Diseases & Conditions
Shoulder Joint Labral Tear
This article was written and/or reviewed by a member of American Shoulder and Elbow Surgeons (ASES).
Advances in medical technology have made it possible for doctors to identify and treat injuries that went unnoticed 30 to 40 years ago.
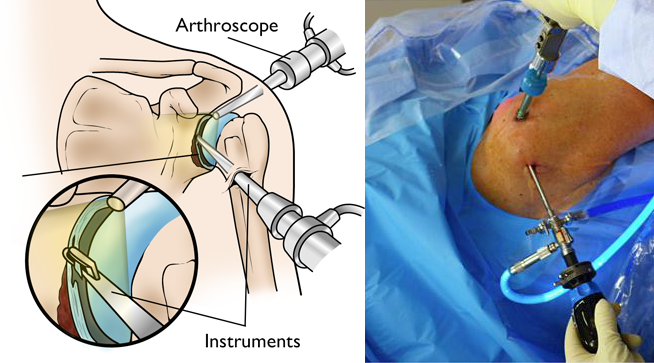
For example, orthopaedic surgeons can now use miniaturized instruments and cameras (arthroscopic surgery) to see inside a joint. This enables them to identify and treat a shoulder injury called a glenoid labrum tear, also known as a labral tear.
Anatomy
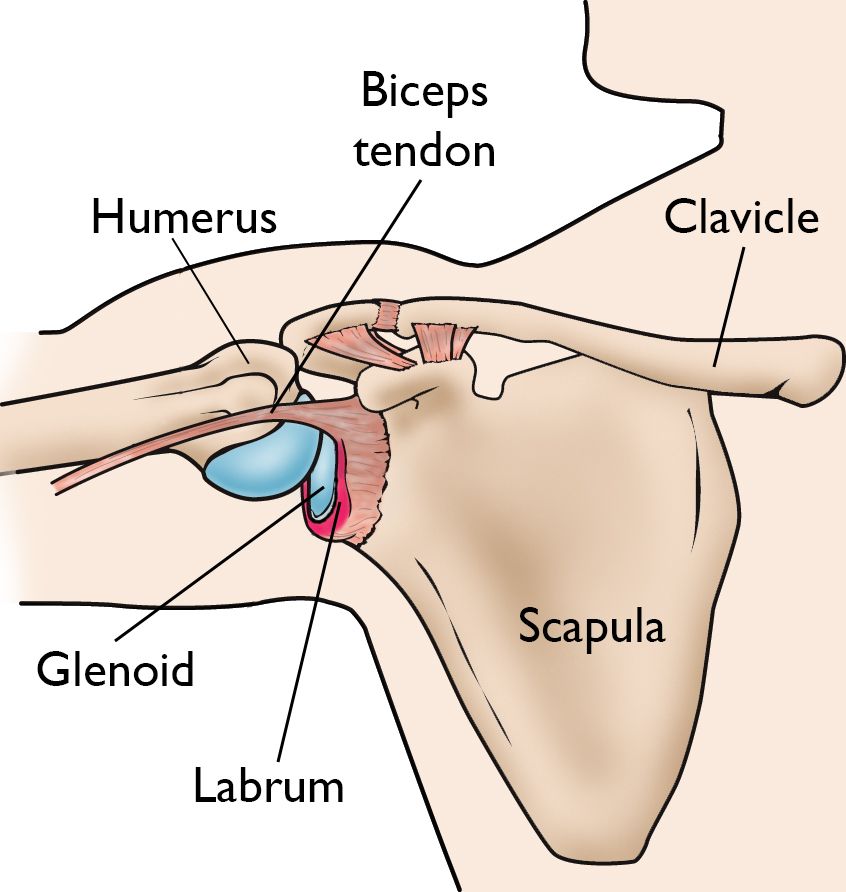
The shoulder is a ball-and-socket joint made up of three bones:
- The humerus (upper arm bone)
- The scapula (shoulder blade)
- The clavicle (collarbone)
The head of the upper arm bone (humeral head) rests in a shallow socket in the shoulder blade called the glenoid. The head of the upper arm bone is usually much larger than the socket, and a soft fibrous tissue rim called the labrum surrounds the socket to help stabilize the joint. The rim deepens the socket by up to 50% so that the head of the upper arm bone fits better. In addition, it serves as an attachment site for several ligaments.
