Treatment
Rotator Cuff Tears: Surgical Treatment Options
The following article provides in-depth information about surgical treatment for rotator cuff injuries and is a continuation of the article "Rotator Cuff Tears." For a good introduction to the topic of rotator cuff injuries, please refer to Rotator Cuff Tears .
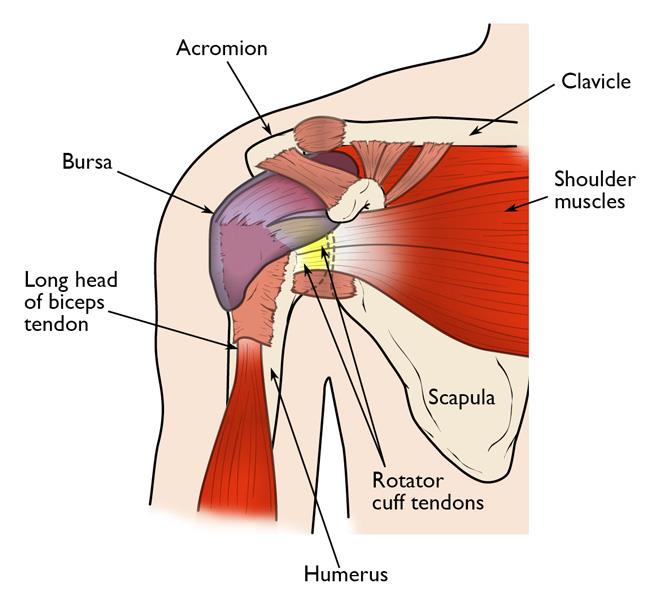
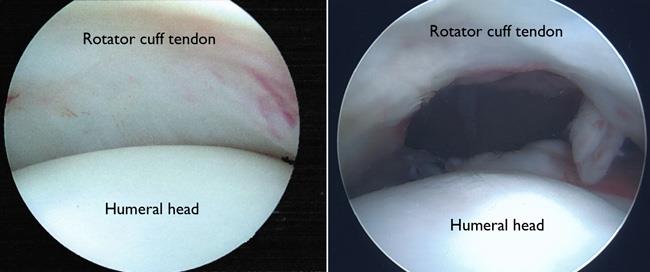
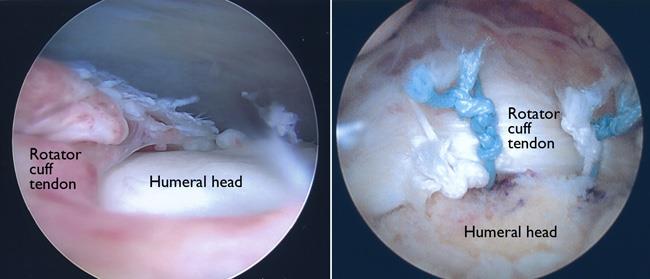
Surgery to repair a torn rotator cuff most often involves re-attaching the tendon to the head of the humerus (upper arm bone). A partial tear, however, may need only a trimming or smoothing procedure called a debridement. A complete tear is repaired by stitching the tendon back to its original site on the humerus.
When Rotator Cuff Surgery is Recommended
Your doctor may offer surgery as an option for a torn rotator cuff if your pain does not improve with nonsurgical methods. Continued pain is the main indication for surgery. If you are very active and use your arms for overhead work or sports, your doctor may also suggest surgery.
Other signs that surgery may be a good option for you include:
- Your symptoms have lasted 6 to 12 months
- You have a large tear (more than 3 cm) and the quality of the surrounding tendon tissue is good
- You have significant weakness and loss of function in your shoulder
- Your tear was caused by a recent, acute injury
Surgical Repair Options
There are a few options for repairing rotator cuff tears. Advances in surgical techniques for rotator cuff repair include less invasive procedures. While each of the methods available has its own advantages and disadvantages, all have the same goal: getting the tendon to heal back to bone.
