Diseases & Conditions
Thumb Fractures
A broken thumb can be a serious problem. Loss of thumb function due to a fracture can affect your ability to grasp items, and certain types of thumb fractures can increase the risk of arthritis later in life.
Anatomy
Several bones contribute to thumb function.
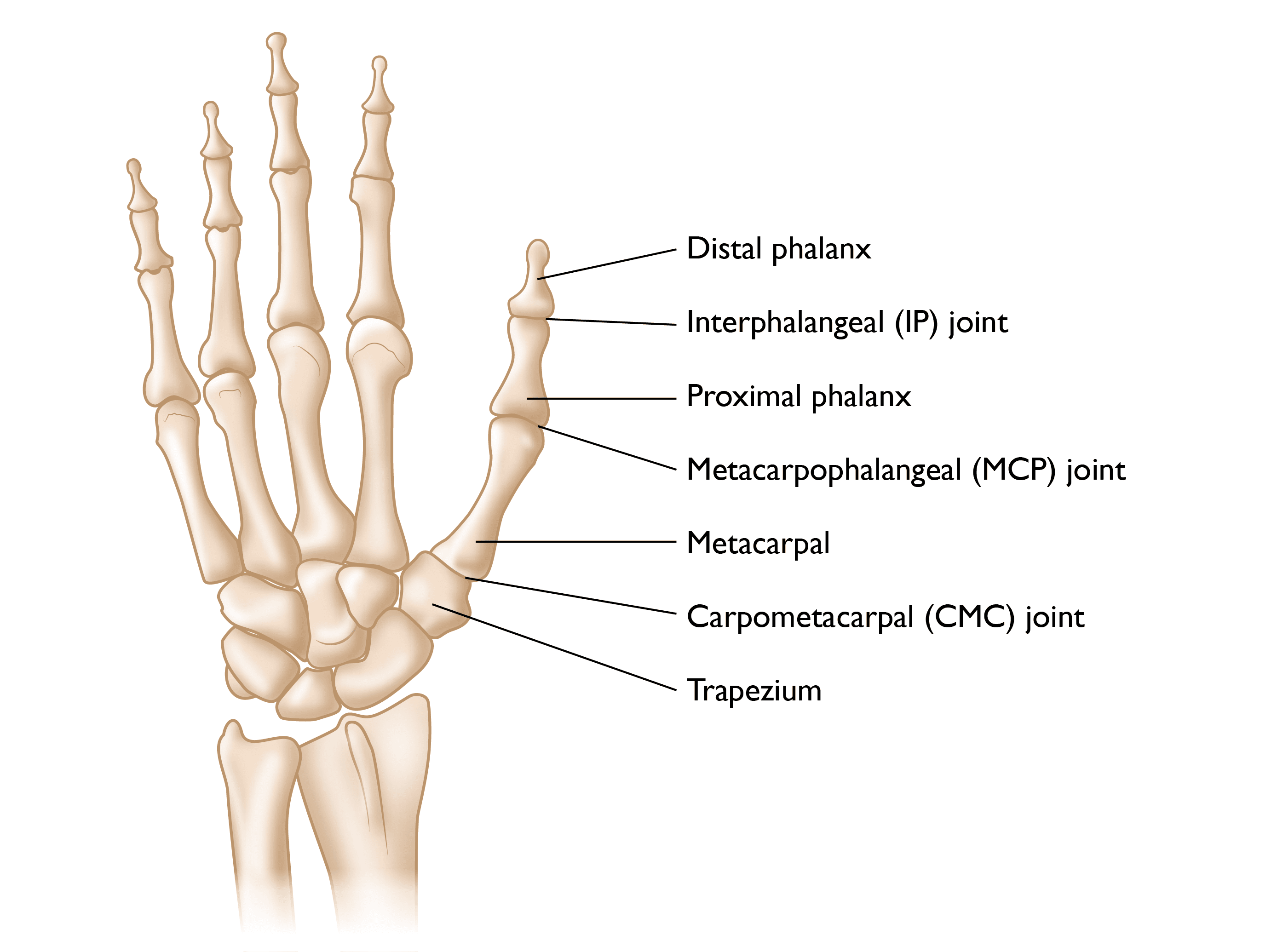
The bone under the nail that makes up the tip of the thumb is called the distal phalanx. The next bone is called the proximal phalanx. The distal phalanx and proximal phalanx connect via the interphalangeal (IP) joint, which allows you to bend the tip of your thumb.
