Treatment
Finger Joint Replacement
Finger joint replacement, also known as finger joint arthroplasty, is a surgical procedure used to relieve pain and restore motion in finger joints that have been damaged by arthritis , trauma (like fractures), gout, or other degenerative conditions.
The procedure involves removing the worn-out joint surfaces and replacing them with artificial implants designed to mimic the natural movement of the finger.
Finger joint replacement is typically performed on patients who have failed to improve with non-operative treatments such as anti-inflammatory medication, therapy, activity modification, or injections. It can be an effective option for patients seeking to regain hand function and quality of life.
Anatomy
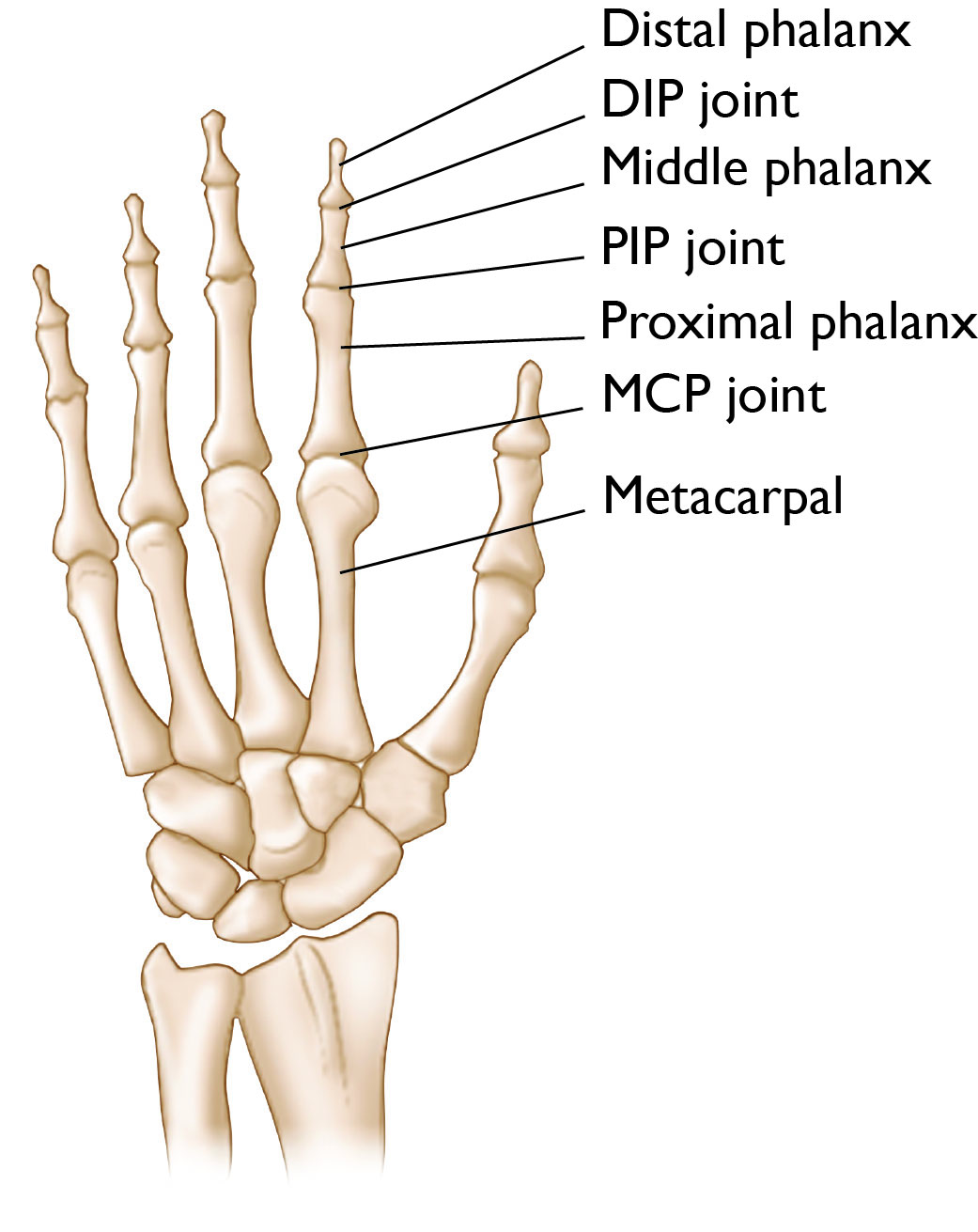
Each finger (not the thumb) has three bones connected by joints.
- The distal phalanx is the last bone of the finger at the very tip. It connects to the middle phalanx, the middle bone of the finger, via the DIP joint.
- The middle phalanx connects to the proximal phalanx, the bone in the finger closest to the hand, via the PIP joint.
- The proximal phalanx connects the finger bone to the hand bone (metacarpal) via the MCP joint.