The type of repair performed depends on several factors, including:
- Your surgeon's experience and familiarity with a particular procedure
- The size of your tear
- Your anatomy
- The quality of the tendon tissue and bone
Most surgical repairs can be done on an outpatient basis and do not require you to stay overnight in the hospital. Your orthopaedic surgeon will discuss with you the best procedure to meet your individual health needs.
You may have other shoulder problems in addition to a rotator cuff tear, such as:
- Biceps tendon tears
- Osteoarthritis
- Bone spurs
- Other soft tissue tears
During the operation, your surgeon may be able to take care of these problems, as well.
The three techniques most commonly used for rotator cuff repair are:
- Traditional open repair
- Arthroscopic repair
- Mini-open repair
In the end, patients rate all three repair methods the same for pain relief, strength improvement, and overall satisfaction.
Open Repair
A traditional open surgical incision (several centimeters long) is often required if the tear is large or complex. The surgeon makes the incision over the shoulder and detaches or splits part one of the shoulder muscles (deltoid) to better see and gain access to the torn tendon.
During an open repair, the surgeon typically removes bone spurs from the underside of the acromion (this procedure is called an acromioplasty). An open repair may be a good option if:
- The tear is large or complex
- Additional reconstruction, such as a tendon transfer, is needed
Open repair was the first technique used for torn rotator cuffs. Over the years, new technology and improved surgeon experience has led to less invasive procedures.
All-Arthroscopic Repair
During arthroscopy, your surgeon inserts a small camera, called an arthroscope, into your shoulder joint. The camera displays a live video feed on a monitor, and your surgeon uses these images to guide miniature surgical instruments.
Because the arthroscope and surgical instruments are small and thin, your surgeon can use very small incisions (portals), rather than the larger incision needed for standard, open surgery.
All-arthroscopic repair is usually an outpatient procedure and is the least invasive method to repair a torn rotator cuff.
Mini-Open Repair
The mini-open repair is performed through a smaller open incision than is used in traditional open repair.
This technique typically uses arthroscopy to assess and treat damage to other structures within the joint. Bone spurs, for example, are often removed arthroscopically. This avoids the need to detach the deltoid muscle.
Once the arthroscopic portion of the procedure is completed, the surgeon repairs the rotator cuff through the mini-open incision. During the tendon repair, the surgeon views the shoulder structures directly, rather than through the video monitor.
Recovery
Pain Management
After surgery, you will feel pain. This is a natural part of the healing process. Your doctor and nurses will work to reduce your pain.
Medications are often prescribed for short-term pain relief after surgery. Many types of medicines are available to help manage pain, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics. Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids.
Be aware that although opioids help relieve pain after surgery, they are narcotics and can be addictive. Opioid dependency and overdose have become critical public health issues. It is important to use opioids only as directed by your doctor and to stop taking them as soon as your pain begins to improve. Talk to your doctor if your pain has not begun to improve within a few weeks after your surgery.
Rehabilitation
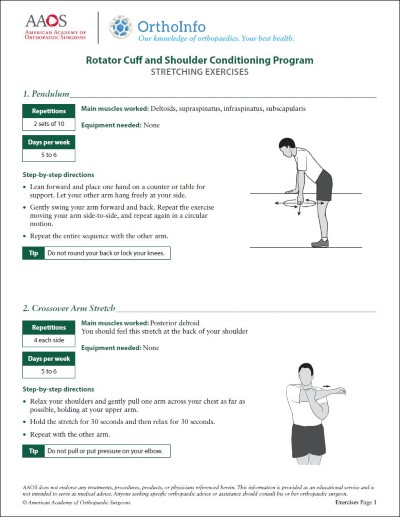
Rehabilitation plays a vital role in getting you back to your daily activities. A physical therapy program will help you regain shoulder strength and motion.
Immobilization. After surgery, therapy progresses in stages. At first, the repair needs to be protected while the tendon heals. To keep your arm from moving, you will most likely use a sling and avoid using your arm for the first 4 to 6 weeks. How long you require a sling depends on the severity of your injury.
