Diseases & Conditions
Patellar Tendon Tear
Tendons are strong cords of fibrous tissue that attach muscles to bones. The patellar tendon works with the muscles in the front of your thigh to straighten your leg.
Small tendon tears can make it difficult to walk and participate in other daily activities. A large tear of the patellar tendon is a disabling injury. It usually requires surgery and physical therapy afterward to regain full knee function.
Anatomy
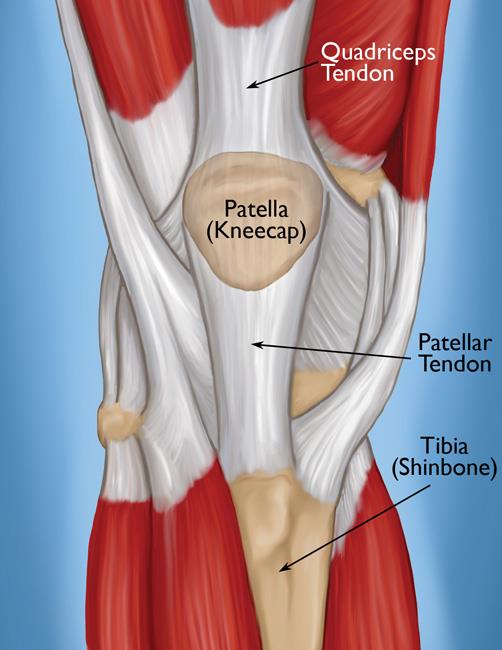
- The patellar tendon attaches the bottom of the patella (kneecap) to the top of the tibia (shinbone). When a structure connects one bone to another, it is actually a ligament, so the patellar tendon is sometimes called the patellar ligament.
- The patella is attached to the quadriceps muscles by the quadriceps tendon.
Working together, the quadriceps muscles, quadriceps tendon, and patellar tendon enable you to straighten your knee.
Description
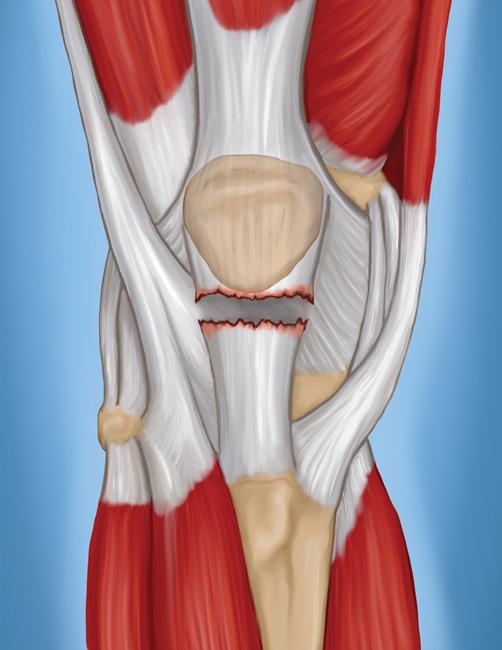
Patellar tendon tears can be either partial or complete.
- Partial tears. Many tears do not completely disrupt the tendon. This is similar to a rope that is stretched so far that some of the fibers are frayed, but the rope is still in one piece.
- Complete tears. When the patellar tendon is completely torn, the tendon is separated from the kneecap. Without this attachment, you cannot straighten your knee.
The patellar tendon often tears at the place where it attaches to the kneecap, and a piece of bone can break off along with the tendon. When a tear is caused by a medical condition — like tendinitis — the tear usually occurs in the middle of the tendon.
Cause
Injury
It takes a very strong force to tear the patellar tendon.
- Falls. Direct impact to the front of the knee from a fall or other blow is a common cause of tears. Deep lacerations are often associated with this type of injury.
- Jumping. The patellar tendon may tear when the knee is bent and the foot planted, like when landing from a jump or when jumping up.
Tendon Weakness
A weakened patellar tendon is more likely to tear. Several things can lead to tendon weakness.
