Diseases & Conditions
Osteoporosis and Spinal Fractures
As we get older, our bones get thinner and our bone strength decreases. Osteoporosis is a condition in which bones are very weak and are more likely to break. It often develops slowly over time, and people often do not know they have osteoporosis until a bone breaks.
Fractures from osteoporosis most often happen in the spine. These spine fractures — called vertebral compression fractures — happen about 1.5 million times every year in the U.S. They are almost twice as common as other fractures linked to osteoporosis, like hip fractures and wrist fractures.
Not all spinal compression fractures are caused by osteoporosis. But when they are, the fracture is often the first sign that a person has weak bones. To learn more about osteoporosis: Osteoporosis.
Anatomy
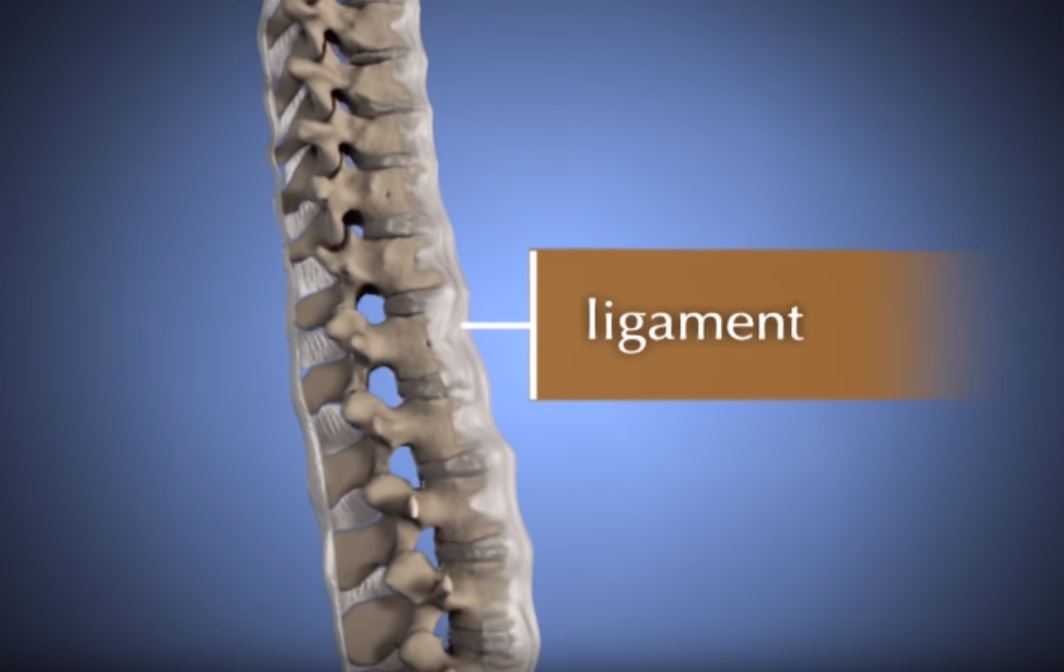
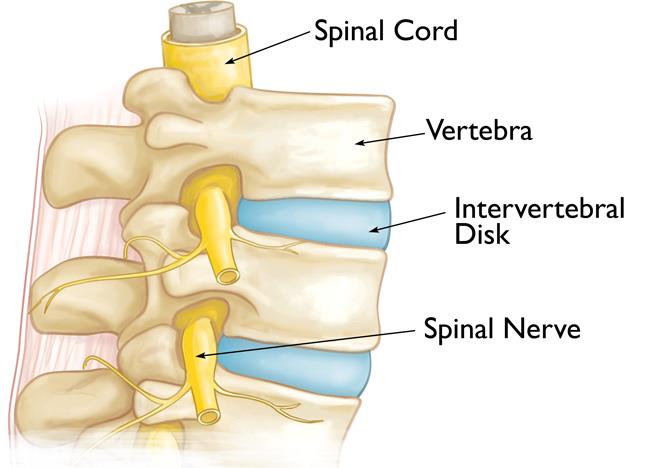
The spine has 24 bones called vertebrae stacked on top of each other. These bones create a tunnel that protects the spinal cord. Other parts of your spine include:
Spinal cord and nerves. These work like electrical wires, running through the spinal canal and carrying messages between your brain and muscles. Nerve roots leave the spinal cord through openings in the vertebrae.
Intervertebral disks. These soft, round disks sit between your vertebrae. They are about 1/2-inch thick. They act like cushions, absorbing shock when you walk or run.
