Staying Healthy
Hip Fracture Prevention
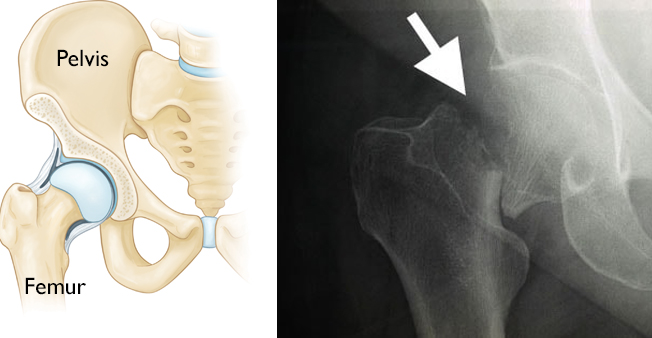
Hip fractures are breaks in the femur (thighbone) at or just below the hip joint. They are serious injuries that most often occur in people age 65 and older. Elderly people, especially women are especially vulnerable to hip fractures because of osteoporosis.
Hip fractures can limit mobility and independence. Almost all hip fractures require surgery, hospitalization, and extended rehabilitation.
Most people who previously lived independently before hip fracture require assistance afterward. This can range from help from family members and home health professionals, to admittance to a nursing home or another long-term health facility.
Cause
Most hip fractures are caused by factors that weaken bone, combined with the impact from a fall.
Bone Strength
Bone strength decreases as we age. Bones can become very weak and fragile — a condition called osteoporosis. Osteoporosis often develops in women after menopause, and in older men. This bone-thinning disorder puts people at greater risk for broken bones, particularly fractures of the hip, wrist, shoulder, and spine.
Risk Factors
Many of the factors that make you more vulnerable to a hip fracture are also those that cause bone loss.
- Age. The risk of hip fractures increases as we age. Almost 80% of the people hospitalized for hip fractures are age 65 and older.
- Sex. Three-quarters (75%) of all hip fractures occur in women.
- Heredity. A family history of osteoporosis or broken bones in later life raises your risk of a hip fracture. People with small, thin builds are also at risk.
- Nutrition. Low body weight and poor nutrition, including a diet low in calcium and Vitamin D, can make you more prone to bone loss and hip fracture.
- Lifestyle. Smoking, alcohol use, and lack of exercise can weaken bones.
- Medical issues. Some medical conditions may weaken bones or contribute to osteoporosis and/or risk of falling. For example, kidney disease, celiac disease or other conditions may lead to osteoporosis. Learn more: Impact of Chronic Illness on Bone Health
In addition to factors that affect bone strength, things that raise your risk of falling can increase the possibility of hip fracture.
- Physical and mental impairments. Physical frailty, arthritis, unsteady balance, poor eyesight, neuropathy, neurological conditions (such as Parkinson's disease), or dementia (such as Alzheimer's disease) can all increase the chance of falling.
- Medications
- Many medicines can affect balance and strength.
- Side effects of some medications can include drowsiness and dizziness.
- Some medications can have a harmful effect on bone health — for example, by making it harder for the body to absorb calcium or by causing the body to break down Vitamin D too quickly.
Tips for Preventing Hip Fractures
Home Safety
Most hip fractures occur as a result of a fall, and most falls occur in the home. Many falls can be prevented by making simple home safety improvements, such as:
- Removing clutter from floors and hallways
- Removing or taping down loose rugs
- Providing enough lighting
- Installing grab bars in bathrooms (especially near the toilet and in the shower)
- Installing handrails along stairways
For more comprehensive information on preventing falls: Guidelines for Preventing Falls
Exercise
Moderate exercise can slow bone loss and maintain muscle strength. It can also improve balance and coordination. Good exercise options include walking, climbing stairs, jogging, hiking, bicycling, swimming, dancing, and weight training.
Tai chi and balance training with an emphasis on core conditioning have been shown to decrease falls and reduce the risk of hip fracture. Tai chi is a program of exercises, breathing, and movements based on ancient Chinese practices. These classes can also increase self-confidence and improve body balance.
Be sure to talk to your doctor if you are just beginning an exercise program.
Understand Your Health and Medications
Schedule an eye examination, as well as a physical that includes an evaluation for cardiac issues, diabetes, and other health conditions that you may need to manage.
Also, talk to your doctor about the side effects of any medications and over-the-counter drugs you take. It is helpful to keep an up-to-date list of all medications you take so that you can provide it to any other doctors with whom you consult.
Learn more about the potential effects of certain chronic health conditions and treatments for health conditions on your bone health: Impact of Chronic Illness on Bone Health
Maintain Your Bone Health As You Age
As we age, our bones are affected by genetics, nutrition, exercise, and hormonal loss. We cannot change our genes, but we can control our nutrition and activity level and, if necessary, take osteoporosis medications.
There are things you can do to maintain and even improve your bone strength.
- Understand your personal fracture risk. This is based on any fracture risk factors you have and your bone density. Ask your doctor if you need a bone density test (DEXA scan).
- Understand your individual risk of bone loss. Genetics plays a role in bone health, and some people have genetically determined high rates of bone turnover after menopause or with aging. Talk to your doctor about bone metabolism testing. Bone metabolism testing can provide additional information about your fracture risk.
- Make healthy lifestyle choices. Maintain a healthy weight and eat a diet rich in calcium and Vitamin D. Do not smoke, and limit your alcohol intake. Begin an exercise program and stick with it.
- Consider bone-boosting medications. There are many drug options that slow bone loss and increase bone strength. Talk to your doctor about these methods for protecting your bones, and learn more: Osteoporosis Prevention and Treatment
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.