Treatment
Posterior Lumbar Interbody Fusion and Transforaminal Lumbar Interbody Fusion
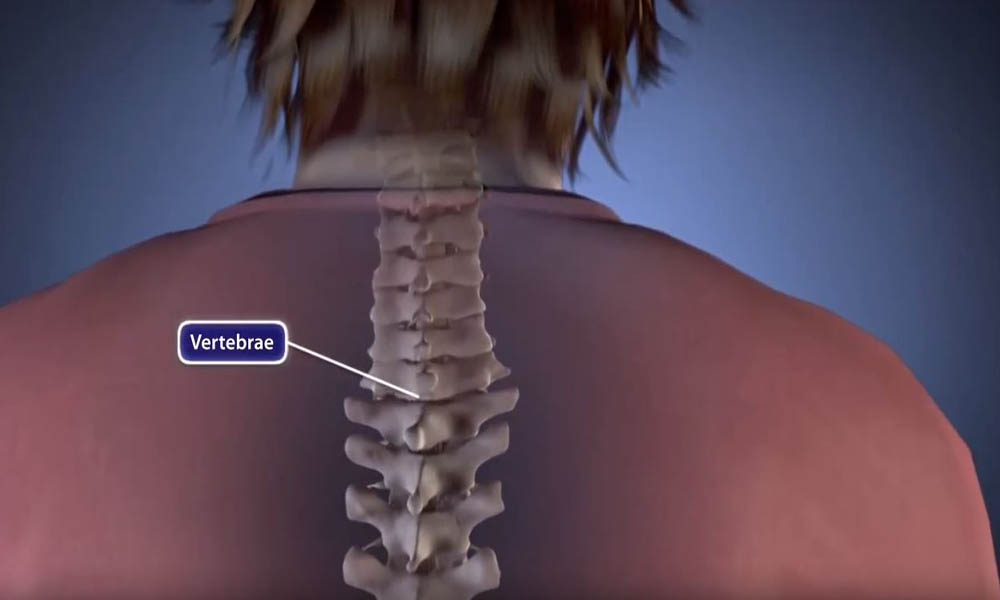
Spinal fusion is a surgical procedure used to correct problems with the small bones in the spine (vertebrae). It is essentially a welding process. The basic idea is to fuse together the painful vertebrae so that they heal into a single, solid bone.
Spinal fusion is a treatment option when motion is the source of the pain — the theory being that if the painful vertebrae do not move, they should not hurt.
This article focuses on two methods of fusing the lumbar (lower) spine:
- Posterior lumbar interbody fusion (PLIF)
- Transforaminal lumbar interbody fusion (TLIF)
Your doctor will talk with you about which method is appropriate in your situation. This article discusses only the surgical component of these two procedures.
For a complete overview of spinal fusion, including approaches, bone grafting, complications, and rehabilitation, please refer to Spinal Fusion.
Interbody Fusion
An interbody fusion is a type of spinal fusion that involves removing the intervertebral disk from the disk space.
When the disk space has been cleared out, your surgeon will implant a metal, plastic, or bone spacer between the two adjoining vertebrae. This spacer, also known as a cage:
- Promotes bone healing
- Helps make the fusion happen
- Increases the collapsed intervertebral disk space
After the cage is placed in the disk space, the surgeon may add stability to your spine by using metal screws, plates, and rods to hold the cage in place.
An interbody fusion can be performed using a variety of different approaches. Two common types are posterior lumbar interbody fusion and transforaminal lumbar interbody fusion.
Posterior Lumbar Interbody Fusion
In posterior lumbar interbody fusion (PLIF), your surgeon inserts the spacer or cage from the back of the spine. With this approach, your surgeon gains access to your spine by removing the bone (lamina) and then retracting (moving) the nerve roots to one side. Then the back of the intervertebral disk can be removed and a spacer inserted.
Transforaminal Lumbar Interbody Fusion
This technique is a variation of PLIF. In transforaminal lumbar interbody fusion (TLIF), your surgeon approaches the disk space slightly more from the side. The advantage of this approach is that it requires less movement of the nerve roots; thus, theoretically, it decreases the chance of nerve injury.
Advantages and Disadvantages of Posterior/Transforaminal Lumbar Interbody Fusion
Each surgical approach — whether from the front, back, or side — has advantages and disadvantages. The potential advantages of a posterior/transforaminal lumbar fusion include:
- Direct access to the bone putting pressure on the nerves
- When performing a revision surgery, allows the surgeon to remove previous hardware
- Improved alignment of the spinal bones
In addition, a transforaminal fusion may be performed with a less invasive technique, resulting in reduced muscle injury.
These results can also be achieved through fusions performed from the back or the front.
Typically, the complication rate for the posterior/transforaminal procedure is similar to that of traditional spinal surgery. Possible disadvantages include:
- Nerve damage, which can result in weakness in the leg
- Potential for the cage to move, putting pressure on the nerves
- Hematoma, or bleeding into the muscle, which can put pressure on the nerves and cause weakness
Talk to your surgeon about the approach that will best meet your health needs.
Recovery
Patients typically go home the same day or next day if only one level is fused. If more than one level is fused, most patients stay in the hospital overnight.
After going home, patients should watch for any weakness in the legs that makes their legs buckle and alert the surgeon right away if this symptom occurs.
Pain medication is usually needed for a few days to weeks. Your surgeon may also provide you with a brace to help the fusion heal.
Outcomes for posterior/transforaminal lumbar interbody fusion are equal to those of traditional surgeries. This procedure can be performed through a smaller incision in some cases, which may minimize muscle damage.
Future Directions
Recent advances include:
- The development of cages made of different materials, which can be used to improve the fusion rate.
- Expandable cages that can be inserted through smaller incisions and then expanded to fit your anatomy. With this approach, there may be less chance of muscle and nerve damage when the surgeon inserts the cage.
- The use of tubular retractors. With the assistance of tubular retractors, surgeons can perform transforaminal interbody fusion in a minimally invasive fashion, which enables smaller incisions and potentially reduces muscle damage.
Last Reviewed
February 2023
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.