads, and helmets make cooling more difficult.
- Sun exposure. Direct exposure to the sun with no available shade can increase your core body temperature.
- Fitness level/acclimatization. Before exercising in the heat, athletes must be in good physical condition. They also need to give their bodies time to adjust to warmer temperatures.
- Age. Children adjust to heat more slowly than adults. Their bodies are less effective at regulating body heat.
- Dehydration. Even mild levels of dehydration (3 to 5% of body weight) can hurt athletic performance. If you have not had enough fluids, your body will not be able to effectively cool itself through sweat and evaporation.
- Pre-activity hydration status. Athletes who start activities in an already dehydrated state are at greater risk for heat injury. Factors that can affect your pre-activity hydration status include inadequate rehydration after a previous exercise session, excessive caffeine or alcohol consumption, rapid weight loss regimes (i.e., wrestling), and fever, vomiting, or diarrhea.
- High body fat. Athletes with high body fat have greater difficulty cooling themselves.
- Fever. Anyone with a current or recent fever may be at increased risk.
- Medications. Diuretics and stimulants may increase risk.
- Sickle cell trait. Sickle cell trait or disease increases the risk for heat illness. This is especially true if good hydration and electrolytes are not maintained.
Mild Heat Injury
Heat Cramps
Heat cramps are painful cramps in the stomach, arm, and leg muscles. These cramps are caused by not replacing salt and fluids during intense, prolonged exercise in the heat.
Treatment for Heat Cramps
- Stop exercise activity
- Gently stretch affected muscles
- Drink cool water or an electrolyte solution (low in sugar)
- For severe symptoms, treat as heat exhaustion (see below)
Moderate Heat Injury
Heat Syncope
Weakness, fatigue, and fainting are the chief symptoms of heat syncope. They are typically brought on by exercising hard in the heat. Too much salt and water are lost through perspiration and are not replaced.
Heat syncope often occurs during the first 5 days of adjusting to a new activity. It also can occur in people taking diuretic medicines or those with pre-existing heat illness. Young athletes returning to play after time off for injury are also at greater risk for heat syncope.
Without treatment, heat syncope can put you at risk for heat stroke.
Heat Exhaustion (Water Depletion)
Heat exhaustion is brought on by heavy sweating and results in extreme weight loss. As heat exhaustion sets in, perspiration decreases, and skin and body temperatures rise. Core body temperature typically rises to 104° F.
Additional signs of heat exhaustion include excessive thirst, weakness, headache, and sometimes loss of consciousness.
Heat Exhaustion (Salt Depletion)
Common signs of heat exhaustion due to salt depletion are nausea and vomiting, frequent muscle cramps, and dizziness. Core body temperature is typically up to 104° F.
You are at risk for this type of heat exhaustion when you do not sufficiently replace normal body salts and minerals. This can sometimes happen during prolonged exercise if water alone is used to replenish fluids. Body minerals, such as those found in sports drinks, must also be replaced.
Electrolyte fluid drinks are an effective way to prevent this type of heat exhaustion.
Treatment for Heat Syncope and Heat Exhaustion
- Move the person to a cool, shaded area
- Remove tight clothing
- Give fluids, if the athlete is conscious
- Apply active cooling measures, such as a fan or ice towels, if the athlete's core temperature is elevated
- Refer to a physician to assess the needs of fluid/electrolyte replacement and further medical attention, especially if the athlete is nauseated and/or vomiting
Severe Heat Injury
Heat Stroke
Heat stroke is the most severe form of heat injury. When suffering from heat stroke, your body cannot cool itself. This is an acute medical emergency.
Heat stroke is medically defined as core body temperature greater than 104° F. Organ system failure can result from this high of a body temperature.
Nausea, seizures, and confusion or disorientation often occur with heat stroke. Unconsciousness and coma are possible.
Heat stroke may occur with no preceding signs of heat injury. It can also occur as a progression from heat syncope and heat exhaustion. Again, this is a medical emergency.
Treatment of Heat Stroke
- Call 911 immediately for emergency services
- Monitor core body temperature and lower it as quickly as possible
- Decrease core body temperature through immersion in an ice bath
- Remove as much clothing as possible
- Apply ice packs to the armpits, groin, and neck
- Continue cooling efforts until an emergency crew arrives
Prevention
There are many ways to reduce your risk for heat injury.
General Guidelines
- Consult with your doctor before starting a new exercise activity if you have a health condition, like heart or lung disease, or take medication that could cause dehydration.
- Take time to adapt to a new activity or climate. Coaches should plan pre-season conditioning programs. These should be held during weather conditions similar to a typical practice.
- Increase the intensity and duration of your exercise program gradually. If you participate in sports that require protective equipment, avoid wearing it at the start of training.
Recommendations
- Allow frequent periods of rest and hydration during activity. Fluid replacement is essential to preventing heat injury.
- Make sure you are well hydrated before, during, and after exercise. Replace your fluids, whether you feel thirsty or not.
- A general recommendation is to drink 24 ounces of non-caffeinated fluid 2 hours before exercise. Drinking an additional 8 ounces of water or sports drink right before exercise is also helpful. While you are exercising, break for an 8 oz. cup of water every 20 minutes.
- Monitor the color of your urine. The darker your urine, the less hydrated you are and the greater your risk for heat injury. Drink enough fluids to keep your urine a very light color.
- Weigh yourself before and after activity to monitor water loss. Make sure you have replaced fluids before your next exercise session.
- Gradually increase activity in the heat over a period of 7 to 10 days to allow adequate acclimatization.
- Wear lightweight and light-colored clothing.
- Protect against sun exposure with sunscreen.
- Schedule outdoor exercise at the coolest time of day, either early morning or after sunset.
- Routinely monitor changing weather conditions. Pay close attention to temperature and humidity on playing surfaces (indoor/outdoor).
- Strongly consider postponing or cancelling your activity when there are extreme heat and humidity conditions.
Preventing Heat Injury Infographic
Last Reviewed
August 2021
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.