Diseases & Conditions
Soft Tissue Sarcomas
Soft tissue sarcomas (STS) are cancerous tumors that begin in the soft tissues of the body such as muscles, fat, joints, nerves, and blood vessels.
These tumors are not common, accounting for about 1% of all cancers. It is estimated that there are approximately 30 new cases of soft tissue sarcoma per year among every 1 million people. The most recent data from the National Cancer Institute reports approximately 13,700 new cases in the U.S. each year.
There are many types of soft tissue sarcoma. Although all sarcomas are serious, some are more aggressive than others. Treatment for soft tissue sarcoma involves surgery to remove the tumor. Larger, more aggressive tumors may also require radiation therapy and chemotherapy.
Description
There are more than 50 different types of soft tissue sarcomas. Some types are identified by the kind of tissue from which they originated:
- Fat: Liposarcoma
- Fibrous tissue: Fibrosarcoma
- Smooth muscle (seen in blood vessels, uterus, and intestines): Leiomyosarcoma
- Skeletal muscle (seen in trunk and limbs): Rhabdomyosarcoma
- Blood vessels: Angiosarcoma
- Nerves: Malignant peripheral nerve sheath tumors (MPNST)
A few other subtypes of soft tissue sarcomas include undifferentiated pleomorphic sarcoma (UPS), synovial sarcoma, clear cell sarcoma, alveolar soft parts sarcoma, epithelioid sarcoma, and myxofibrosarcoma.
Cause
- In most cases, the cause of soft tissue sarcoma is not known.
- Some studies have connected soft tissue sarcomas to exposure to certain chemicals, high-dose radiation, or certain viral infections.
- There are a few genetic conditions that increase the risk for sarcoma, including Li-Fraumeni Syndrome, neurofibromatosis type I, or retinoblastoma.
Symptoms
- For many people, the first symptom of soft tissue sarcoma is a painless slow-growing lump in the trunk or limbs.
- As the mass grows, it may begin to press upon nerves or muscles and possibly cause pain, numbness, and/or skin breakdown.
Doctor Examination
It is much more common for a soft-tissue mass or lump to be benign (noncancerous) than malignant (cancerous). Your doctor will perform a physical examination and use imaging and other tests to identify the type of mass you have.
If your doctor determines that you may have soft tissue sarcoma, they will refer you to a cancer specialist (oncologist).
Diagnosing and Staging Soft Tissue Sarcoma
Imaging and other tests will help determine the size and location of the tumor and whether any other areas of the body are involved. They will also help determine the prognosis (prediction of outcome for a disease) of a soft tissue sarcoma. In general, masses that are bigger than 5 cm and located deep in the tissues are more likely to be cancerous.
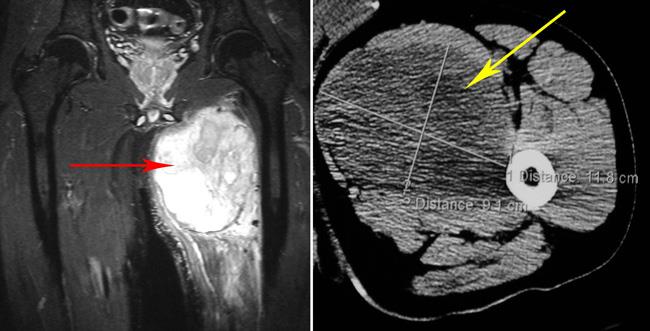
Magnetic resonance imaging (MRI) scan. An MRI can help identify the tumor's size and depth since it clearly shows the tumor's relationship to normal muscle, fat, nerves, and blood vessels. It can also be used to check the tumor's response to treatment and observe the progression of the disease.
X-rays. X-rays provide images of dense structures such as bone. In the case of soft tissue sarcomas, X-rays can be used to evaluate whether or not the bone is involved with the tumor. They can also show if there is any hardening or bone tissue inside the tumor.
X-rays may help in the diagnosis of certain tumors that may contain calcium deposits, such as synovial sarcoma and liposarcoma.
Computerized tomography (CT) scan. Like an X-ray, a CT scan can be used to clearly outline how much bone is involved with a tumor. It is also useful in detecting the spread of cancer to the lungs, abdomen, and pelvis. A CT scan is sometimes used instead of an MRI for masses that are located around a metal implant.
