Diseases & Conditions
Patellofemoral Arthritis
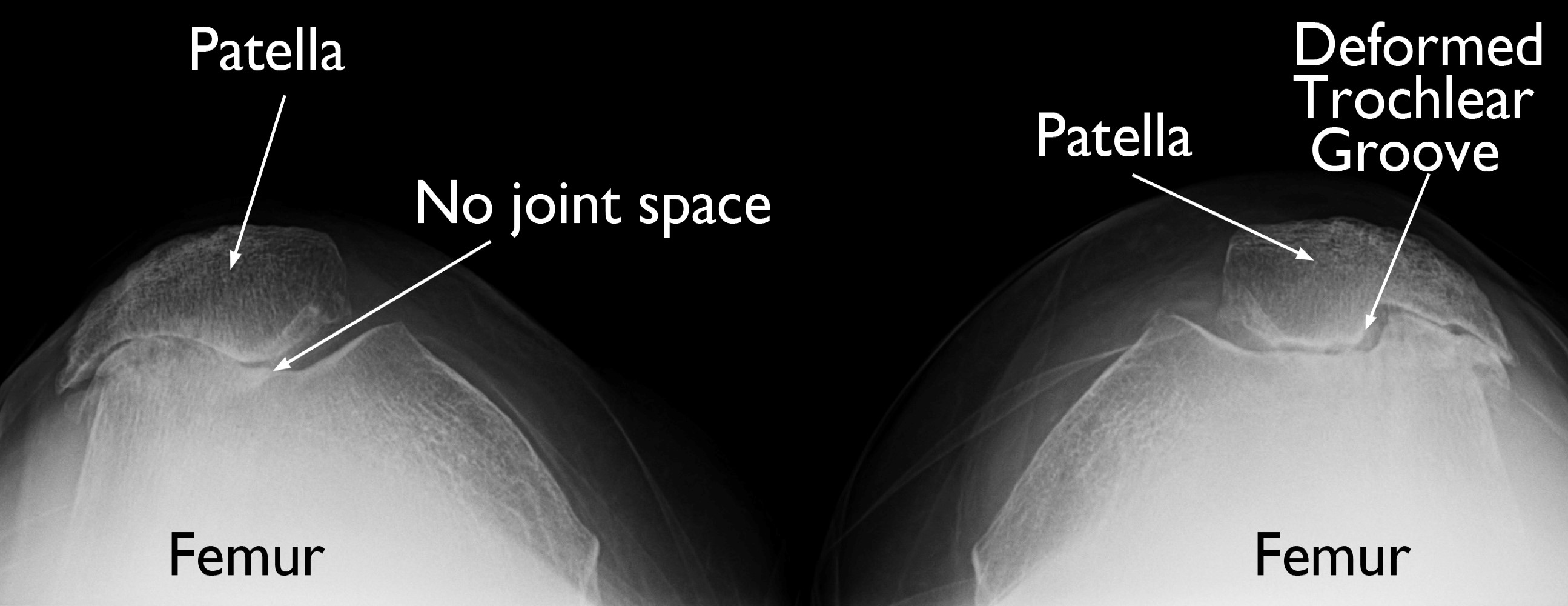
Patellofemoral arthritis affects the underside of the patella (kneecap) and the channel-like groove in the femur (thighbone) that the patella rests in. It causes pain in the front of your knee and can make it difficult to kneel, squat, and climb and descend (go down) stairs.
