Diseases & Conditions
Ulnar Tunnel Syndrome of the Wrist
The ulnar nerve is one of the three main nerves that provide feeling and function to the hand. This nerve arises from the spinal cord and travels from your neck down your arm and into your hand. The nerve can be constricted in several places along the way, most commonly the wrist and elbow.
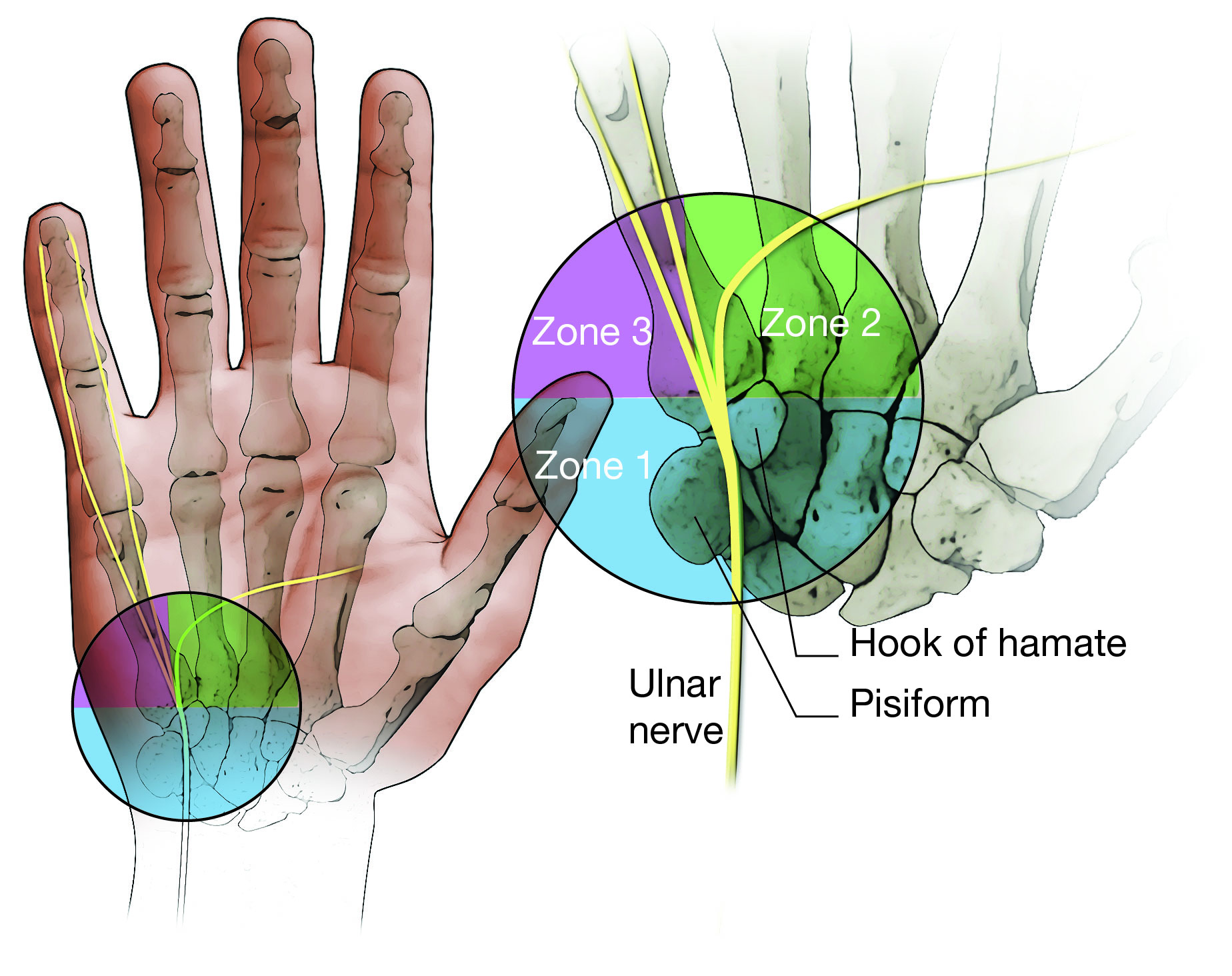
Ulnar tunnel syndrome occurs when the ulnar nerve is compressed at the wrist. This reduces blood flow to the nerve and can harm its function.
When compressed at the wrist, the malfunction of the nerve can cause numbness and tingling in the little finger (pinky) and the outside of the ring finger. Additionally, you may experience weakness of hand pinch and grip.
Learn more about Ulnar Nerve Entrapment at the Elbow (Cubital Tunnel Syndrome)
Cause
The most common cause of ulnar tunnel syndrome is a soft tissue tumor that pushes against the nerve. The tumor is typically a benign (noncancerous) cyst called a ganglion which originates from the wrist joint. Ganglion cysts are filled with a thick gel and can fluctuate in size.