Cause
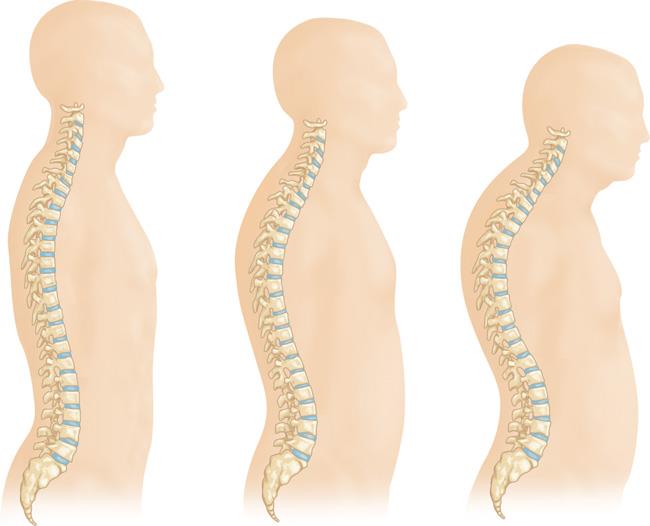
Osteoporosis is a common part of getting older. As we get older, our bones get weaker. When the vertebrae in the spine weaken, they can shrink and flatten. This can make older adults shorter and give them a curved back or a hunched appearance.
Weakened vertebrae are more likely to break. A vertebral compression fracture happens when too much pressure is placed on a weak bone and the front of it cracks and becomes shorter, losing its original height.
These fractures often happen after a fall. But people with osteoporosis can break a bone even when during seemingly innocent activities like reaching, twisting, coughing, or sneezing.
Symptoms
A vertebral compression fracture causes back pain, usually in the spot where the bone is broken. These fractures most often occur near the waistline but can also happen above or below it in the middle or lower back.
- The pain often gets worse when you move, especially when changing positions. Resting or lying down often helps.
- Coughing and sneezing can make the pain worse.
- The pain might spread to other places, like the stomach or legs, but this does not happen often.
- If the fracture is serious, it can press on nerves and cause pain or other symptoms that involve the legs.
Doctor Examination
Physical Examination
Your doctor will ask you about your health and will do a physical exam.
- While you are standing, the doctor will check your spine and posture.
- The doctor will press on certain parts of your back to find out if the source of the pain is your muscle or bones.
- To check your nerves, your doctor will do a neurological exam. They will look for numbness, reflex changes, or weak muscles.
Imaging Tests
Imaging helps the doctor learn more about your fracture and see if it is acute (new) or chronic (older).
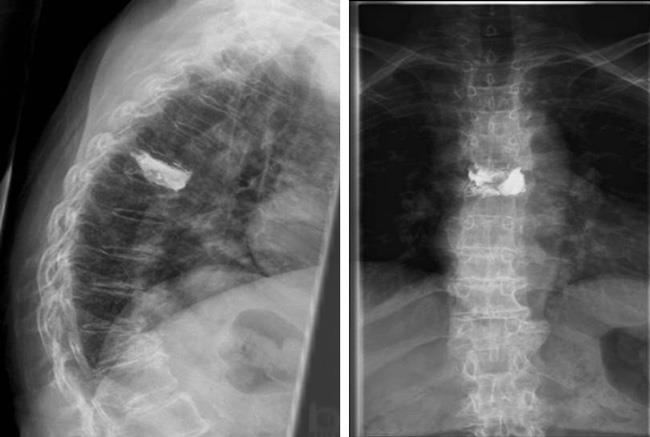
X-rays. X-rays provide images of the bones in the spine (vertebrae). If your doctor thinks you have a spinal fracture, they will order an X-ray to find out.
X-rays may reveal other spine problems. Older adults with a spinal fracture may also have smaller disk spaces (degenerative disk disease) or scoliosis, a sideways curve of the spine.
Magnetic resonance imaging (MRI) scan. An MRI shows soft tissues like nerves and intervertebral disks. It can help tell if the fracture is new. A new fracture will look brighter on the scan, which shows edema (swelling) in the bone. An old fracture will look normal on an MRI.
Bone scan. A bone scan can show abnormal activity, including fractures, in bones. It may also help to show if the fracture is new or old.
Computed tomography (CT) scan. A CT scan shows both soft tissues and bones. It helps the doctor see if the fracture has spread into the spinal canal, where the spinal cord and nerve roots are.
