Diseases & Conditions
Pectoralis Tendon Tear
This article was written and/or reviewed by a member of American Shoulder and Elbow Surgeons (ASES).
The pectoralis major tendon attaches the pectoralis major muscle to the humerus (the arm bone). The tendon and muscle provide power to move the arm in several ways:
- Adduction (toward the middle of the body)
- Internal rotation (rotating the arm inward)
- Flexion (lifting the arm)
The pectoralis major tendon is most at risk of tearing when it is under maximum stress. This commonly occurs during what is called an "eccentric load." An example of eccentric load would be on the downward motion of a bench press.
When a pectoralis major tear is caused by an injury, you may have bruising, pain, and difficulty raising your arm. You may also feel a "pop" or a ripping sensation in your chest and arm while contracting the muscle during exercises, such as a bench press or push-up.
Surgical repair is often recommended and has the best results when performed soon after the injury.
Anatomy
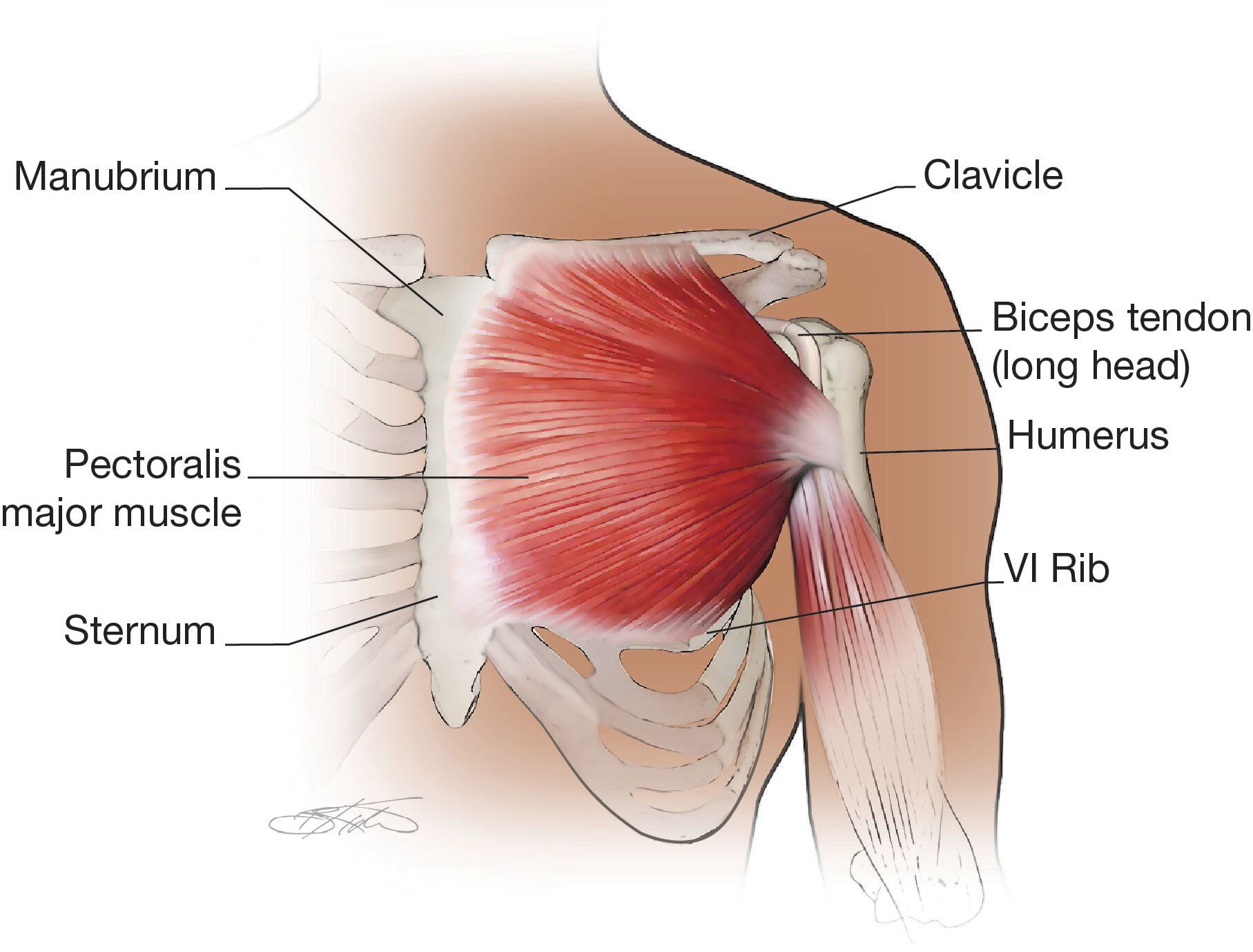
The pectoralis major muscle is a broad, large muscle made up of two parts, or "heads":
- One comes from the sternum (chest bone)
- The other comes from the clavicle (collarbone)
The common tendon attaches the muscle to the humerus (arm bone) about 1/3 of the distance down the arm. This tendon is easily felt as the fingers are placed in the axilla (armpit); the tendon is the large one on the anterior (front) of the armpit.