The thumb connects to the hand through the next joint, known as the metacarpophalangeal (MCP) joint. This joint sits between the proximal phalanx and a bone in the hand called the first metacarpal.
The first metacarpal is connected to the wrist by the carpometacarpal (CMC) joint, which sits between the metacarpal and a carpal bone called the trapezium.
There is an area of webbing between the thumb and first finger that allows you to spread your thumb out to grasp an object.
The bones of the thumb have several important ligaments at each joint that both allow for motion of the joint and keep the joint stable so it does not dislocate:
- The flexor pollicis longus (FPL), which runs along the palm side of the thumb and allows you to bend your thumb
- The extensor pollicis longus (EPL), located on the back side of the thumb, which allows you to straighten your thumb.
Several other tendons/muscles allow the thumb to move in virtually all directions.
The thumb also has several nerves that give you feeling and blood vessels that provide the thumb with blood flow.
Description
All of the bones in the thumb are susceptible to fracture. Typically, the most concerning and problematic broken bones involve the joints. Fractures that involve the joints are typically more difficult to treat and are at increased risk for an unfavorable outcome.
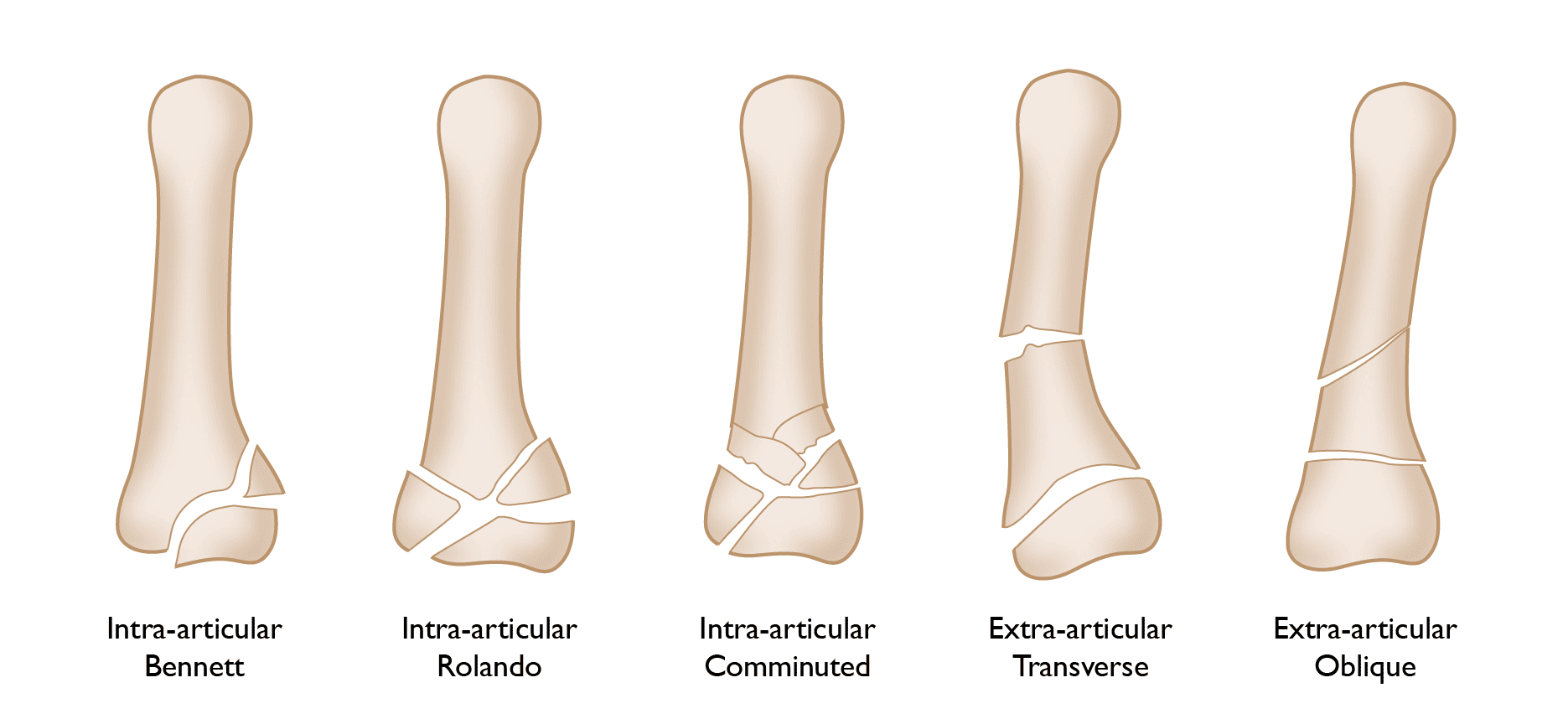
The most common of these in the thumb are fractures involving the base of the first metacarpal, affecting the CMC joint where the thumb connects to the wrist:
- A Bennett fracture is a fracture at the base of the thumb metacarpal involving the CMC joint, resulting in a clean break with a sizeable piece of bone broken off.
- A Rolando fracture is similar to a Bennett fracture, except that instead of a clean break, the bone is shattered into several pieces.
Fractures of the thumb metacarpal can also occur in the long portion of the bone, which is called the metacarpal shaft. These are often easier to treat than fractures involving the joint.
