Diseases & Conditions
Osteosarcoma
Osteosarcoma is a rare cancer of the bone.
Cancer occurs when one type of cell grows out of control and, in some cases, spreads to other parts of the body. A sarcoma is a specific type of cancer that originates in bone (osteosarcoma), or muscle, fat, nerves, tendons, or blood vessels (soft tissue sarcoma). This article covers only osteosarcomas. Soft tissue sarcomas are covered in a separate article.
Osteosarcomas occur most frequently in the bones of growing kids between the ages of 10 and 30 years, though they can affect people of all ages. Although it is rare, with only about 1,000 cases diagnosed each year in the U.S., it is the most common childhood bone cancer.
Most osteosarcomas develop around the knee or the shoulder, though they can affect any bone. Most patients with osteosarcoma seek medical attention due to unrelenting (constant) pain, swelling, or abnormal growth of a bone.
It is important to find a team of doctors who are experts in treating osteosarcoma. This team usually involves an orthopaedic oncologist (a bone cancer surgeon), a medical oncologist (an expert in chemotherapy), and specialized radiologists, pathologists, physical therapists, psychologists, nurses, and advanced practice providers.
Osteosarcomas are usually treated with chemotherapy (medications to kill the cancer cells) and surgery to remove the cancer in the bone.
Description
Osteosarcoma is an aggressive bone cancer. This type of cancer occurs when a bone-forming cell starts growing out of control, making a malignant (cancerous) tumor in the bone. Cancers that start elsewhere in the body and then metastasize (spread) to bone are much more common than tumors that actually start in bone.
Although osteosarcoma is rare, it is the most common childhood bone cancer. Of the 1,000 new cases of osteosarcoma diagnosed each year in the U.S., about half are in children and teens.
Most osteosarcomas develop around the knee, shoulder, or hip of growing kids. Common locations include the femur (thigh bone), tibia (shin bone), or humerus (upper arm bone). However, osteosarcoma can also affect other parts of the body and can even arise outside of the bones in the soft tissues, especially in older patients.
In some cases, osteosarcoma can metastasize, or spread to other areas of the body. This means the cancer cells travel throughout the body and start growing in another location. When osteosarcomas metastasize, they most often spread to the lungs. Learn more: Metastatic Bone Disease
Cause
The cause of osteosarcoma is not known, but doctors have determined several factors that may make someone more likely to develop the disease.
Groups more commonly affected:
- Growing kids ages 10 to 30 years
- Older adults ages 60 to 80
- Males (osteosarcoma is more common in males than females)
Risk Factors
Factors that may increase your risk for developing osteosarcoma include:
- Previous treatment with radiation therapy
- Certain bone disorders. These include:
- Certain inherited (genetic) cancer syndromes. These include:
- Familial retinoblastoma
- Li-Fraumeni syndrome
- Bone infarct. In this condition, a disruption of the blood supply to a part of the bone leads to cell death.
Symptoms
- Pain is the most common symptom of osteosarcoma. This pain may come and go at first but, gradually, it becomes constant.
- Some people may have swelling or notice a growing lump or bump in the area where the tumor is growing.
- If the tumor is located in the leg, the patient may also develop a limp.
- Osteosarcoma weakens the bone and makes it more fragile than healthy bone. Sometimes people may break their bone due to the bone cancer. This is called a pathologic fracture.
Doctor Examination
Physical Examination
The doctor will:
- Talk with you about your or your child's general health and medical history
- Ask about your or your child's symptoms.
- Examine the painful area, looking for:
- Tenderness over the bone
- Swelling in the extremity (arm or leg)
- A firm, painful lump, tumor, or mass
- Limited range of motion in the nearby joint
Imaging and other tests are used to help diagnose osteosarcoma.