Anatomy
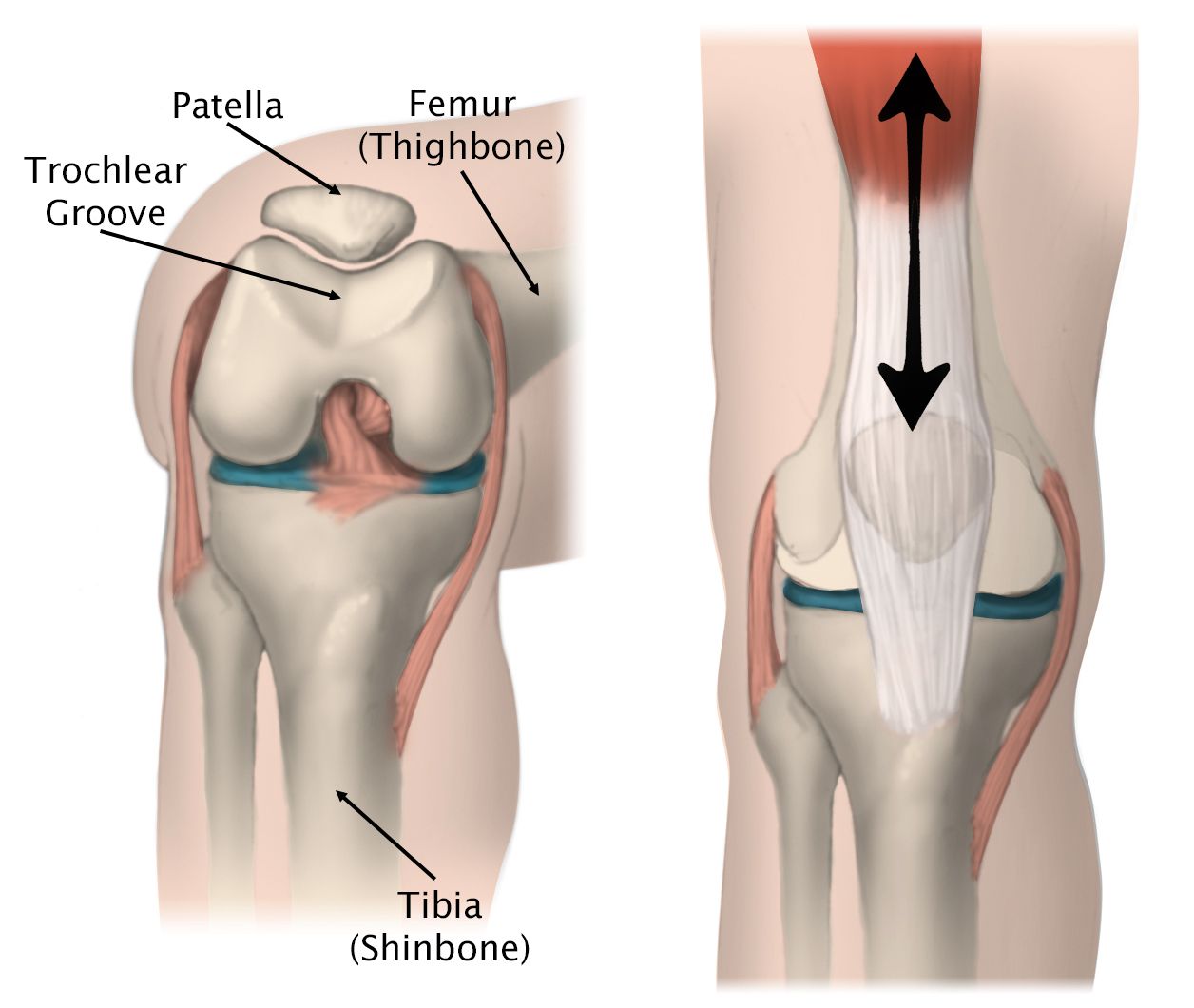
The patella is a small bone located in front of the knee joint — where the femur (thighbone) and tibia (shinbone) meet. It protects your knee and connects the muscles in the front of your thigh to your tibia.
The patella rests in a groove on top of the femur called the trochlear groove. When you bend and straighten your knee, the patella moves back and forth inside this groove.
A slippery substance called articular cartilage covers the ends of the femur, trochlear groove, and underside of the patella. Articular cartilage helps your bones glide smoothly against each other as you move your leg.