Most implants are designed to replace the PIP joints or the MCP joints, where motion is most important for finger function. Patients with severe DIP joint issues typically are treated with fusion (also called arthrodesis) instead of replacement.
Types of Implants
Finger joint implants vary in material, design, and the method by which they connect to the bone. Common types include:
- Silicone implants – flexible spacers that allow some motion and have some stability built into the implant itself. These types of implants have been around the longest in clinical use.
- Pyrocarbon implants – durable and wear-resistant, offering more natural joint mechanics.
- Metal and plastic (polyethylene) implants – similar to knee replacements, these function very much like pyrocarbon implants.
Each implant type has advantages and limitations. Your surgeon will select the best option based on your anatomy, activity level, and underlying condition.
Conditions Treated
Finger joint replacement is typically performed for patients with degenerative, or worn out, finger PIP and MCP joints. There are a variety of conditions that can cause this, including but not limited to:
- Osteoarthritis (wear-and-tear arthritis)
- Autoimmune arthritis
- Posttraumatic arthritis (arthritis caused by injury)
- Gout
- Post-infectious arthritis
Finger joint replacement may be performed on any of the fingers; however, it is rarely, if ever, performed at the DIP joints of the fingers.
Patients may be candidates for finger joint replacement when:
- Nonsurgical treatments (anti-inflammatory medications, injections, therapy, etc.) have failed
- The joint becomes painful, interfering with daily activities
- The patient wants to maintain motion of the joint, something fusion surgery does not do
- The patient is healthy enough to undergo surgery and the therapy that follows
Fusion (also called arthrodesis) is an alternative to joint replacement where the affected joint is removed and the bones at the joint are connected with pins, wires, plates/screws, etc. This robs the joint of motion but relieves pain and has excellent longevity. Your doctor will likely discuss this option with you. In some cases, it may be a better choice for you than joint replacement.
Learn more: Finger (IP Joint) Fusion
Doctor Examination
Physical Examination
Your doctor will ask how and when your symptoms started and will ask you to describe your symptoms. They will then carefully examine your finger and hand.
Your doctor will move your finger in different ways to test the stability and motion of the joint(s). The result of this examination may change your doctor's recommendation on which surgery or implant may be best for you, or if any surgery at all is an option.
Imaging Tests
X-rays. X-rays provide images of dense structures, such as bone. Your doctor may order X-rays of your finger and hand to evaluate your condition and plan the surgery.
Other imaging tests. If more information is needed, your doctor may order a computed tomography (CT) scan or a magnetic resonance imaging (MRI) scan. These tests can help your doctor learn more about the severity of your condition and make decisions about your treatment.
Surgery
Finger joint replacement is typically an outpatient procedure, meaning you will go home the same day as your surgery.
The surgery itself involves the following steps:
- Safely entering the joint
- Removing the damaged joint surfaces
- Selecting, sizing, and inserting the prosthetic implant
- Repairing any critical tissues (e.g. ligaments or tendons)
- Closing the skin
- Applying a dressing or splint
Post-Surgical Treatment
Within a few days to a few weeks after surgery, your doctor will likely send you to a therapist to work on moving the new joint.
Hand therapy is essential after finger joint replacement and focuses on range of motion exercises, tendon gliding exercises, and eventually strengthening within the safe confines of your surgery. You will need to find a balance between moving the joint to avoid stiffness and protecting the joint to avoid damage. A removable splint may be created for you to protect the joint when not performing therapy exercises.
An example post-operative course would be:
- Weeks 1 and 2: Hand is immobilized in a splint or cast. Elevation and pain control are critical. Gentle range-of-motion exercises may begin. Sutures are removed (10 to 14 days)
- Weeks 3 to 5: Swelling begins to subside. Hand therapy advances with guided motion and stretching.
- Weeks 6 to 8: Patients may resume light activities and some work duties. Splints may be discontinued.
- Weeks 8 to 12: Most patients regain functional use of the hand. Return to household activities and hobbies is often permitted.
- 3 to 6 Months: Continued improvement in strength and motion. Full recovery may take up to 1 year.
Your doctor will typically see you in their office at regular intervals for several weeks or months to make sure you are recovering appropriately.
Outcomes
In the right patient, outcomes for finger joint replacement can be good.
- Finger joint replacement can relieve pain, improve joint alignment, restore functional motion, and enhance finger appearance and quality of life.
- It is important to know that finger joint replacement will probably not improve finger motion. Most patients keep the motion they had prior to the surgery. The benefit is in the relief of pain during that motion.
- Success rates are generally high, though long-term durability depends on implant type, patient activity, and how well you stick with your rehabilitation. You doctor may advise you to avoid heavy gripping, contact sports, or high-impact activities to prolong implant life.
Risks of surgery may include, but are not limited, to:
- Infection
- Implant loosening or failure
- Joint stiffness or instability
- Nerve injury or tendon injury
- The need for revision surgery
Because of these risks, it is important to select the right surgery for each patient, and to select the right implant for patients who do have joint replacement.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.