Imaging Tests
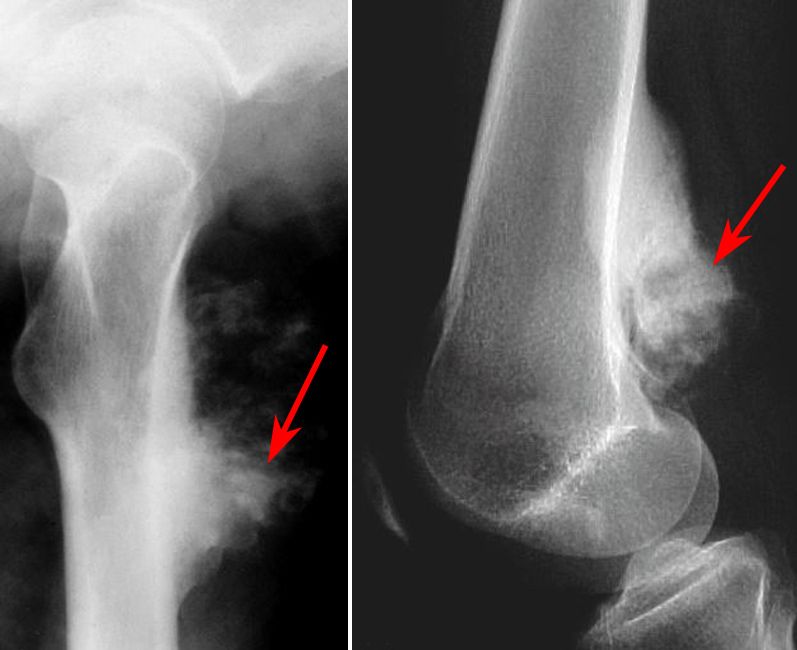
X-rays. X-rays provide images of dense structures, such as bone, and are very helpful in diagnosing osteosarcoma. Osteosarcoma can appear in different ways on an X-ray, but typical findings include:
- Formation of new bone in a "sunburst" pattern
- Onion-skinning — layering of the tissue on the outside of the bone
- Codman triangle — layering of the tissue on the surface of the bone and bony destruction
- A "cumulus cloud" appearance — a white, cloud-like lesion
While many osteosarcomas appear osteoblastic (meaning they make new bone) on X-ray, less common findings include lesions that appear osteolytic (meaning they break down bone), or mixed osteolytic/osteoblastic. Osteoblastic lesions appear white on X-ray, while osteolytic lesions appear dark/black.
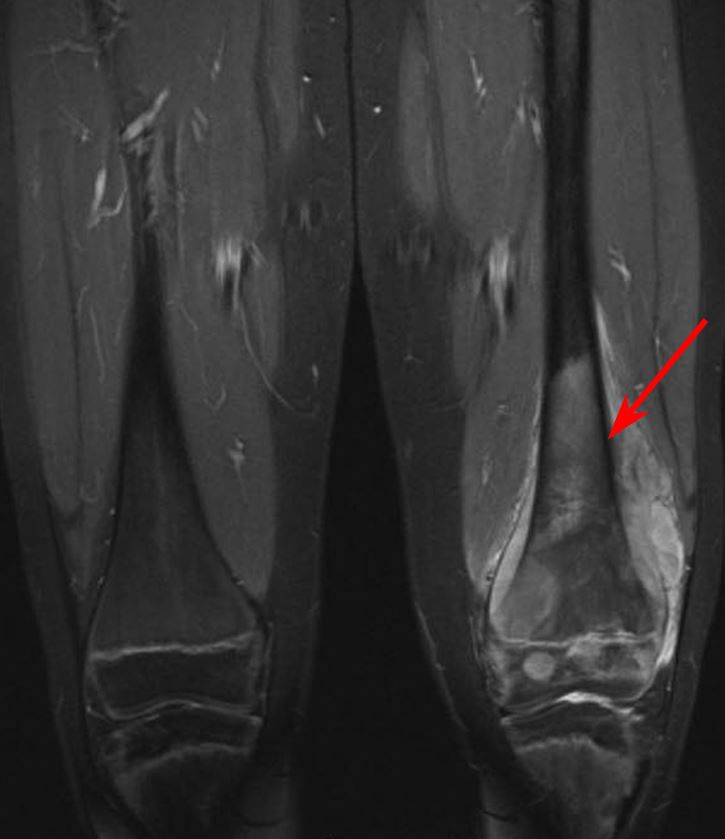
Magnetic resonance imaging (MRI) scans. MRI scans provide detailed views of bone marrow and other soft tissues. An MRI will help your doctor determine the extent (size) of the tumor and look for the spread of cancer to other parts of your or your child's body.