The other bones of the thumb — the distal phalanx and proximal phalanx — are also susceptible to fractures. Like the metacarpal, the distal and proximal phalanges can fracture near/into a joint or in the shaft of the bone.
Sometimes, thumb fractures can result in joint instability when they involve the important ligaments that keep the joints aligned. These are often avulsion injuries, which occur during an extreme force to the joint that causes the ligament to rip away from its attachment, taking a piece of bone with it. These injuries function as ligament injuries and are often treated as such.
Cause
- Thumb fractures are usually caused by direct trauma, such as from a fall or a blow to the hand.
- A thumb fracture may also happen in sports when a ball catches and pulls the thumb back.
- Some fractures may be caused indirectly, from twisting or even from strong muscle contractions, as might occur in wrestling, hockey, football, and skiing.
People with a history of bone disease or calcium deficiency are especially at risk for thumb fractures.
The risk of a thumb fracture can be lessened by using protective taping, padding, or other equipment. Developing strength in the hands through exercise and getting proper nutrition can also provide some protection.
Symptoms
Symptoms of a fractured thumb include:
- Severe pain at the fracture site
- Swelling
- Limited or no ability to move the thumb
- Extreme tenderness when the thumb is touched
- A misshapen or deformed look to the thumb
- Numbness or coldness in the thumb
- Instability of a joint in the thumb
Doctor Examination
Consult a doctor as soon as possible if you suffer a thumb injury and suspect a fracture has occurred. A delay in treatment may make it more difficult to align the bones properly and may lead to a poor outcome. A padded splint can be used to prevent the bone from moving farther out of alignment. This is encouraged before treatment is finalized.
