Diseases & Conditions
Scapular (Shoulder Blade) Disorders
This article was written and/or reviewed by a member of American Shoulder and Elbow Surgeons (ASES).
The scapula (shoulder blade) is a bone, shaped like a triangle, on the upper back. The bone is surrounded and supported by a complex system of muscles that work together to help you move your arm. If an injury or condition causes these muscles to become weak or imbalanced, it can alter the position of the scapula at rest or in motion.
A change in scapular positioning or motion:
- Can make it difficult to move your arm, especially when performing overhead activities
- May cause your shoulder to feel weak
- Can lead to injury if the normal ball-and-socket alignment of your shoulder joint is not maintained
Treatment for scapular disorders usually involves physical therapy designed to strengthen the muscles in the shoulder and restore the proper position and motion of the scapula.
Anatomy
The shoulder joint is a ball-and-socket joint. The head of the humerus (upper arm bone) is the ball, and the scapula (shoulder blade) forms the socket.
The scapula and arm are connected to the body by multiple muscle and ligament attachments. The front and top of the scapula (acromion) is also connected to the clavicle (collarbone) through the acromioclavicular joint.
As you move your arm around your body, your scapula must also move to maintain the ball and socket in normal alignment.
Description
Disorders of the scapula result in a change in the:
- Normal resting position of the scapula, or
- Normal motion of the scapula as the arm moves
The medical term for these alterations is scapular dyskinesis ("dys"= alteration of, "kinesis" = movement).
In most cases, alterations of the scapula can be seen by looking at the patient from behind. The medial (inner) border of the affected shoulder blade will appear more prominent than the one on the opposite side. This prominence (bump) will often be exaggerated as the patient moves their arm away from the body. This is commonly called a "winged" scapula.
Cause
Causes of scapular dyskinesis include:
- Weakness, imbalance, tightness, or (rarely) detachment of the muscles that control the scapula
- Injuries to the nerves that supply the muscles
- Injuries to the bones that support the scapula or injuries within the shoulder joint
Symptoms
The most common symptoms of scapular dyskinesis include:
- Pain and/or tenderness around the scapula, especially on the top and medial (inner) border
- Weakness in the affected arm — your arm may feel tired or "dead" when you try to use it vigorously
- Fatigue with repetitive activities, especially overhead movements
- Limited range of motion — you may be unable to raise your arm above shoulder height
- A crunching or snapping sound with shoulder movement
- Noticeable protrusion or "winging" of the scapula
- A drooped or forward tilted posture on the affected side
Doctor Examination
Physical Examination
Your doctor will talk to you about your medical history and general health and ask about your symptoms. They will examine your entire shoulder and scapula, looking for injury, weakness, or tightness. In most cases, the physical exam will include the following:
Visual observation. Your doctor will look at your affected scapula from behind, comparing it to the other side.
To see if you have scapular dyskinesis, your doctor may ask you to move your arms up and down a few times, sometimes with light weights in your hands, or to put both hands on a wall and push away from it. This will usually reveal any weakness in the muscles and display the abnormal motion patterns.
Manual muscle testing. Your doctor will perform strength testing of your shoulder and scapular muscles to determine if muscle weakness is contributing to the abnormal scapular motion.
Corrective maneuvers. Specific tests involve corrective maneuvers that will help your doctor learn more about your condition. These tests include:
- Scapular assistance test (SAT). In this test, the doctor will apply gentle pressure to your scapula to assist it upward as you elevate your arm. If your symptoms are relieved and the arc of motion is increased, it is an indication that your muscles are not strong enough to raise your arm.
- Scapular retraction test (SRT). In this test, the doctor will test your arm strength by pushing down on your extended arm. They will then manually place the scapula in a retracted position and test your strength again. In patients with scapular dyskinesis, muscle strength will improve when the shoulder blade is retracted.
- Special tests. There are several other specific tests that your doctor may perform to evaluate your shoulder blade based on what they find during the exam and how the scapula looks.