Computerized tomography (CT) scan. CT scans provide cross-sectional images that can help the doctors further evaluate the tumor. While MRI scans are generally considered more helpful than CT scans in diagnosing osteosarcomas, a CT scan may be helpful for planning future surgeries.
Tests
Laboratory tests. There are no blood tests that can make the diagnosis of osteosarcoma. The doctor may order lab tests to gather all information and help make a diagnosis, as well also get the patient ready for treatment.
Biopsy. A biopsy is needed to confirm the diagnosis of osteosarcoma. In a biopsy, a small sample of the tumor is removed and examined under a microscope. The procedure can be performed under local anesthesia (medicine is used to numb a specific area of the body) either with a needle or as a small operation using an incision. The biopsy may be performed by an orthopaedic surgeon or an interventional radiologist.
A pathologist will analyze the tissue sample to establish a diagnosis. Sometimes this process can take 7 to 10 days, as the pathologist may need to perform special tests on the tissue to get the answers.
Grading. The tumor will be graded during the biopsy. In general, the higher the grade, the more aggressive the tumor is suspected to be.
- Low-grade, or Grade 1 = (less aggressive). These tumors typically look more like normal cells than intermediate- or high-grade tumors.
- High-grade, or Grade 2 or 3 = (more aggressive). These tumors look almost nothing like the surrounding tissue and are often associated with a poorer outcome.
Staging. Once the tumor has been identified as osteosarcoma, the doctors will use imaging and other tests to determine whether the cancer has spread. This process is known as staging. Identifying the stage of the tumor will help the doctor determine the most effective treatment strategy.
The options for staging osteosarcoma include:
- Chest CT
- Whole body positron emission tomography (PET) CT
- Whole body bone scan
- Whole body PET MRI
Treatment
Treatment of osteosarcoma depends on many factors, including:
- The patient's age
- The patient's overall health
- The presence of other medical conditions
- The location of the tumor
- Whether the cancer has metastasized (spread)
- The specific subtype of osteosarcoma
When treating osteosarcoma, the team of doctors will work closely with the patient and their family to develop the best possible treatment plan.
Although treatment is individualized, many osteosarcomas are treated with a combination of chemotherapy and surgery.
Chemotherapy
Chemotherapy is the use of medications to treat cancer. Most chemotherapy is given to patients in the hospital through an IV. In patients with osteosarcoma, chemotherapy is given:
- Before surgery to help shrink the tumor and prevent the spread of the cancer
- After surgery to target any cancer cells that may remain and lower the risk that the cancer will return.
The most common drugs used for osteosarcoma include:
- Doxorubicin (DOX) or Adriamycin
- Methotrexate (MTX)
- Cisplatin (CDDP)
Most patients receive two or more of these drugs at once, which is known as combination chemotherapy.
- Chemotherapy is effective for high-grade osteosarcomas. Most patients complete about 10 weeks of chemotherapy before moving forward with surgery.
- Low-grade osteosarcomas usually do not need chemotherapy and are treated with surgery alone.
Preparing for Treatment
- A port, a special IV, will be placed under the skin just below the collarbone to help you or your child get chemotherapy.
- You or your child will have an ultrasound of the heart called an echocardiogram, or echo, to check your baseline function (how the heart is working) before chemotherapy.