Description
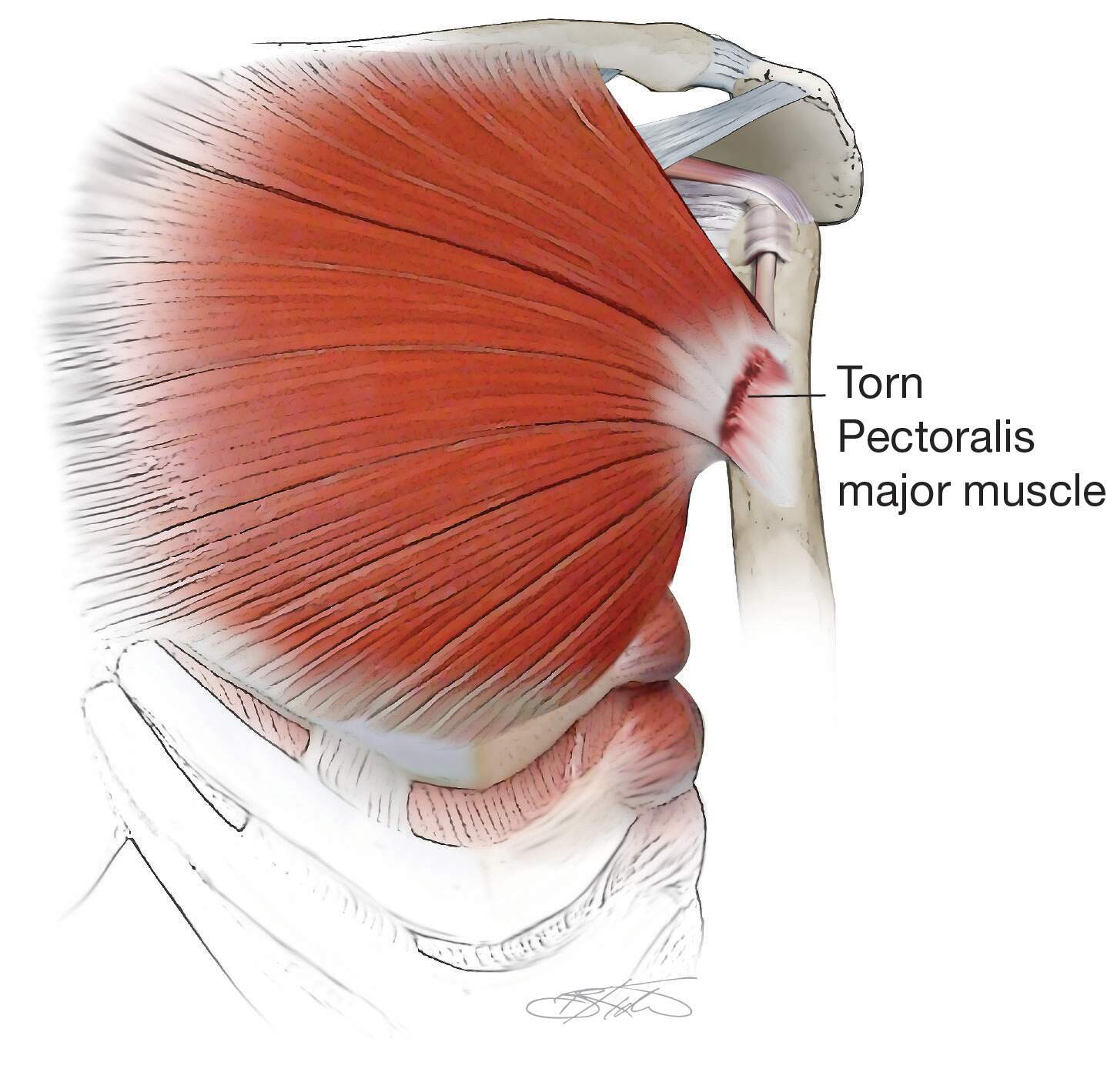
Pectoralis major tendon tears can be partial or complete and may happen:
- At the muscle origin (the spot where it attaches to the collarbone or sternum)
- Within the muscle belly
- At the musculotendinous junction (where the muscle becomes a tendon)
- Most commonly, at the spot where the pectoralis tendon attaches the pectoralis major muscle to the humerus (arm bone)
Risk Factors
There are several risk factors for pectoralis major tear:
- Participating in certain sports or exercise activities, including but not limited to weightlifting, wrestling, windsurfing, gymnastics, boxing, football, rodeo, and waterskiing
- Certain demographic factors, including biological males between the ages of 30 and 60 years
- Anabolic steroid use
Symptoms
- Pectoralis tendon tears typically produce a "pop" and/or a ripping feeling in the arm.