Description
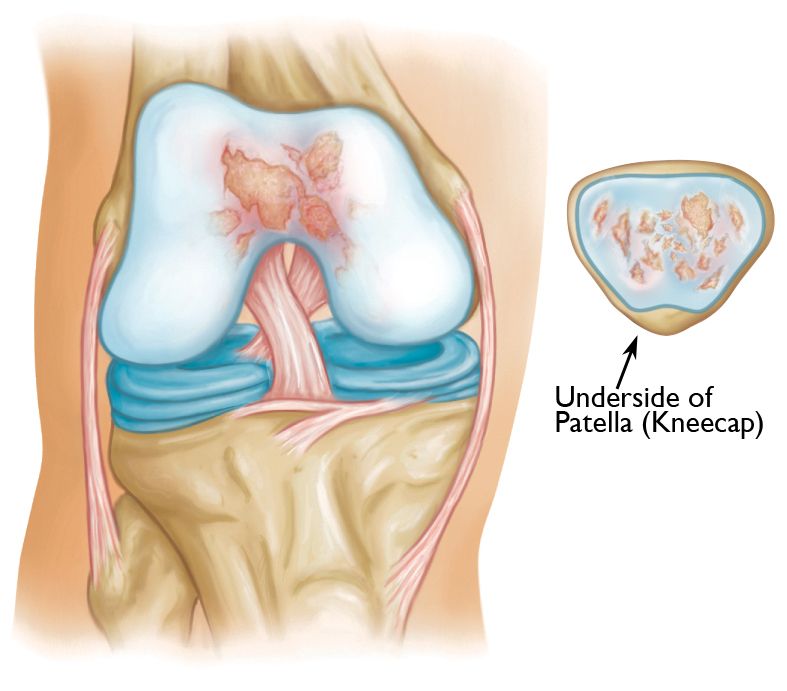
Patellofemoral arthritis occurs when the articular cartilage along the trochlear groove and on the underside of the patella wears down and becomes inflamed.
When cartilage wears away, it becomes frayed. When the wear is severe, the underlying bone may become exposed. Moving the bones along this rough surface may be painful.
Cause
Dysplasia
Dysplasia occurs when the patella does not fit properly in the trochlear groove of the femur. Because of this, when the knee moves, there are increased stresses on the cartilage. This begins to wear the cartilage down.
Kneecap Fracture
Patellar (kneecap) fractures often damage the articular cartilage that covers and protects the underside of the bone. Even though the broken bone heals, the joint surface may no longer be smooth. There is friction when the patella moves against the joint surface of the femur. Over time, this can lead to arthritis.
Symptoms
The main symptom of patellofemoral arthritis is pain. Typically, the pain is on the front of the knee, behind the kneecap (also known as anterior knee pain.
The pain can be present at rest or with no activity at all. Most of the time, however, it is brought on by activities that put pressure on the kneecap, such as:
- Going up and down stairs
- Sitting with the knees bent
- Rising from a chair
- Kneeling or squatting
In addition, you may experience a crackling sensation called crepitus when you move your knee. Crepitus is sometimes painful and can be loud enough for other people to hear.
When the disease is advanced, your kneecap may get stuck, or catch, when you straighten your knee.
Doctor Examination
When you visit the doctor, they will do a complete medical history and physical examination, as well as order imaging tests.
Medical History
Your doctor will ask you several questions about your general health, your knee pain, and your ability to function.
It is important for your doctor to determine the exact location of your pain so they can determine whether you have patellofemoral arthritis or another condition.
Physical Exam
Your doctor will examine the affected knee in various positions to see if there is pain or restricted motion. They will look for creaking or grinding noises (crepitus) that indicate bone-on-bone friction, muscle loss (atrophy), and signs of injury to muscles, tendons, and ligaments.