- You or your child will have a hearing test to check baseline function before chemotherapy; hearing loss can be a side effect of chemotherapy, so it’s important for your doctors to be able to compare hearing before and after treatment.
Local Control Surgery
Effective treatment of osteosarcoma requires surgical removal of all of the cancer. Most of the time, orthopaedic oncologists (cancer surgeons) are able to perform limb salvage surgery. This means that the surgeon is able to remove the bone with cancer cells in it and then rebuild the limb with various techniques.
Sometimes, amputation is still required to remove all the cancer.
Limb Salvage Surgery and Reconstruction
- In limb salvage surgery, the doctor removes the tumor and a portion of the healthy tissue around it, while saving as much of the nearby tendons, nerves, and blood vessels as possible.
- The section of bone that is removed is replaced with either a bone graft (bone taken from a donor or from another part of the patient's own body) or a prosthesis made of metal and other materials. Sometimes, a bone graft and a prosthesis are used together.
Amputation
- There are many types of amputations. The level of amputation (how much of the limb is removed) is dictated by the tumor. Usually, a limb cannot be saved if the tumor is wrapped around major blood vessels.
- A unique amputation in sarcoma surgery is called a rotationplasty. This involved removing the segment (portion) of bone with the osteosarcoma and reconnecting the leg bones “rotated,” or backward, to allow the ankle to function as a knee in the prosthetic.
When the tumor is removed, it will be analyzed under a microscope to ensure complete removal and to determine the response of tissues to the preoperative chemotherapy.
- If it is determined that the tumor was not completely removed, another surgery may be needed to remove the rest of it.
- If tissue response to the preoperative chemotherapy was poor (meaning that not enough of the tumor cells were killed), the medical oncologist may recommend different chemotherapy drugs after surgery.
- If tissue response to the preoperative chemotherapy was good, the medical oncologist will usually recommend continuing the same chemotherapy regimen as before.
Radiation Therapy
Radiation therapy uses high-dose X-rays to kill cancer cells and shrink tumors. Although radiation therapy is not commonly used to treat osteosarcoma, it may be recommended for certain patients.
Recovery
Recovery after limb-salvage surgery requires extensive physical therapy, rehabilitation, and follow-up care. Patients need to be encouraged and supported by family and friends during this time. It can be challenging to participate in rehabilitation while still on chemotherapy due to reduced energy level and lack motivation to exercise.
The rehabilitation plan will vary based on the type of surgery that was performed. Most patients notice improvement in strength, function, and mobility for 1 to 2 years after surgery; after 2 years, there will not be much, if any, additional improvement.
Regular follow-up visits will be needed after treatment to check for complications from treatment and cancer recurrence or spread. These visits may include blood tests or imaging studies, such as X-rays or CT scans.
Surveillance
Regular follow-up visits will be needed after treatment for osteosarcoma.
- You or your child will need to have regular imaging and physical exams to make sure the cancer does not return or spread to other locations in your body.
- Your team will also closely monitor the outcomes of your treatments.
- Follow-up visits may include blood tests or imaging studies, such as X-rays, CT scans, and/or MRIs.
Outcome
The patient's prognosis after treatment will depend on many factors, including:
- Age
- Overall health
- The presence of other medical conditions
- The stage and grade of the tumor
- Whether the cancer has metastasized (spread to other locations)
- The specific subtype of osteosarcoma
- Response to chemotherapy
In most cases, how the tumor responds to preoperative chemotherapy is the best predictor of prognosis. At the time the tumor is removed, the doctor will examine it under a microscope to determine the amount of necrosis (how much of the tumor has died). In general, the higher the percentage of necrosis, the better the prognosis.
The goal of treatment for osteosarcoma is to cure the cancer. Treatment is successful for many patients with osteosarcoma. However, because each situation is unique, it is best to talk to the treatment team about the specific prognosis for you or your child.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.