Some people may be more susceptible to ulnar tunnel syndrome due to their particular anatomy. In these cases, the ulnar nerve may be compressed by a narrow tunnel (called Guyon's canal) as the nerve heads from the wrist into the hand.
Ulnar tunnel syndrome can also be caused by repetitive trauma or chronic pressure applied to the area of the hand where the ulnar nerve enters from the wrist. Specifically, this area is on the palm close to where the wrist meets the hand on the little finger side.
- A common example of repetitive trauma is the use of a jackhammer or other power tools.
- A common example of chronic pressure is cycling long distances with the body weight resting through the palm on a handlebar.
People with repetitive and/or chronic trauma to the palm can also develop issues with the blood flow to their hand, resulting in a condition called hypothenar hammer syndrome. In these cases, poor blood flow to the fingers (e.g., blue or white fingers) may accompany the numbness and tingling.
Symptoms
Symptoms of ulnar tunnel syndrome typically develop gradually.
- People commonly describe numbness and tingling in the little and ring fingers. They may also experience weakness in the hand resulting in poor grip, weak pinch, and difficulty separating and/or closing the fingers. The degree of numbness and weakness depends on the location of the pressure point and how long the condition has gone untreated.
- As the disease progresses, it may become more difficult to open jars, hold objects, or coordinate the fingers during certain tasks, such as typing or playing a musical instrument.
Doctor Examination
Physical Examination
Your doctor will examine your hand looking for common signs of ulnar tunnel syndrome.
- They will test the sensation in your fingers, focusing on the little finger and ring finger. They may ask you to try to tell the difference when they touch your fingertips with two small points vs. one small point. This ability can be diminished in patients with ulnar tunnel syndrome.
- They will look for indications that the muscles in your hand are becoming weak, such as reduced bulk (muscle atrophy) and poor strength.
- Sometimes muscle weakness can be seen when patients can't pull their small finger in to touch their ring finger (Wartenberg's sign).
- Weakness can also be seen when patients are unable to effectively pinch a piece of paper between the thumb and index finger without flexing the last joint on each digit (Froment's sign).
- They may apply pressure over the ulnar nerve at your wrist to see if this makes your numbness and tingling worse.
- They may tap their finger over the ulnar nerve at the wrist to determine whether this causes a tingling sensation (Tinel sign), which is a sign of nerve compression.
- Because the ulnar nerve also travels through a narrow tunnel at the elbow, your doctor may examine the elbow, as well. Pressure on the ulnar nerve at the elbow can also cause symptoms in the hand.
Tests
- A nerve conduction study/electromyography (NCS/EMG) may be performed to determine whether the nerve is working properly.
- A computed tomography (CT) scan, magnetic resonance image (MRI) scan, or ultrasound (US) may be used to identify whether something is putting pressure on the nerve (e.g., a cyst).
- X-rays may be used to identify whether a fragment of a fractured bone is pressing on the nerve.
Nonsurgical Treatment
Nonsurgical treatment depends on what is causing pressure on the nerve.
For example:
- If the pressure is caused by the way the wrist is positioned when typing, a change in wrist position or the addition of some padding may be recommended.
- In the case of a jackhammer operator, the person must eliminate the repetitive trauma by altering their technique, using protective padding, or changing jobs.
- A cyclist may relieve chronic pressure by frequently changing hand position on the handlebars and/or by adding protective padding between wrist and handlebar.
In many cases of ulnar tunnel syndrome, nonsteroidal anti-inflammatory drugs (NSAIDs), such as naproxen or ibuprofen, may alleviate symptoms. Short-term use of a wrist splint may also be helpful.
Surgical Treatment
Many cases of ulnar tunnel syndrome are caused by a growth at the wrist or a narrow ulnar tunnel as the nerve runs from the wrist into the hand. In these cases, surgery is necessary to remove the growth or open up the tunnel.
An experienced hand surgeon can remove cysts, scar tissue, and other causes of compression and open up the ulnar tunnel on an outpatient basis. This can restore normal blood flow to the nerve and allow for recovery of nerve function.
Complications
Complications of surgery are rare but may include infection, wound issues, or damage to nearby structures such as nerves, vessels, and tendons. You should discuss the risks and benefits of the surgery with your doctor before proceeding.
Surgical Outcome
Once the pressure point is removed, normal sensation may return and the tingling may decrease. It can, however, take several months to a year for the nerve to recover and heal completely.
Recovery may be incomplete in older patients with longer-term compression. Some muscle wasting/weakness may not be reversible. Even in these cases, addressing the issue is important to prevent worsening of the condition. Your surgeon may prescribe postoperative rehabilitation and/or home exercises to help with recovery.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.