Patellar tendinitis. Inflammation of the patellar tendon, called patellar tendinitis, weakens the tendon. It may also cause small tears.
Patellar tendinitis is most common in people who participate in activities that require running or jumping. Although it is more common in runners, it is often referred to as "jumper's knee."
Steroid use. Corticosteroid injections to treat patellar tendinitis have been linked to increased tendon weakness and increased likelihood of tendon rupture. Therefore, doctors typically avoid giving these injections in or around the patellar tendon. Oral corticosteroid and anabolic steroid use have also been linked to increased muscle and tendon weakness.
Chronic disease. Weakened tendons can also be caused by diseases that disrupt blood supply, including:
- Chronic kidney failure
- High cholesterol
- Inflammatory diseases (rheumatoid arthritis, systemic lupus erythematosus)
- Diabetes mellitus
- Infection
- Metabolic disease
Surgery
Previous surgery around the tendon, such as a total knee replacement or anterior cruciate ligament reconstruction, might put you at greater risk for a tear.
Symptoms
When a patellar tendon tears, you often experience a tearing or popping sensation. Pain and swelling typically follow, and you may not be able to straighten your knee. Additional symptoms include:
- An indentation at the bottom of your kneecap where the patellar tendon tore
- Bruising
- Tenderness
- Cramping
- Your kneecap moving up into the thigh because it is no longer anchored to your shinbone
- Difficulty walking due to the knee buckling or giving way
Doctor Examination
Medical History and Physical Examination
Your doctor will discuss your general health and the symptoms you are experiencing. They will also ask you about your medical history. These are some questions your doctor may ask you:
- Have you had a previous injury to the front of your knee?
- Do you have patellar tendinitis?
- Do you have any medical conditions that might make you more likely to experience a patellar tendon injury?
- Have you had surgery on your knee, such as a total knee replacement or an anterior cruciate ligament reconstruction?
After discussing your symptoms and medical history, your doctor will conduct a thorough examination of your knee. To pinpoint the cause of your symptoms, your doctor will test how well you can extend, or straighten, your knee. While this part of the examination can be painful, it is important for the doctor to determine whether you have a patellar tendon tear or a different injury so they can properly treat the injury.
Imaging Tests
To confirm the diagnosis, your doctor may order some imaging tests, such as an X-ray or magnetic resonance imaging (MRI) scan.
X-rays. The kneecap moves out of place when the patellar tendon tears. This is often very obvious on a side view X-ray of the knee. Complete tears can often be identified with these X-rays alone.
Magnetic resonance imaging (MRI) scan. An MRI creates images of soft tissues, like the patellar tendon. The MRI can show the amount of tendon torn and the location of the tear. Sometimes, an MRI is required to rule out a different injury that has similar symptoms.
Treatment
Your doctor will consider several things when planning your treatment, including:
- The type and size of your tear
- Your activity level
- Your age
Nonsurgical Treatment
Very small, partial tears respond well to nonsurgical treatment. Complete tears almost always are treated with surgery.
Immobilization. Your doctor may recommend you wear a knee immobilizer or brace, which locks into place to keep your knee straight and help it heal. You will most likely need crutches to help you avoid putting all of your weight on your leg. You can expect to be in a knee immobilizer or brace for 3 to 6 weeks.
Physical therapy. Once the initial pain and swelling have settled down, you can begin physical therapy. Specific exercises can restore your strength and range of motion.
While you are wearing the brace, your doctor may recommend exercises to strengthen your quadriceps muscles, such as straight-leg raises. As time goes on, your doctor or therapist will unlock your brace, which will allow you to move more freely with a greater range of motion. You will be prescribed more strengthening exercises as you heal.
Surgical Treatment
Most people with complete patellar tendon tears require surgery to regain knee function. Surgical repair involves reattaching the torn tendon to the kneecap.
People who require surgery do better if the repair is performed soon after the injury. Early repair may prevent the tendon from scarring and tightening into a shortened position.