Bone Density Testing
When you have a spinal fracture, your doctor may check to see if you have osteoporosis and, if so, how serious it is. X-rays can often show thin bones in the spine. This condition is called low bone mass (also known as osteopenia). Low bone mass can lead to osteoporosis.
A scan called dual-energy X-ray absorptiometry (DEXA) measures how strong your bones are. DEXA results help the doctor predict your risk for more fractures in the spine or other bones. The results also help the doctor decide if you need medicine to treat bone loss.
It is important to consider treatment for osteoporosis. Studies have shown that more than 30% of people with a spinal fracture will suffer another fracture within 1 year.
Treatment
Nonsurgical Treatment
Most people with a spinal compression fracture feel better within 3 months without surgery.
- Rest and a small amount of pain medication are often enough.
- Sometimes, patients wear a back brace to help the fracture heal.
When the fracture heals, the bone does not return to its normal shape. But once it heals, it usually does not collapse again.
If your doctor finds that you have osteoporosis, you are more likely to have more spinal fractures or fractures in the hip or wrist. Your doctor may discuss options to help prevent these. Learn more: Osteoporosis Prevention and Treatment
Surgical Treatment
If your pain is severe and does not improve, surgery may be an option.
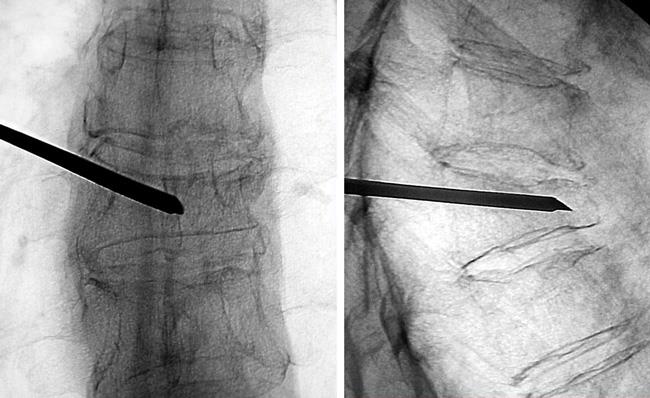
In the past, surgery for spinal fractures was very invasive. Now, there are less invasive surgeries called vertebral augmentation procedures.
There are two types: kyphoplasty and vertebroplasty. These are best for people with severe pain from a recent fracture.
Your doctor will help you choose which one is best based on your fracture.
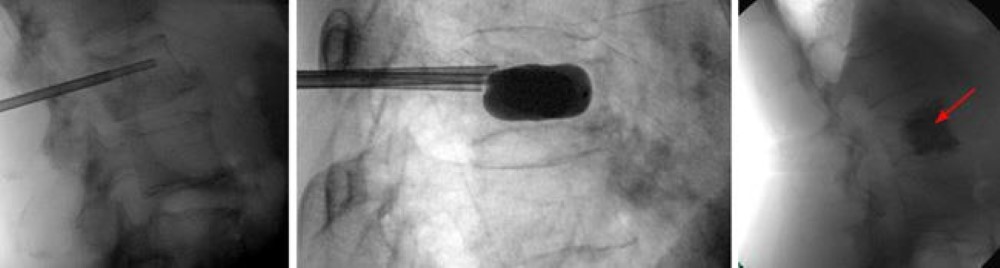
Kyphoplasty. In a kyphoplasty:
- A needle is placed in the broken vertebra using X-ray images to guide it.
- A small balloon is inserted through the needle into the bone.
- The balloon is inflated to make the bone taller and more round again.
- After the balloon is removed, the empty space is filled with special bone cement to make the bone strong.
Kyphoplasty can be done with general anesthesia (you are asleep) or local anesthesia (you are awake, but your body is numb). During the procedure, you lie face down and the doctor works from the back.
After surgery, patients can return to all normal activities as soon as they feel able.
Vertebroplasty. Vertebroplasty is like kyphoplasty, but it does not use a balloon. Instead, cement is injected straight into the broken vertebra. As with kyphoplasty, the patient lies face down while the surgeon works from the back of the spine.
After surgery, patients are encouraged to return to normal daily activities quickly.
Talk to your surgeon about whether a procedure is appropriate for you and, if so, which procedure is best for you.
Surgical Outcomes
Many studies have looked at how well vertebral augmentation surgeries work.
- Two large studies shows that vertebroplasty only helps in the short term.
- In contrast, current studies have shown that kyphoplasty may help people feel better sooner and move more easily than if they only have nonsurgical treatment.
If surgery is recommended for you, your doctor will explain what you can expect in terms of recovery and pain relief.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.