During the exam, the doctor will:
- Inspect your knee to determine the overall alignment of the joint
- Palpate (feel) around your knee to see if your pain can be reproduced
- Test range of motion to determine if you have knee stiffness or problems with patellar tracking (the kneecap moves out of place when the knee straightens or bends)
- Assess the quality of the ligaments around the joint and the overall stability of your knee
Imaging Tests
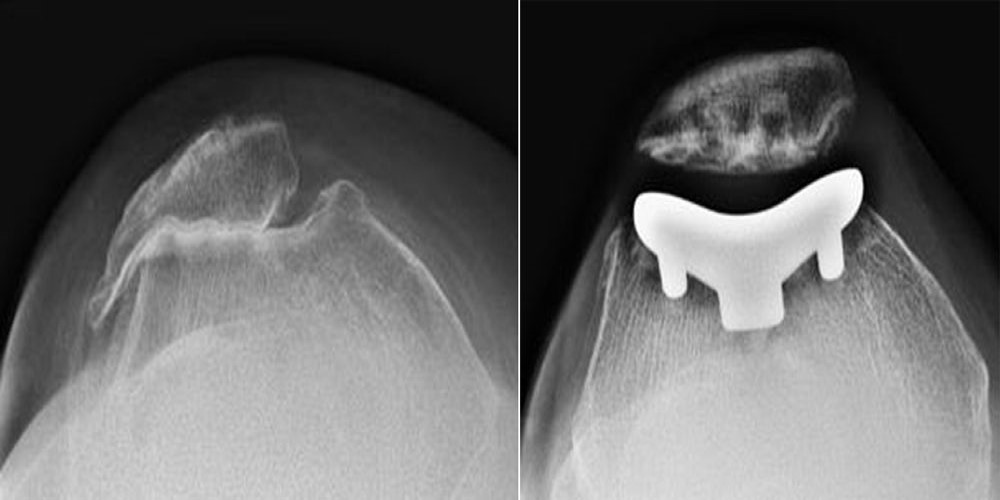
X-rays. X-rays provide images of dense structures, such as bone. Your doctor will order X-rays from several different angles to ensure that your arthritis is limited to the space between the kneecap and the femur, and to assess the overall alignment of your knee.
Magnetic resonance imaging (MRI) scans. MRI scans provide images of the soft tissues in your knee. Your doctor may order an MRI to better evaluate the cartilage in your knee.
Treatment
Nonsurgical Treatment
Treatment of patellofemoral arthritis is similar to the treatment of knee arthritis in general. Most cases can be treated without surgery. Nonsurgical options include:
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs like aspirin, naproxen, and ibuprofen reduce both pain and swelling.
Exercise. Regular exercise can decrease stiffness and strengthen the muscles that support your knee. Patients who have patellofemoral arthritis should try to avoid activities that put stress on the front of the knee, such as squatting. If you regularly do high-impact exercise, switching to low-impact activities will put less stress on your knee. Walking and swimming are good low-impact options.
Activity modification. In many cases, avoiding activities that bring on symptoms — such as climbing stairs — will help relieve pain.
Weight loss. If you are overweight, losing just a few pounds can make a big difference in the amount of stress you place on your knee. Losing weight can also make it easier to move and maintain independence.
Physical therapy. Specific exercises can improve range-of-motion in your knee and help with patellar tracking, including:
- Exercises to strengthen the quadriceps muscles and remove some of the load from the patella
- Stretching the external rotator muscles around the hip joint
If an exercise causes pain, stop the exercise and talk to your doctor or physical therapist.
Cortisone (steroid) injections. Cortisone is a strong anti-inflammatory medicine that can be injected directly into your knee.
Viscosupplementation. In this procedure, a substance is injected into the joint to improve the quality of the joint fluid. The effectiveness of viscosupplementation in treating arthritis is unclear and continues to be studied by researchers.
Surgical Treatment
Surgery is an option when nonsurgical treatment has failed. Several types of surgical procedures are available.
Chondroplasty. This procedure is done with arthroscopy — inserting thin surgical instruments into small incisions around your knee. During a chondroplasty, your surgeon trims and smooths roughened arthritic joint surfaces. Chondroplasty is an option in cases of mild to moderate cartilage wear.
Realignment. The soft tissues on either side of the kneecap are tightened or released to change the position of the kneecap in the trochlear groove.
Cartilage grafting. Normal healthy cartilage may be taken from another part of the knee or from a tissue bank to fill a hole in the articular cartilage. This procedure is typically considered only for younger patients who have small areas of cartilage damage.
Tibial tuberosity transfer. This procedure can help relieve pain in patients with arthritis in specific portions of the patella. The patellar tendon below the kneecap attaches to a bump on the front of the knee called the tibial tuberosity. Shifting the bump in any direction will change the position of the kneecap. After the procedure, the patella should move more smoothly in the trochlear groove, reducing pressure on the arthritic areas and relieving pain.
