Diseases & Conditions
Osteoarthritis of the Elbow
This article was written and/or reviewed by a member of American Shoulder and Elbow Surgeons (ASES).
Osteoarthritis of the elbow occurs when the cartilage surface of the elbow is worn out or damaged. This can happen because of a previous injury such as an elbow dislocation or fracture. Most commonly, however, it is the result of a normal wearing away of the joint cartilage as we age and from years of activity.
Osteoarthritis usually affects the weightbearing joints, such as the hip and knee. The elbow is one of the least affected joints because of its well-matched joint surfaces and strong stabilizing ligaments. As a result, the elbow joint can tolerate large forces across it without becoming unstable.
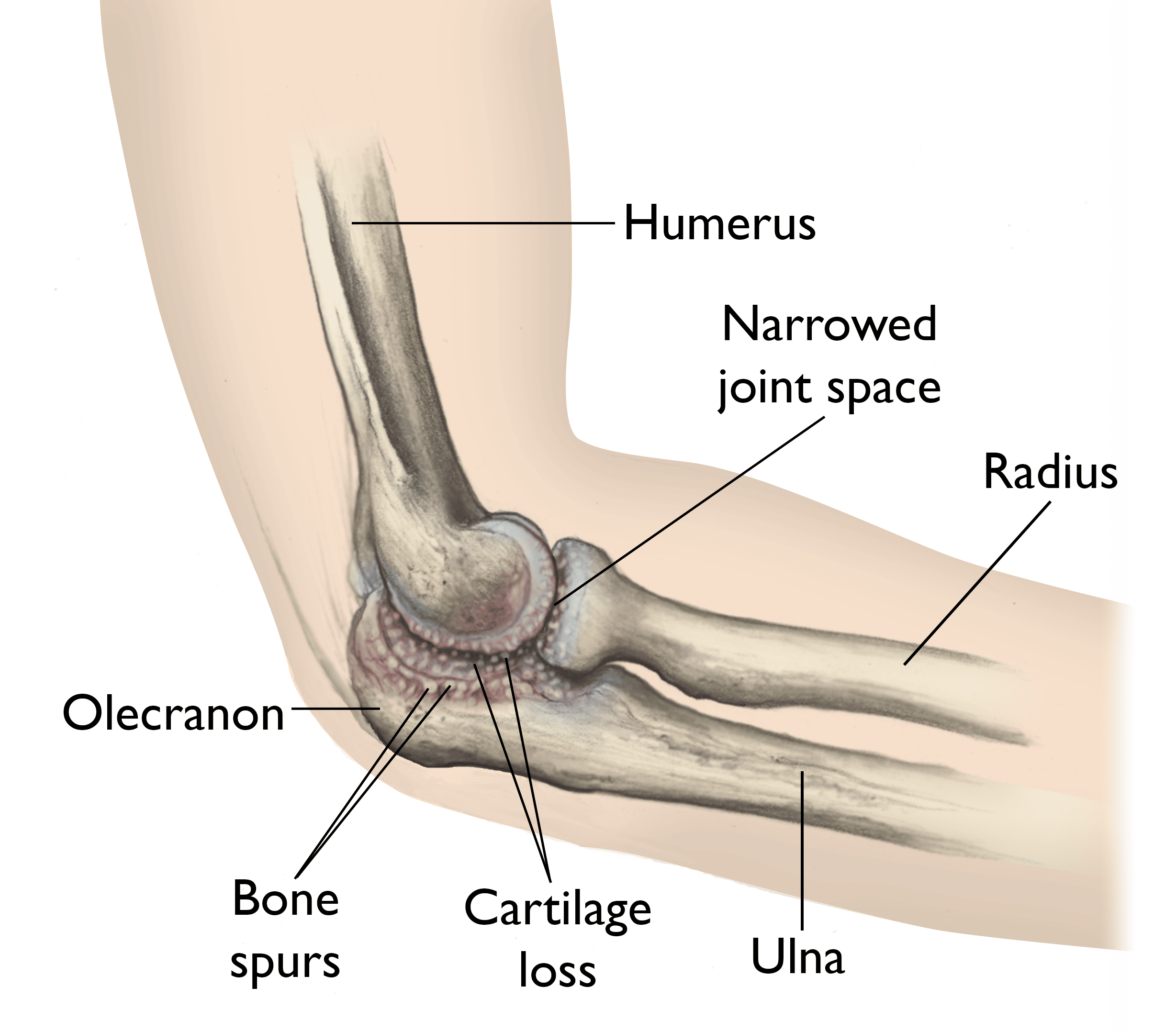
Anatomy
The elbow is a hinge joint which is made up of three bones:
- The humerus (upper arm bone)
- The ulna (forearm bone on the pinky finger side)
- The radius (forearm bone on the thumb side)
The surfaces of the bones where they meet to form the elbow joint are covered with articular cartilage, a smooth substance that protects the bones and enables them to move easily.