Biopsy. A biopsy may be necessary to confirm the diagnosis of soft tissue sarcoma. In a biopsy, a tissue sample of the tumor is taken and examined under a microscope.
- Your doctor may give you a local anesthetic to numb the area and take a sample using a needle.
- A biopsy can also be performed as a small operation.
MRI imaging is used to guide the biopsy. The doctor is very careful when taking biopsy samples to avoid the risk of contaminating normal tissue with cancer cells.
Other tests. Bone scans are used to detect the spread of a tumor into a bone or to determine if the tumor has spread to other bones in the body. Positron emission tomography (PET) scans may be helpful in monitoring a tumor's response to treatment or in determining if there may be other tumors hidden in the body.
Grading. The tumor grade is determined by the pathologist after biopsy is performed. Sarcomas can be classified as Grade 1 (low-grade), Grade 2 (intermediate-grade), or Grade 3 (high-grade) based on the appearance of the cells under the microscope.
Staging. Computed tomography (CT) scans of the chest, abdomen, and pelvis are usually recommended for initial staging. Staging is important to determine if the tumor has spread to any other parts of the body. Most commonly, sarcomas spread to the lungs.
Occasionally, sarcoma can spread to the lymph nodes or other organs. Sometimes, PET scans may be helpful in monitoring a tumor's response to treatment or in seeing if there are other tumors hidden in the body.
Determining the stage of your sarcoma will require the diagnosis, tumor size, location, grade, and presence of any tumors in other locations.
Treatment
A multidisciplinary approach is needed in the treatment of soft tissue sarcomas. The treatment team includes the surgeon and oncologists (such as medical oncologists and radiation oncologists) and includes discussion with radiologists and pathologists.
The main goal of treatment is to control the local and distant spread of the tumor while maintaining, as best as possible, function and quality of life. With soft tissue sarcoma, this requires adequate resection (removal of the tumor) through a properly planned surgery.
Surgery
The extent of the surgery performed depends on several factors, including the amount of tissue that needs to be removed and the functional outcome that is expected afterwards.
Excision. If the sarcoma has not spread, surgery is done to remove the tumor and any surrounding tissues that could potentially be affected by the cancer. Even healthy tissues may need to be removed to reduce the chance of the cancer returning.
Advances in reconstructive surgery allow the transfer and repair of skin, blood vessels, and nerves. This makes it possible to remove more of the tissue around the tumor while preserving the function of the limb.
Amputation. If adequate tumor removal would mean sacrificing important nerves, blood vessels, and muscle structures, amputation may be necessary. Although limb preservation is the goal, in some cases it is not possible. Additionally, if sparing the limb results in a limb that is not useful, an amputation followed by proper artificial limb fitting could provide better function and quality of life.
Radiation Therapy
Radiation therapy is often combined with surgery to lower the risk of the tumor returning to the same location. Radiation can be given either before or after the tumor is removed. The timing of the radiation depends on the tumor site and the doctor's judgment. Radiation is delivered by a doctor called a radiation oncologist.
Chemotherapy/Systemic Therapy
The role of chemotherapy in treating soft tissue sarcomas depends on several factors.
For patients with large (greater than 5 cm) and high-grade sarcomas, a conversation about the risks and benefits of chemotherapy is recommended. At best, there is modest improvement in survival with chemotherapy.
The chemotherapy drugs that have been most effective against soft tissue sarcomas are:
- Doxorubicin (Adriamycin®)
- Ifosfamide (Ifex®)
Other chemotherapy drugs that may be used to treat sarcoma include gemcitabine and docetaxel.
Newer drugs that target specific cellular traits are being researched. Occasionally, a soft tissue sarcoma has a genetic mutation that makes certain medications more effective.
- The first drug to work by this method was imatinib (Gleevac®), which has been effective at treating a specific type of sarcoma — gastrointestinal stromal tumor (GIST).
- There is also promising evidence with other drugs, including larotrectinib (NTRK gene fusion), trabectedin, eribulin, pembrolizumab, pazopanib, and cabozantinib, to name a few.
Discussion about systemic therapy (chemotherapy or other medical therapy) is personalized to your tumor, stage, and overall health status. These decisions are led by a medical oncologist.