The physician will examine the injury, take a medical history, and order X-rays of the injury. They will also:
- Test the tendons and nerves of the thumb to make sure there are no other associated injuries
- Look for injuries to the other digits and the rest of the hand
- Stress the ligaments of the thumb to make sure they are strong and have no evidence of injury
Treatment
Nonsurgical Treatment
If the bone fragments of the fracture have not moved (displaced) very much, or if the break is located in the middle (shaft) of the bone, your surgeon may be able to treat the thumb fracture without surgery using a specially designed cast (spica cast) to hold the bone fragments in place. You will likely need to wear the cast for at least 4 to 6 weeks. During that time, you will need regular X-rays to ensure that the bone has not slipped out of alignment.
Surgical Treatment
You may need surgery to treat the thumb fracture, depending on the location of the break, the alignment of the broken bone, and the amount of movement between the fragments. Your surgeon may use one of several operative fixation techniques to realign the bone fragments. These broken bone fragments must be held in place while the bone heals.
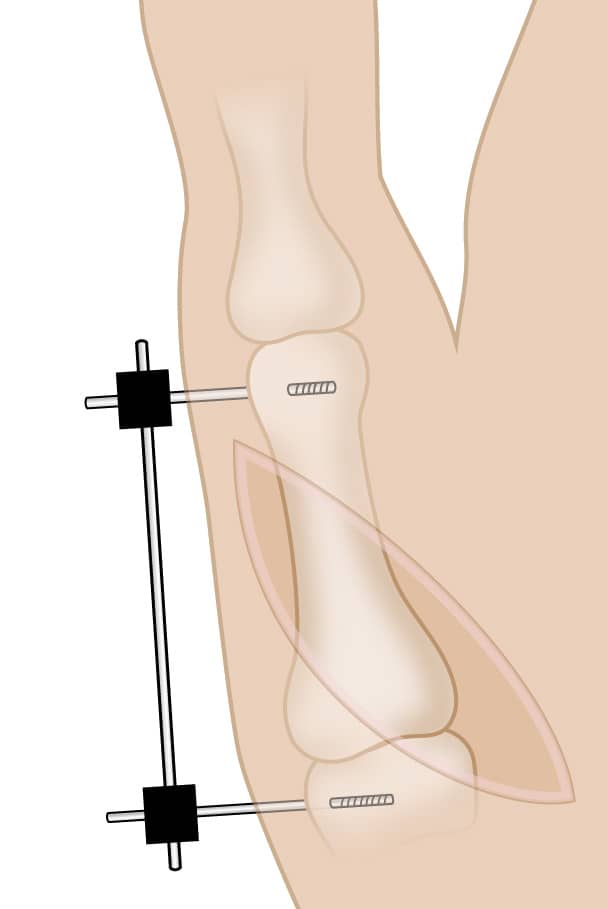
Bone fixation techniques include devices that hold the bone fragments in place either inside the body (internal fixation) or outside the body (external fixation).
- Internal fixation techniques include the use of wires, pins, plates, and screws.
- External fixation techniques include the use of pins in bone that are held in place through their attachment to an external fixation device.
There are pros and cons to all treatment options. Your surgeon will discuss with you which option is best for your fracture.
You will likely wear a cast or splint for 2 to 6 weeks after surgery. When the cast is removed, your doctor may recommend hand therapy to restore movement to your hand. It can take 3 months or more to regain full use of the hand, depending on the severity of the injury.
Outcome
If the bones remain in a stable position with good alignment, thumb fractures generally heal well. Surgery does have some potential complications, which could include infection, wound issues, or failure of the surgery to hold alignment. These complications, while rare, can be problematic.
If the thumb fracture involves a joint, there is an increased tendency to develop arthritis in the long term even if the fracture is treated perfectly. Arthritis can result in limited joint motion and pain in the joint. This typically occurs several years after the injury.
Once the fracture has healed, it is very important to follow all therapy instructions to improve motion in the thumb. Therapy is designed to ensure that you won't overdo it and possibly cause the thumb to come out of alignment, or do too little, which can lead to stiffness of the thumb.
Overall, many thumb fractures have good outcomes after appropriate treatment.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.