Description
There are several types of labral tears:
- A SLAP lesion (superior labrum, anterior [front] to posterior [back]) is a tear of the labrum that usually occurs on the upper part of the socket and may also involve the origin, or starting point, of the long head of the biceps tendon.
- A tear of the front part of the labrum at the bottom of the socket is called a Bankart lesion. This usually happens from an interior shoulder dislocation (a dislocation when the humeral head comes out of the front of the socket).
- A tear of the labrum can also occur in the back part of the socket. This is called a posterior labral tear. It can be a traumatic tear due to injury, or it may be degenerative due to normal wear and tear.
Cause
Injuries to the tissue rim surrounding the shoulder socket can occur from acute trauma or repetitive shoulder motion. Examples of traumatic injury include:
- Falling on an outstretched arm
- A direct blow to the shoulder
- A sudden pull, such as when trying to lift a heavy object
- A violent overhead reach, such as when trying to stop a fall or slide
Throwing athletes or weightlifters can experience glenoid labrum tears as a result of repetitive shoulder motion.
Symptoms
The symptoms of a tear in the shoulder socket rim are very similar to those of other shoulder injuries. Symptoms include
- A sense of instability in the shoulder
- Shoulder dislocations
- Pain, usually with overhead activities
- Catching, locking, popping, or grinding
- Occasional night pain or pain with daily activities
- Decreased range of motion
- Loss of strength
Doctor Examination
If you are experiencing shoulder pain, your doctor will:
- Take a history of your injury. You may be able to remember a specific incident, or you may note that the pain gradually increased.
- Do several physical tests to check range of motion, stability, and pain.
- Request X-rays to see if there are any other reasons for your problems.
Because the rim of the shoulder socket is soft tissue, X-rays will not show damage to it. The doctor may order a computed tomography (CT) scan or magnetic resonance imaging (MRI) scan. In both instances, a contrast medium may be injected to help detect tears. However, the diagnosis will ultimately be made with arthroscopic surgery.
Treatment
Until the final diagnosis is made, your physician may prescribe anti-inflammatory medication and rest to relieve symptoms. They may also recommend rehabilitation exercises to strengthen the rotator cuff muscles.
In many cases, nonsurgical methods are effective in relieving symptoms and healing the injured structures. If these nonsurgical measures are insufficient, or if the symptoms return, your doctor may recommend surgery.
Depending on your injury, your doctor may perform a traditional, open procedure, or an arthroscopic procedure using small incisions and miniature instruments.
During arthroscopic surgery, the doctor will examine the rim and the biceps tendon.
- If the injury is confined to the rim, without involving the tendon, the shoulder is still stable. The surgeon will remove the torn flap and correct any other associated problems.
- If the tear extends into the biceps tendon or if the tendon is detached, the biceps tendon may be considered unstable. The surgeon will need to repair or transfer the tendon to a safer location using absorbable tacks, screws, or sutures (stitches). Studies have shown that the various techniques produce the same outcomes; no one technique is better than the others.
- Tears of the labrum located in the bottom half of the socket may be associated with shoulder instability. The surgeon will reattach the labrum and ligaments and tighten the shoulder socket tissue by folding it over and "pleating" it. This procedure may be done arthroscopically or open with a small incision on the front of the shoulder.
It should be noted that not all tears in the shoulder can be made better with surgery. If your tear cannot be made better with surgery, your surgeon may recommend nonsurgical management.
Rehabilitation
After surgery, you will need to keep your shoulder in a sling for 2 to 6 weeks, depending on your doctor's recommendation. Your doctor will also prescribe gentle, passive, pain-free range-of-motion exercises. When the sling is removed, you will need to do motion and flexibility exercises and gradually start to strengthen your shoulder.
Athletes can usually begin doing sport-specific exercises 12 weeks after surgery, although it will be 4 to 6 months before the shoulder is fully healed.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.