Recovery
Every type of tumor has its own treatment course, and every patient will respond to disease and treatment differently.
After treatment of a soft tissue sarcoma, you will continue to see your doctor for regular follow-up visits. Tumors that come back may pose a serious problem, so it is important to detect them early. A recurrent tumor could regrow at the original site or in a distant site (metastasis) such as the lungs.
For some patients whose cancer returns — whether in the same site or a metastasized location — additional surgery to cut away the disease can provide a better outcome and extend their life.
Types of Soft Tissue Sarcoma
The World Health Organization has identified 19 categories and more than 50 histologic (microscopic makeup of tissues) types of soft tissue sarcomas, including those described below.
Liposarcoma
- This tumor is composed of fatty tissue that usually appears as an enlarging, painless mass deep in the muscles of the limbs.
- It can also occur in the abdomen or buttock, where it can stay undetected for a long period of time and possibly evolve to a more aggressive type.
- It is commonly seen in adult men and women over the age of 50.
- The course of the disease depends on the type and location of the tumor.
- Surgical removal of the tumor is needed.
There are several types of liposarcoma.
- A well-differentiated liposarcoma is now referred to as an atypical lipomatous tumor if it occurs in the limbs because it does not metastasize or cause death. Fatty tumors that occur in the abdomen or pelvis can still referred to as well-differentiated liposarcomas because they are more aggressive and tend to recur or metastasize to the lungs.
- The more aggressive dedifferentiated liposarcoma is commonly located in the abdomen, pelvis, or thigh and has a higher chance of recurring locally and spreading to distant areas.
- Another fairly common type is myxoid liposarcoma which, although very rare, occurs in younger patients and is often seen in the deep thigh muscles. The round cell liposarcoma sometimes is seen together with the myxoid type and is prone to recur and spread to other organs.
Fibrosarcoma
- This is a malignant tumor made up mostly of cells of fibrous tissues and collagen.
- Two different clinical behaviors characterize the two main groups of fibrosarcoma:
- Adult fibrosarcoma occurs in middle-aged to older adults and is commonly seen in the deep soft tissues of the limbs and trunk. This tumor can be associated with previous radiation therapy. It can spread to the lungs and bone. The mortality rate can be rather high depending on the aggressiveness (grade) of the tumor cells.
- Infantile fibrosarcoma differs from the adult form in many ways. Most cases are congenital (present at birth) and almost never occur after the age of 2 years. It has a better outcome with a lower chance of tumor regrowth and spread. These tumors commonly have an NTRK gene fusion and can be treated medically with the targeted drug larotrectinib.
Myxofibrosarcoma
- This is the most common malignant soft tissue tumor in late adulthood.
- It may be divided into subtypes based on which cells are the dominant cells.
- The most common location is in the lower limbs, particularly the thigh region, where it can appear as a painless mass.
- Less frequently, it can grow in the abdomen and be undetected until the patient starts to develop symptoms related to an increase in abdominal pressure, such as bloating, frequent urination, or constipation.
- There have been some reports of myxofibrosarcoma developing in patients who received high doses of radiation in the past, and other reports suggest a viral or a chemical cause. In most cases, the origin is not known.
Rhabdomyosarcoma
- This is the most common malignant soft tissue tumor in children.
- It occurs most often in young children or teenagers.
- The tumor can grow quite large in a short period of time, causing pain, discomfort, or joint stiffness due to pressure on the adjacent soft tissue structures.
- It is seen mostly in the head and neck region. In 25% of cases, it is found on the trunk and limbs.
- This tumor is aggressive and requires multidisciplinary treatment with chemotherapy, surgery, and radiation therapy.
Synovial Sarcoma
- These tumors occur in the muscle of both the upper and, more frequently, lower limbs.
- They are common in early adulthood, particularly among young males in their 30s.
- The mass may remain small for some time but can noticeably enlarge.
- Sometimes there is a history of trauma before the mass appears.
- Synovial sarcoma has a signature genetic translocation on t(X;18), meaning there is a genetic cause for this subtype of sarcoma.
- If a synovial sarcoma is larger than 5 cm, multidisciplinary treatment is usually recommended with chemotherapy, radiation therapy, and surgery.
- The risk of spread, mostly to the lungs, can be high and can take as long as 5 to 10 years. That is why 10 years of long-term follow-up or surveillance is recommended.