Passive exercise. Even though your tear has been repaired, the muscles around your arm remain weak. Once your surgeon decides it is safe for you to move your arm and shoulder, a therapist will help you with passive exercises to improve range of motion in your shoulder. With passive exercise, your therapist supports your arm and moves it in different positions. In most cases, passive exercise is begun within the first 4 to 6 weeks after surgery.
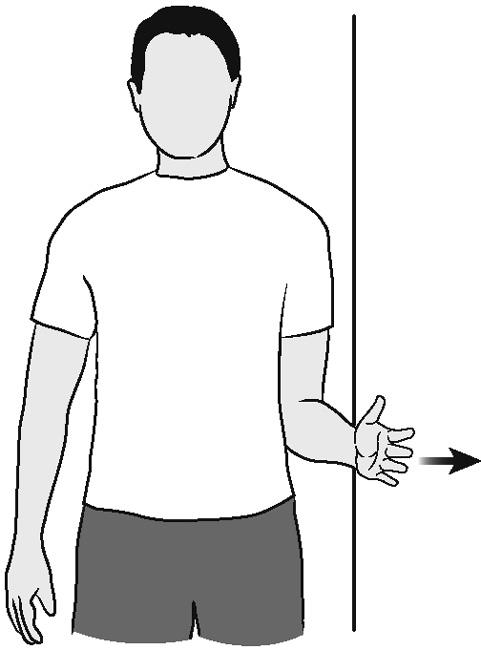
Active exercise. After 4 to 6 weeks, you will progress to doing active exercises without the help of your therapist. Moving your muscles on your own will gradually increase your strength and improve your arm control. At 8 to 12 weeks, your therapist will start you on a strengthening exercise program.
Expect a complete recovery to take several months. Most patients have a functional range of motion and adequate strength by 4 to 6 months after surgery. Although it is a slow process, your commitment to rehabilitation is key to a successful outcome.
Outcome
The majority of patients report improved shoulder strength and less pain after surgery for a torn rotator cuff.
Each surgical repair technique (open, mini-open, and arthroscopic) has similar results in terms of pain relief, improvement in strength and function, and patient satisfaction. Surgeon expertise is more important in achieving satisfactory results than the choice of technique.
Factors that can decrease the likelihood of a satisfactory result include:
- Poor tendon/tissue quality
- Large or massive tears
- Poor patient compliance with/participation in restrictions and rehabilitation after surgery
- Patient age (older than 65 years)
- Smoking and use of other nicotine products
- Workers' compensation claims
Complications
After rotator cuff surgery, a small percentage of patients experience complications. In addition to the risks of surgery in general, such as blood loss or problems related to anesthesia, complications of rotator cuff surgery may include:
- Nerve injury. This typically involves the nerve that activates your shoulder muscle (deltoid).
- Infection. Patients are given antibiotics during the procedure to lessen the risk for infection. If an infection develops, additional surgery and/or prolonged antibiotic treatment may be needed.
- Deltoid detachment. During an open repair, this shoulder muscle may be partially detached to provide better access to the rotator cuff. It is stitched back into place at the end of the procedure. It is very important to protect this area after surgery and during rehabilitation to allow it to heal.
- Stiffness. Early rehabilitation lessens the likelihood of permanent stiffness or loss of motion. Most of the time, stiffness will improve with more aggressive therapy and exercise.
- Tendon re-tear. There is a chance for re-tear following all types of repairs. The larger the tear, the higher the risk of re-tear. Patients who re-tear their tendons usually do not have greater pain or decreased shoulder function. Repeat surgery is needed only if there is severe pain or loss of function.
To assist doctors in the management of rotator cuff tears, the American Academy of Orthopaedic Surgeons has conducted research to provide some useful guidelines. These are recommendations only and may not apply to every case. For more information: Plain Language Summary - Clinical Practice Guideline - Management of Rotator Cuff Injuries - AAOS
Last Reviewed
June 2022
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.