Diseases & Conditions
Talus Fractures
A talus fracture is a break in one of the bones that forms the ankle. This type of fracture often occurs during a high-energy event, such as a motor vehicle collision or a fall from a substantial height.
Because the talus is important for ankle movement, a fracture often results in substantial loss of motion and function. A talus fracture that does not heal properly can lead to complications, including a limp, arthritis, and chronic pain. For this reason, most talus fractures require surgery.
Anatomy
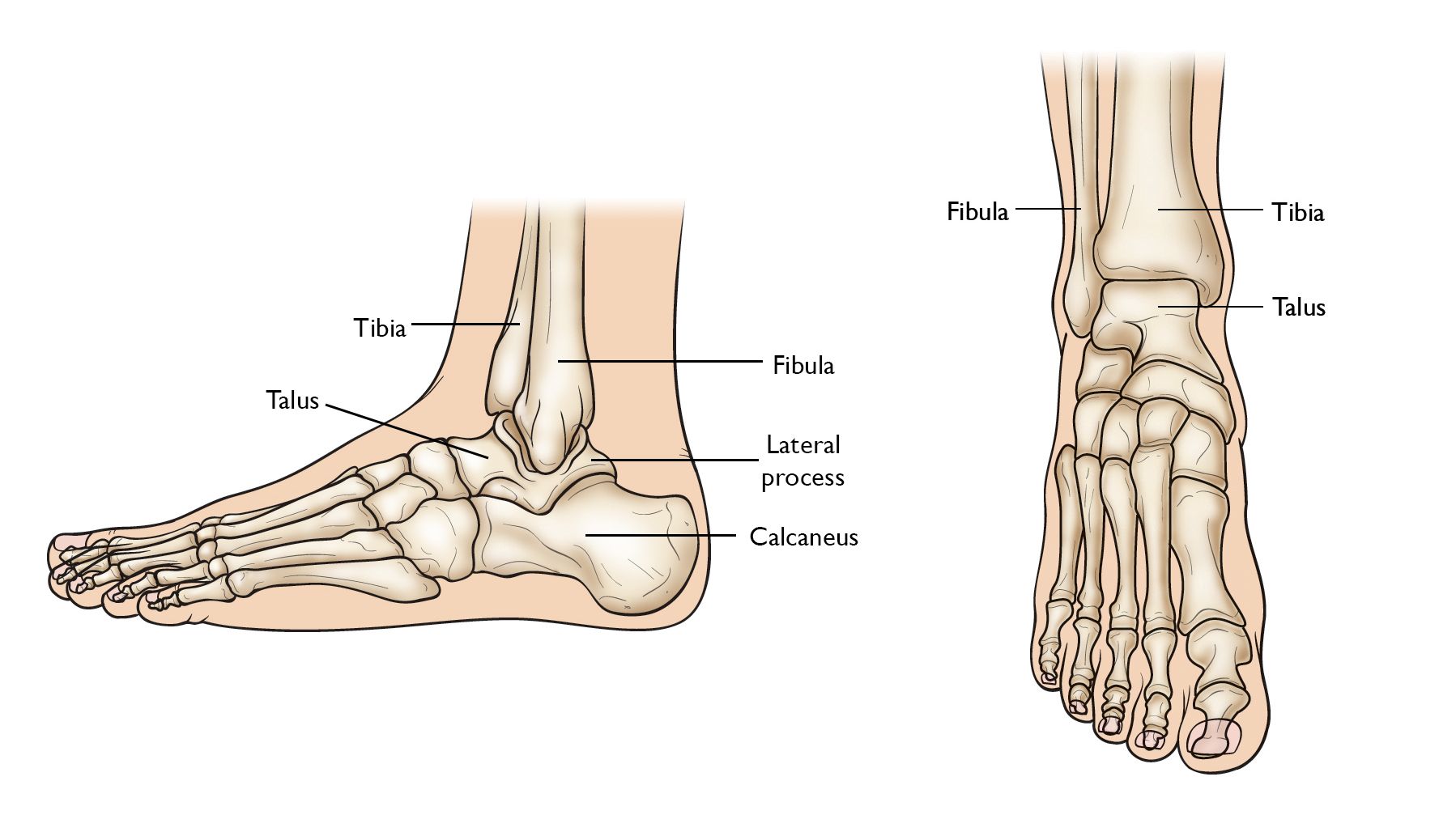
The talus is the bone that makes up the lower part of the ankle joint (the bones of the lower leg, the tibia and fibula, make up the upper part of the ankle joint). The ankle joint allows your foot to move up and down.