- You may have immediate pain and/or weakness.
- Many people who suffer this injury are unable to continue their exercise.
Other signs may include:
- Pain with pushing motions
- Bruising on the chest/inside arm
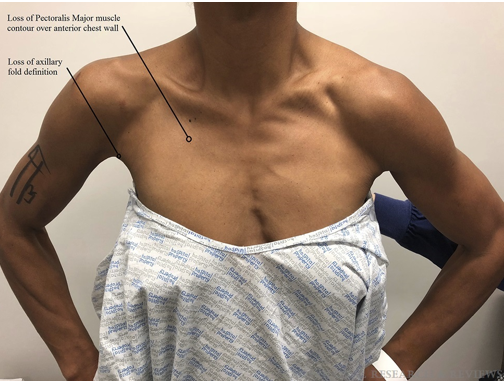
- The chest, curve of the armpits, or nipples look uneven (for instance, one nipple may be lower than the other)
If you have any of these symptoms, please seek medical care immediately. Resting, icing, and anti-inflammatory medications may help with the pain and bruising but will not heal the tear.
Doctor Examination
Physical Examination
The doctor will examine your chest and arm to check:
- The range of motion in your shoulder
- Your strength, especially during internal rotation (rotating your palm toward your belly button)
- Symmetry (evenness) of your chest, nipple lines, and/or armpits
- Whether there is a tendon defect in the armpit
Imaging Tests
X-rays are used to diagnose any fractures, fragments of bone that pulled away with the torn tendon, or a dislocation that may have happened along with the tear.
Your doctor will typically order a magnetic resonance imaging (MRI) scan. Because a routine MRI does not usually image the pectoralis muscle fully, this injury needs a specific MRI of the chest (called a Pectoralis MRI) to see the full extent of the injury. However, if the injury can be clearly diagnosed during the physical exam and getting an MRI would delay surgery, your doctor may not send you for an MRI.
Ultrasound can also be used to diagnose a pectoralis tendon tear.
Treatment
Nonsurgical Treatment
Studies suggest surgical repair has a higher level of patient satisfaction than nonsurgical care. Nonsurgical care is usually reserved for people who are older and not active, or those with incomplete tears.
Initial nonsurgical treatment includes a sling, rest, ice, and non-steroidal anti-inflammatory drugs (NSAIDs), followed by physical therapy.
Although pain can improve over time with nonsurgical treatment, the chest deformity will not go away and you will continue to experience weakness.
Your surgeon will talk to you about which type of treatment is right for you.
Surgical Treatment
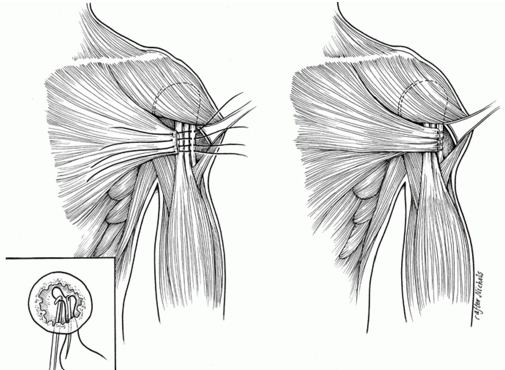
- Surgical repair is usually done under general anesthesia (you are asleep).
- Your surgeon will usually make the incision on the anterior (front) portion of the upper arm.
- The surgeon then reattaches the tendon to the bone. This can be done with sutures using bone tunnels, with implants called buttons or suture anchors, or by directly sewing the tendon back to its stump.
- Occasionally, if the tendon cannot be repaired to the bone or if the tendon is separated from the muscle, the surgeon may use an allograft (donor tissue) to help complete the repair.
Recovery
After surgery, your doctor will prescribe a rehabilitation protocol and likely recommend seeing a physical therapist.
- During the first stage of therapy, it is important to protect the repair. That usually means limiting range of motion and wearing a sling.
- During the next stage, you will start some gentle range of motion exercises to avoid stiffness.
- The last stage involves strengthening exercises.
Both the injury and the surgery to repair it take a long time to heal. Typically, it takes at least 6 months before you can return to full activity, and it may take you 1 or more years to regain full strength.
Possible Complications After Surgery
- Re-rupture (retear) is uncommon but happens in 5 to 7% of patients who undergo a repair.
- Most commonly, the tendon fails to fully heal and the sutures pull through the tendon.
- Some patients will have stiffness, pain, and/or loss of strength.
- The chest may also continue to appear uneven after surgery.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.