Hospital Stay
Though tendon repairs are often done on an outpatient basis, some people do stay in the hospital at least 1 night after this operation. Whether you need to stay overnight will depend on your medical needs.
The surgery may be performed with either:
- Regional (spinal) anesthesia that numbs your lower body
- Regional anesthesia that numbs only your surgical leg
- General anesthesia, which puts you to sleep.
Procedure
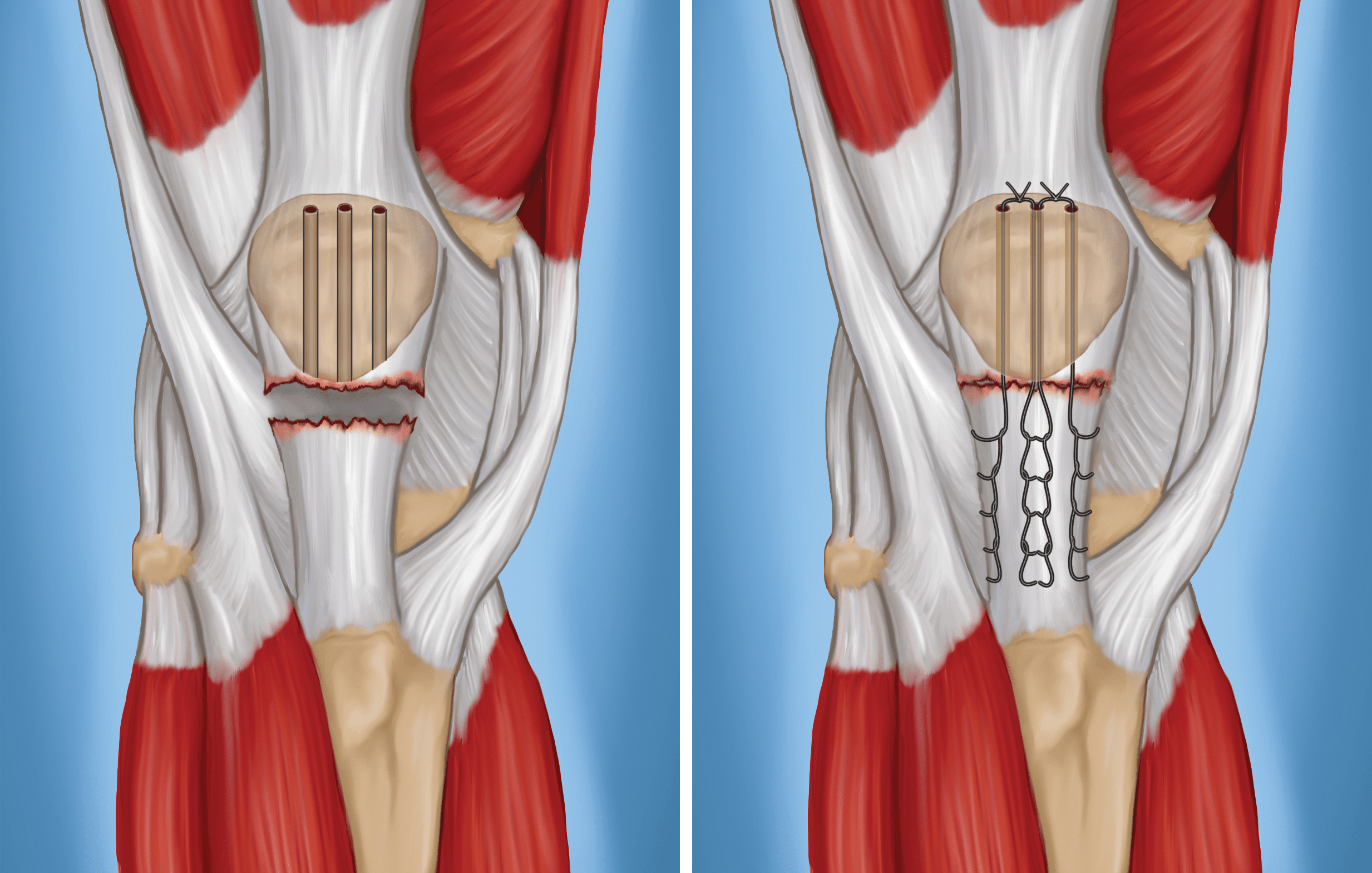
- To reattach the tendon, your surgeon places sutures in the tendon, then threads the sutures through drill holes from the bottom to the top of the kneecap.