The talus also sits above the heel bone (calcaneus). Together, the talus and calcaneus form the subtalar joint. This joint allows your foot to move inward and outward, which is important for walking on uneven ground.
The talus is the main connector between the foot and leg, helping to transfer weight and pressure forces across the ankle joint. It is largely covered by articular cartilage, the white, smooth material that covers all joint surfaces. This cartilage allows the talus to glide against its neighbor bones.
Description
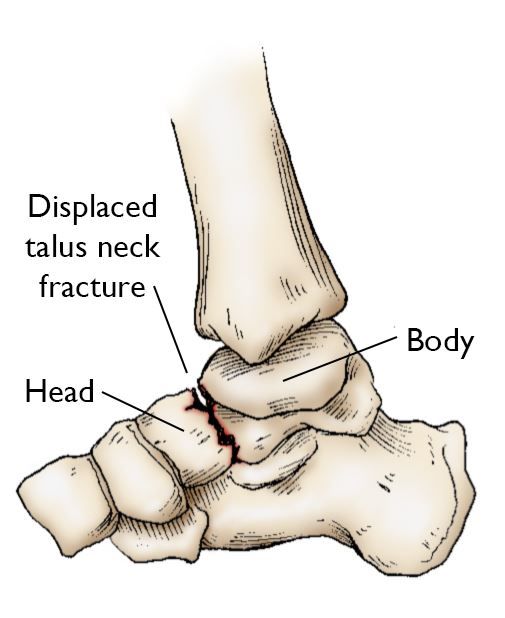
Fractures can occur in all parts of the talus bone. Most commonly, the talus breaks in its mid-portion, called the "neck." The neck is between the "body" of the talus, under the tibia, and the "head" of the talus, located further down the foot.
The talus may also fracture through a prominence (bony bump) on the outside of the bone called the lateral process. Lateral process fractures occur when the ankle is forced out to the side and are commonly seen in snowboarding injuries.
Talus fractures can be classified by the location of the break and by how much the pieces of bone have displaced (moved out of their normal position).
Minimally displaced or stable fractures. In this type of fracture, the bones are well-aligned and usually stay in place during healing. Surgery to repair the bones is not required.
Displaced fracture. A displaced fracture occurs when the bone breaks and the pieces move out of their anatomic position. The amount of displacement relates to the force of the injury — the greater the force, the more the bones may move out of place.
Highly displaced fractures are more likely to be unstable. They often require surgery to restore the alignment and give the best chance for a return to normal function of the foot and ankle.
In addition to fracture location and displacement, it is important to know if the fracture is open or closed.
Open fracture: When broken bones break through the skin, the injury is called an open or compound fracture.
Open fractures often involve greater injury to the surrounding muscles, tendons, and ligaments. In addition, open fractures expose the fracture site to the environment (air, dirt, water, etc.), allowing debris from the outside to get into the wound. For this reason, these fractures have a higher risk of infection and often take a longer time to heal than closed fractures (fractures that do not have a break through the skin).
Cause
Most talus fractures are the result of high-energy trauma such as a motor vehicle collision or a fall from height. Injuries from sports, especially snowboarding, are another, though less common, cause of talus injuries.
Symptoms
Patients with talus fractures usually experience:
- Acute pain
- Inability to walk or bear weight on the foot
- Considerable swelling, bruising, and tenderness
Doctor Examination
Most people with talus fractures will go to an urgent care center or emergency room for initial treatment because of the severity of their symptoms.
Physical Examination
After reviewing your symptoms and medical history, your doctor will do a careful examination. During the exam, they will:
- Examine your foot and ankle carefully to see if there are any cuts from the injury.
- Check to see if you can move your toes and can feel things on the bottom of your foot. In some cases, nerves may be injured at the same time that the bone is broken.
- Check your pulse at key points of the foot to be sure that there is good blood flow to the foot and toes.
- Check to see that pressure from fluids is not building up in the muscles of the leg, a condition called compartment syndrome. Compartment syndrome is a medical emergency. It can result in loss of sensation and function, and it requires immediate surgery once it is diagnosed.