A thin, smooth tissue called synovial membrane covers all remaining surfaces inside the elbow joint. In a healthy elbow, this membrane makes a small amount of fluid that lubricates the cartilage and eliminates almost any friction as you bend and rotate your arm.
Muscles, ligaments, and tendons hold the elbow joint together.
Description
Osteoarthritis is an age-related, wear-and-tear type of arthritis. It usually occurs in people age 50 and older but may occur in younger people, too. The cartilage that cushions the bones of the elbow softens and wears away. The bones then rub against one another. Over time, the elbow joint becomes stiff and painful.
Cause
Some people who are diagnosed with elbow osteoarthritis have a history of injury to the elbow, such as a fracture that involved the surface of the joint, or an elbow dislocation. The risk for elbow arthritis increases if:
- You needed surgery to repair the injury or reconstruct the joint
- There is loss of joint cartilage
- The joint surface cannot be repaired or reconstructed to its preinjury level
Injury to the ligaments resulting in an unstable elbow can also lead to osteoarthritis, even if the elbow surface is not damaged, because the normal forces across the elbow are altered, causing the joint to wear out more rapidly.
In some cases, no single injury to the elbow occurs. Work or heavy activities can lead to osteoarthritis of the elbow if a person places more demands on the joint than it can bear.
For example, professional baseball pitchers place unusually high demands on their throwing elbows, which can lead to failure of the stabilizing ligaments. When this occurs, surgical reconstruction may be needed. High-shear forces placed across the joint can lead to cartilage breakdown over a period of years.
The best way to prevent elbow arthritis is to avoid injury to the joint. If you do suffer an injury, it is important to recognize it right away and get treatment. Individuals involved in heavy work or sports activities should maintain muscular strength around the elbow, and always condition properly and use correct technique.
Symptoms
The most common symptoms of elbow arthritis are:
- Pain
- Loss of range of motion
These symptoms may not occur at the same time. Patients usually report a grating or locking sensation in the elbow.
- The grating is due to loss of the normal smooth joint surface. This is caused by cartilage damage or wear.
- The locking is caused by loose pieces of cartilage or bone that dislodge from the joint and become trapped between the moving joint surfaces, blocking motion.
Joint swelling may also occur, but this does not usually happen at first. Swelling occurs later, as the disease progresses.
In the later stages of osteoarthritis of the elbow, patients may notice numbness in their ring finger and small (pinky) finger. This can be caused by elbow swelling or limited range of motion in the joint.
- The ulnar nerve (funny bone) is located in a tunnel behind the inner (medial) side of the elbow. Swelling in the elbow joint can put increased pressure on the nerve, causing tingling.
- If the elbow cannot be moved through its normal range of motion, it may stiffen into a position where it is bent (flexion). This can also cause pressure around the ulnar nerve to increase.
Doctor Examination
A doctor can usually diagnose osteoarthritis of the elbow based on symptoms and standard X-rays. X-rays show the arthritic changes. Advanced diagnostic imaging, such as a computed tomography (CT) scan or magnetic resonance imaging (MRI) scan, is typically not needed to diagnose osteoarthritis of the elbow.
Elbow osteoarthritis that occurs without previous injury is more common in men than women. Onset typically occurs in people 40 to 50 years of age or older, but some patients will experience symptoms earlier.
Treatment
Treatment options depend on:
- The stage of the disease
- Prior history of injury to the elbow
- The patient's desires
- The patient's overall medical condition
- The results of X-rays and other tests
Nonsurgical Treatment
For the early stages of osteoarthritis of the elbow, the most common treatment is nonsurgical. This includes:
- Oral medications to reduce or alleviate pain.
- Physical therapy.
- Activity modification.
- Corticosteroid injections. These injections, which are sometimes used to treat osteoarthritis symptoms, work in most but not all patients with elbow osteoarthritis. Although the effects of injections are temporary, they can provide some pain relief until symptoms progress enough to need additional treatment.