Imaging Tests
Imaging tests are not always necessary to diagnose scapular dyskinesis. Your doctor may, however, order imaging, such as an X-ray, computed tomography (CT) scan, or magnetic resonance imaging (MRI) scan, if they suspect a bony abnormality of the scapula (such as an osteochondroma) or an injury to another part of the shoulder.
If your doctor thinks there may be a nerve injury, they may order a nerve conduction study to see how the nerves are functioning.
Treatment
Nonsurgical Treatment
In almost all cases, the symptoms of scapular dyskinesis will improve with nonsurgical treatment.
Nonsurgical treatment may include:
Nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs, such as ibuprofen and naproxen, can help relieve pain and swelling.
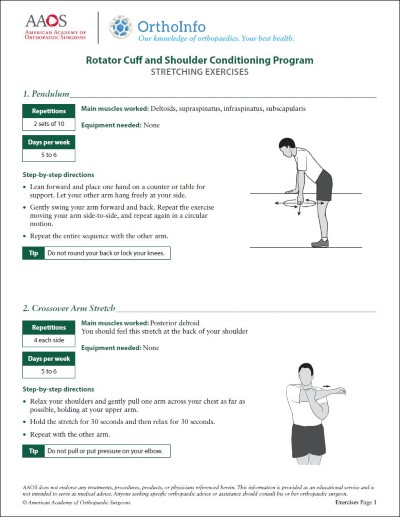
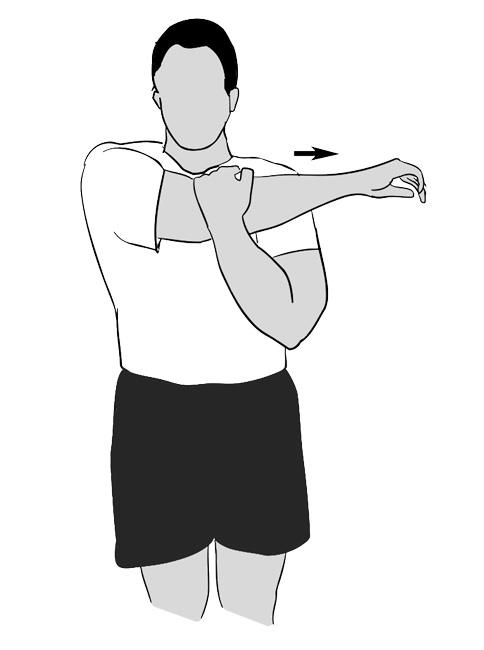
Physical therapy. Your doctor or physical therapist will provide an exercise program that targets the specific causes of your dyskinesis. Physical therapy usually focuses on:
- Strengthening the muscles that stabilize and move the scapula
- Stretching the tight muscles that are limiting scapular motion
Heat therapy. Soaking in a hot bath or using a heating pad may help relieve tightness in the shoulder muscles.
In addition, it is important to:
Practice good posture. As you perform your everyday activities, try to stand and sit properly. To do this, pull your shoulder blades back together, and bend your elbows down and back as if you are trying to put them in your back pockets.
Balance your exercise routine. If you are in a regular home exercise program, make sure your upper body strength sessions are balanced. For instance, for every set of "presses" you perform, you should do 1 set of "flys" and 2 sets of "rows." Your program should also include stretching exercises for your front shoulder muscles and for shoulder joint rotation.
Tell your doctor if your symptoms do not improve with nonsurgical treatment.
Surgical Treatment
Most patients who have general dyskinesis due to muscle weakness or tightness do not need surgery.
However, if your dyskinesis is being caused by an injury to your shoulder joint, your doctor may perform a procedure to repair or reconstruct the injured tissues. This will be followed by rehabilitation to restore the scapula's normal motion.
Long-Term Outcomes
Once the causes of your dyskinesis have been addressed and normal scapular position and motion are restored, your doctor may recommend a maintenance conditioning program of flexibility and strengthening. This is especially important if your job or recreational activities involve vigorous or repetitive shoulder and arm movements. These exercises should be done 3 times a week or as recommended by your doctor.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.