- Determine if you have any other injuries by examining the rest of your injured foot, as well as your legs, pelvis, and spine.
Imaging Tests
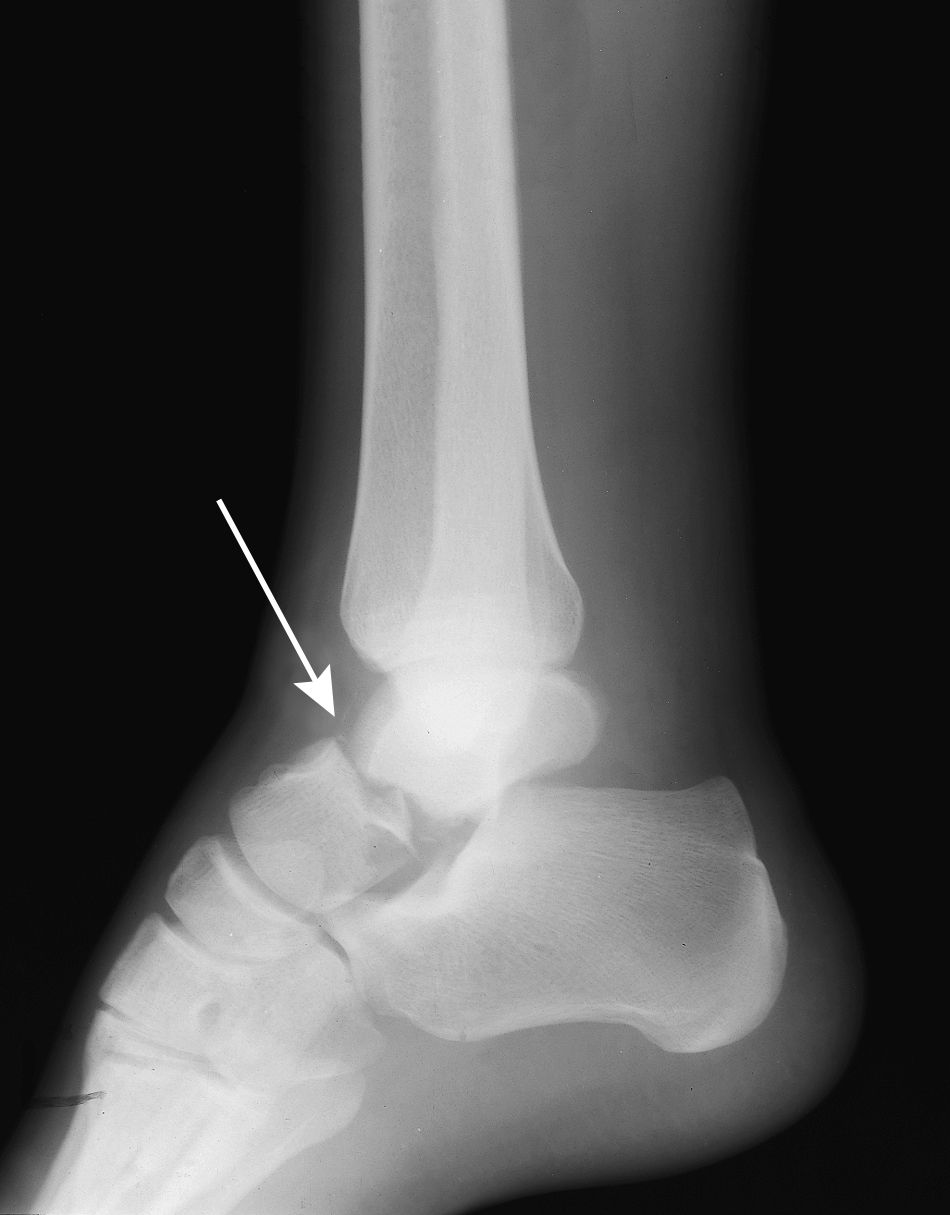
Information from diagnostic imaging tests will help your doctor decide whether surgery is required and will be critical for surgical planning.
- X-rays. X-rays are the most common and widely available diagnostic imaging technique. An X-ray can show if the bone is broken and whether there is displacement (pieces of bone are out of place). It can also show how many pieces of bone there are.
- Computerized tomography (CT) scan. If your doctor still needs more information after viewing your X-rays, they may order a CT scan. A CT scan shows a cross-sectional image of your foot. It can provide valuable information about the severity of the fracture by helping your doctor see the fracture lines more clearly.