Surgical Treatment
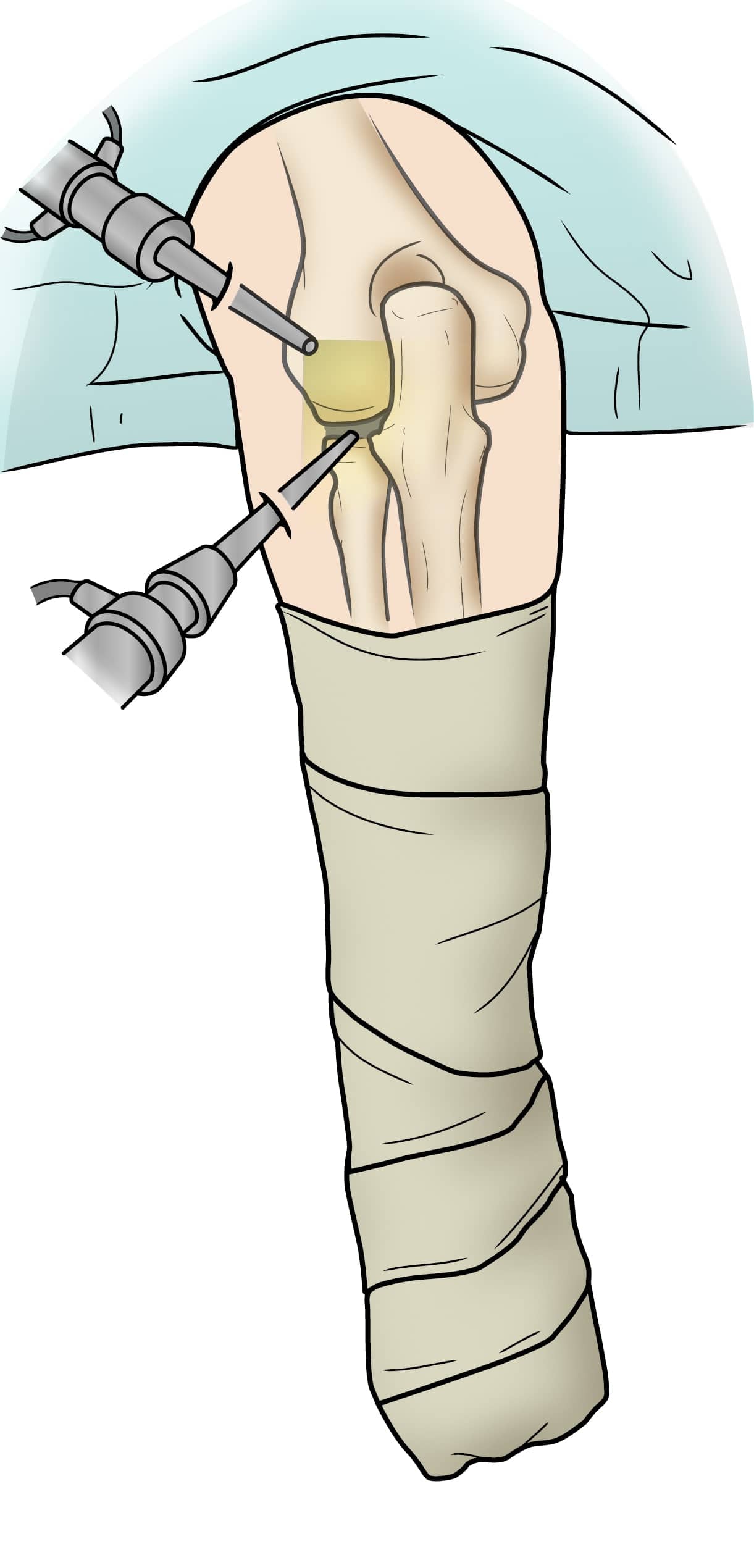
When nonsurgical interventions are not enough to control symptoms, surgery may be helpful. By the time arthritis can be seen on X-rays, there has been significant wear or damage to the joint surfaces. Even if the wear and bone spurs are severe, arthroscopy, a minimally invasive surgical treatment, can improve motion and decrease pain.
Arthroscopy, which can be done as an outpatient procedure, has been shown to improve symptoms and range of motion. the surgeon uses multiple small incisions to perform the surgery, which involves removing any loose bone/cartilage fragments or inflammatory/degenerative tissue in the joint; smoothing out irregular surfaces; and/or removing bone spurs. Because arthroscopy does not require large incisions, recovery is reasonably quick.
If the joint surface has worn away completely, it is unlikely that anything other than a joint replacement would bring about relief. There are several different types of elbow joint replacement available.
In appropriately selected patients, the improvement in pain and function after a joint replacement can be dramatic. However, there are long-term functional limits — usually, you cannot lift more than 5 to 10 pounds with the treated arm — so the decision to have a total elbow replacement should be made carefully.
For patients who are too young or too active to have a joint replacement, there are other reasonably good surgical options. If loss of motion is the primary symptom, the surgeon can release the stiffness and smooth out the joint surface. At times, a new surface made from the patient's own body tissues can be made. These procedures can provide some improvements in symptoms and function.
Research on the Horizon
In patients with loss or damage to specific areas of the elbow joint, a cartilage/bone graft can be considered. The goal of this procedure is to return the joint to its prior smooth appearance and form to try to prevent further deterioration. As the understanding of cartilage growth and regeneration improves, this may allow replacement of larger areas of joint damage or degeneration.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.