- Your surgeon will carefully tie the sutures at the top of the kneecap to get the correct tension in the tendon. This will also ensure that the position of the kneecap closely matches that of your uninjured kneecap.
Alternate Technique
Another option in patellar tendon repair is the use of suture anchors. The surgeon attaches the tendon to the bone using small implants called suture anchors. Using these anchors means that the surgeon does not have to drill holes in the kneecap.
Considerations
To provide extra protection to the repair, some surgeons use a wire, sutures, or cables to help hold the kneecap in position while the tendon heals. If your surgeon does this, the wires or cables may need to be removed during a later, scheduled operation.
Your surgeon will discuss your need for this extra protection before your patellar tendon repair surgery. However, surgeons sometimes make this decision for additional protection during the operation, when they see that the tendon shows more damage than expected, or that the tear is more extensive.
If your tendon has shortened too much before surgery, it will be hard to re-attach it to your kneecap. Your surgeon may need to add tissue graft to lengthen the tendon. This sometimes involves using donated tissue (allograft).
Tendons often shorten if more than 1 month has passed since your injury. Severe damage from the injury or underlying disease can also make the tendon too short. Your surgeon will discuss this additional procedure with you before your surgery.
Complications
- The most common complications of patellar tendon repair include weakness and loss of motion.
- Re-tears sometimes occur, and the repaired tendon can detach from the kneecap.
- In addition, the position of your kneecap may be different after the procedure.
- As with any surgery, other possible complications include infection, wound breakdown, a blood clot, or complications from anesthesia.
After surgery you will require some type of pain management, including ice and medications. About 2 weeks after surgery, you will have your skin sutures or staples removed in your surgeon's office.
Surgical Recovery
Most likely, your repair will be protected with a knee immobilizer or, rarely, a long leg cast. You may be allowed to put your weight on your leg with the use of a brace and crutches (or a walker) with your leg in a straight position.
- To start, your surgeon may recommend "toe touch" weight bearing. This is when you lightly touch your toe to the floor, putting down just the weight of your leg.
- By 2 to 4 weeks, your leg can usually bear about 50% of your body weight.
- After 4 to 6 weeks, your leg should be able to handle your full body weight. In some cases, you can bear weight fully in extension earlier, but it depends on your individual tear, repair, and surgeon's recommendations.
- Over time, your doctor or physical therapist will unlock your brace. This will allow you to move more freely with a greater range of motion. Strengthening exercises will then be added to your rehabilitation plan.
In some cases, your doctor will prescribe an immediate motion protocol (treatment plan). This is a more aggressive approach and not appropriate for all patients. Most surgeons protect motion early on after surgery.
Your doctor and physical therapist will customize a rehabilitation plan for you. How long you need therapy and which exercises your treatment team prescribes will be based on:
- The type of tear you have
- Your surgical repair
- Your medical condition
- Your needs
Complete recovery takes about 6 months. Many patients report that they required 12 months before they reached all of their goals.
Outcomes
Most people are able to return to their previous occupations and activities after recovering from a patellar tendon tear. Many people report stiffness in the affected leg, but most regain range of motion nearly equal to that in the uninjured leg.
If you are an athlete, your surgeon will conduct a thorough assessment before giving you the go-ahead to return to your sport. Your surgeon will compare your leg strength using some functional knee testing (like hopping).
The goal is for your injured leg to be at least 85 to 90% as strong as your uninjured leg. In addition to leg strength, your surgeon will assess:
- Your leg's endurance
- Your balance
- Whether you have any swelling
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.