Treatment
Immediate first aid treatment for a talus fracture, as with any painful ankle injury, is to apply a well-padded splint around the back of the foot and leg to immobilize (hold still) and protect the limb. The splint will typically extend from the toe to the upper calf.
Elevating the foot above the level of the heart helps to minimize swelling and pain.
Specific treatment depends on the severity and the type of fracture, so it is important to seek medical attention.
Nonsurgical Treatment
Many talus fractures require surgery because of the high-energy force that creates the injury. Stable, well-aligned fractures, however, can often be treated without surgery. This is usually done with a combination of immobilization and then rehabilitation.
Casting. A cast will hold the bones in your foot in place while they heal. You will have to wear a cast for 6 to 8 weeks. During this time, you will be asked to limit the amount of pressure you put on your foot. The goal is for the bone to heal enough for you to bear weight on it without the risk that it will move out of position.
Rehabilitation. When the cast is removed, your doctor will give you exercises to help restore range of motion and strengthen your foot and ankle.
Surgical Treatment
If the bones have shifted out of place (displaced), surgery to internally set and stabilize the broken pieces results in the best outcome and reduces the risk of future complications.
Open reduction and internal fixation. During this operation, the bone fragments are first reduced (positioned back into their normal alignment). They are then held together with special screws or metal plates and screws.
Recovery
Bones have a remarkable ability to heal. The more severe your injury, however, the longer your recovery may be. After surgery, your foot will be in a splint or cast from 2 to 8 weeks. This depends on the nature of the injury and how well the healing progresses. Your doctor will take X-rays at specific points during your recovery to ensure that the bones stay in position and are healing properly.
Pain Management
After surgery, you will feel pain. This is a natural part of the healing process. Your doctor will work to reduce your pain, which can help you recover from surgery faster.
Medications are often prescribed for short-term pain relief after surgery. Many types of medicines are available to help manage pain, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics. Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids.
Be aware that although opioids help relieve pain after surgery, their use has risks and complications. These medications can be addictive and potentially dangerous. Opioid dependency and overdose have become critical public health issues in the U.S. It is important to use opioids only as directed by your doctor, to use as little as possible for as short a time as possible, and to stop taking them as soon as your pain begins to improve. Talk to your doctor if your pain has not begun to improve within a few days of your surgery.
Learn more: Prescription Drug Safety in Orthopaedic Surgery
Early Motion
Many doctors encourage motion of the foot and ankle early in the recovery period, as soon as your pain allows.
- Patients who have had surgery are instructed to begin moving the affected area as soon as the wound heals.
- Patients who are treated without surgery will work on regaining motion in the foot and ankle after the cast is removed.
Physical Therapy
Specific physical therapy exercises can improve the range of motion in your foot and ankle and strengthen supporting muscles.
Weightbearing
When you begin walking, you may need to use a cane or crutches and wear a special boot. You will not be able to put all of your weight on your foot for up to 2 to 3 months. If you place too much weight on your foot too soon, the bone pieces may move out of place. Be sure to follow your surgeon's directions.
As your break heals and your pain improves, you will be allowed to put more pressure on your foot.
Complications After Talus Fractures
Avascular Necrosis (AVN)
With unstable talus fractures, the blood flow to the bone can be disrupted at the time of the injury. Sometimes, the blood supply simply returns to the bone and normal healing begins. In other cases, however, the bone does not survive, leading to a gradual and painful collapse of the bone. This condition is called avascular necrosis (AVN) or osteonecrosis.
When the bone collapses, the articular cartilage covering the bone is also damaged. Without this smooth cartilage, bone rubs against bone, leading to increased pain, arthritis and loss of motion and function. The more severe the talus fracture, the more likely it is that AVN will occur. Even fractures that are treated appropriately, including those that are treated surgically, may develop AVN.
Posttraumatic Arthritis
Posttraumatic arthritis is a type of arthritis that develops after an injury. Even when your bones heal normally, the cartilage protecting the bones can be damaged, leading to pain and stiffness over time.
A significant percentage of talus fractures result in some degree of posttraumatic arthritis. In cases of extreme arthritis or avascular necrosis that limit activity, additional surgery, such as a joint fusion or ankle replacement, may be the best option to relieve symptoms.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.