Epithelioid Sarcoma
- This rare tumor most often develops in the forearm and hand but may also be seen on the trunk or legs.
- Patients typically are males in their teens or 20s.
- The tumor can be deceiving because it can mimic benign (noncancerous) masses in the hand, including small tumors just beneath the skin that may resemble an infection.
- The source of this tumor is not clear, but a genetic abnormality involving an immature cell type is likely. There is no known hereditary pattern (how certain traits are passed down from one generation to another)
- Risk of recurrence (the tumor coming back) is very high and is usually due to an incomplete removal of the initial lesion. It can spread to the lungs and lymph nodes and affect the likelihood of survival.
Alveolar Soft Part Sarcoma
- This rare, slow-growing tumor occurs mainly in adolescents and young adults.
- It develops in the deep thigh area in nearly half (50%) of cases, although it tends to develop in the head and neck region in younger children.
- Other organs, such as the lungs, bones, and brain, may be affected and cause a patient to seek treatment.
- In some individuals, there appears to be a relationship between pregnancy and the occurrence of alveolar soft part sarcoma.
- Survival depends on the size of the tumor and whether there is distant spread (metastasis). However, unlike other types of cancers, metastatic tumors in the lungs may grow very slowly over many years.
Clear Cell Sarcoma
- Clear cell sarcoma is a tumor common in young adults between the ages of 20 and 40.
- It is believed to be caused by a genetic abnormality even though no known hereditary pattern can be identified.
- It grows just beneath the skin, affecting tendons and muscle sheaths of the limbs, particularly in the foot and ankle region.
- The mass can cause pain and patients sometimes develop lymph node enlargements in the armpits or groin signifying cancer spread.
- Recurrences and distant spread to the lungs and bone are common and can occur even after 10 years. Long-term follow-up is therefore recommended.
Leiomyosarcoma
- Middle-aged and older adults are commonly affected by this tumor
- It tends to begin in blood vessels of the trunk and limbs, and it is also found in the uterus. It may spread to the lungs and the liver.
- It can obstruct blood flow to vital organs such as the liver, kidneys, and pancreas.
- Possible symptoms include jaundice, nausea, abdominal distention, and leg swelling.
- Leiomyosarcoma tumors located in the limbs are easier to control than the more common abdominal tumors, which tend to be larger and more difficult to remove.
Gastrointestinal Stromal Tumor (GIST)
- A rare tumor arising in the abdomen, GIST tends to occur in adults.
- Tumors may become quite large before being noticed. For this reason, complete surgical removal is more difficult to achieve than with sarcomas in the limbs.
- The development of drug therapy targeted at specific characteristics of cancer cells in GIST has improved the treatment of this tumor compared with surgical removal alone. The first drug that worked with this method was imatinib (Gleevac®). Other drugs are in development and testing phases.
Outcomes
Most major cancer centers report the overall survival rate for patients with soft tissue sarcoma in the range of 65% at 5 years.
Survival rates depend on the patient's age and gender as well as the size, grade, and stage of the tumor when it was first identified. The best results are achieved with tumors that:
- Are small (less than 5 cm)
- Are superficial
- Are less aggressive (low-grade)
- Have not spread to lymph nodes and other organs
Complete surgical removal is required to cure the cancer.
Radiation therapy is recommended to reduce the risk of local recurrence (the cancer coming back).
Chemotherapy is recommended in select circumstances or if the patient has metastatic disease.
Incomplete surgical removal and the presence of distant spread to other organs will lead to a poorer outcome. After the tumor has been removed, there is a 5 to 20% chance of it regrowing at the same site and a 30 to 50% chance of it growing in a different organ. Surgical removal of a metastatic lesion (metastatectomy) is possible and is recommended for appropriate patients.
The future of soft tissue sarcoma treatment:
- Relies heavily on gathering more data to define the role of chemotherapy for soft tissue sarcoma management and of combination therapy for patients with poor prognoses and distant spread.
- Depends upon development of new drugs targeted at specific tumor cell characteristics.
Ultimately, better disease detection and diagnosis, improved surgical techniques, better radiation therapy methods, and more effective systemic agents (chemotherapy, targeted therapy, immunotherapy) will give patients a better chance of surviving soft tissue sarcomas.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.