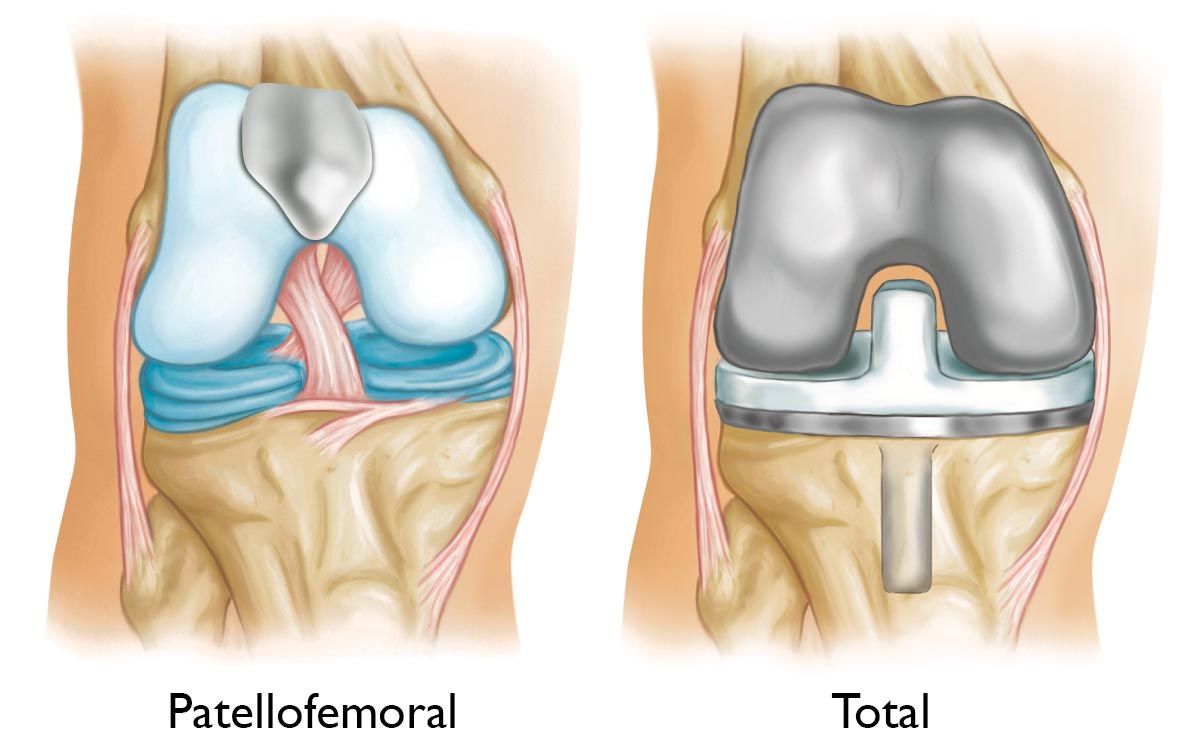
Patellofemoral replacement. During this partial knee replacement, the surgeon uses special tools to remove damaged cartilage and a small amount of bone from the patellofemoral compartment. A plastic button, or cover, is used to resurface the backside of the patella. This button will line up with a thin metal component that is used to resurface the trochlear groove at the end of the femur. These parts are typically secured to the bone with cement.
Patellofemoral replacement surgery cannot be performed if there is arthritis involving other parts of the knee. If this is the case, your doctor may recommend a total knee replacement.
Total knee replacement. In a total knee replacement, all the cartilage surfaces of the knee are resurfaced. The end of the femur and the top of the tibia are capped with a metal prosthesis. A plastic spacer is placed in between these components to create a smooth gliding surface. Additionally, the patella itself is usually resurfaced with a plastic button.
Outcomes
For most patients, treatment for patellofemoral arthritis is successful in relieving pain and improving function. Outcomes vary, however, depending on patient-specific factors and the type of treatment. Your doctor will talk with you about the expected outcome of treatment in your specific situation.
To help doctors in the nonsurgical management of osteoarthritis of the knee — the American Academy of Orthopaedic Surgeons has conducted research to provide some useful guidelines. These are recommendations only and may not apply to every case. For more information: Osteoarthritis of the Knee - Clinical Practice Guideline (CPG) | American Academy of Orthopaedic Surgeons (aaos.org)
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.