Diseases & Conditions
Morton's Neuroma
If you sometimes feel that you are "walking on a marble," and you have persistent pain in the ball of your foot (forefoot), you may have a condition called Morton's neuroma.
Also known as an interdigital neuroma, a Morton's neuroma is a benign (non-cancerous) tumor of a nerve. Morton's neuroma is not actually a tumor, but a thickening of the tissue that surrounds the digital nerve leading to the toes. This thickening can lead to various levels of pain or discomfort in the forefoot that may limit your ability to perform certain activities.
Anatomy
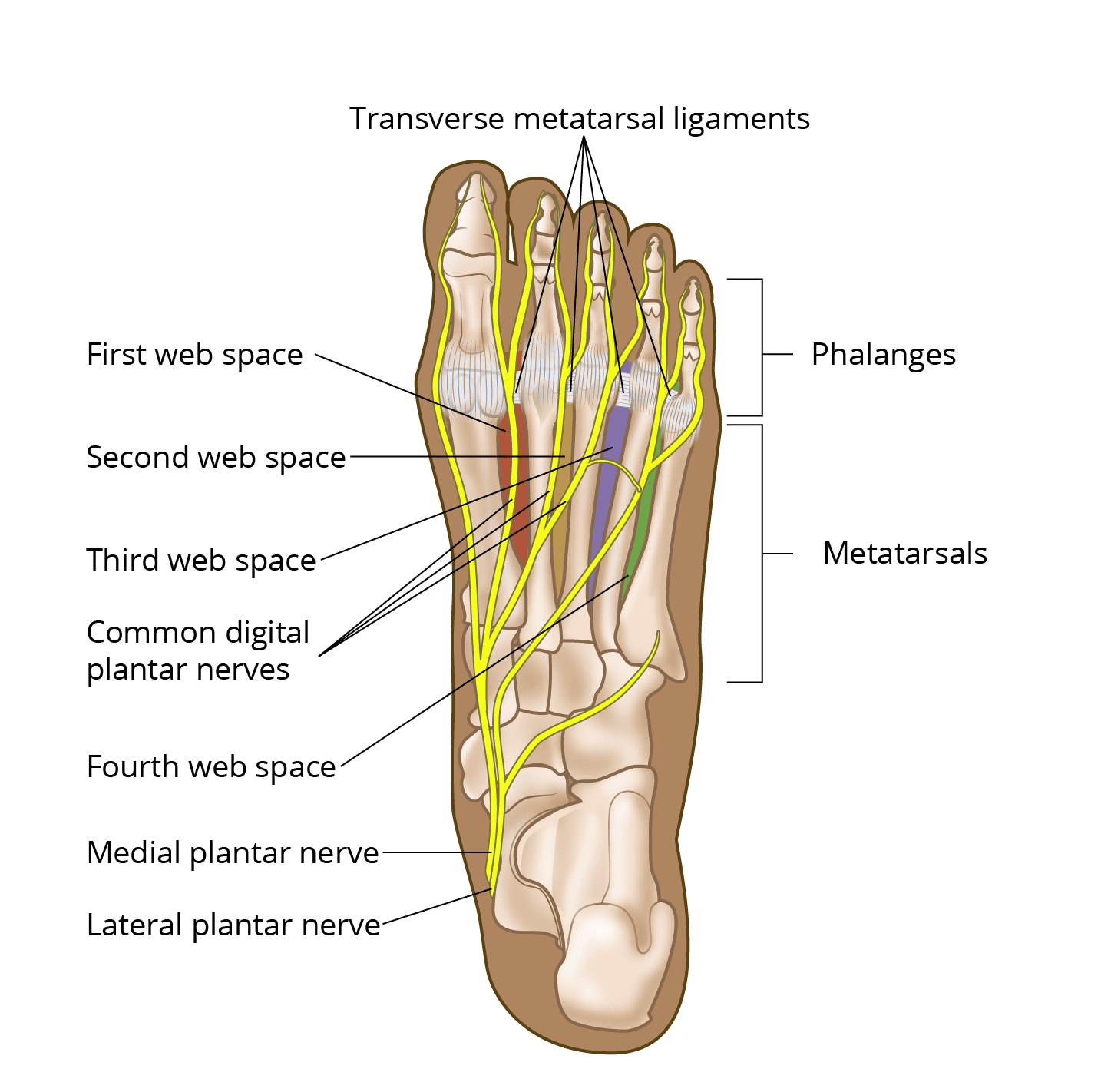
- The forefoot (front part of the foot) has 14 phalanges (toe bones) and five metatarsals (bones that connect the forefoot to the midfoot).
- The areas between the bases of the metatarsals, known as web spaces, are part of the forefoot. There are four web spaces:
- The first web space is located between the big toe and second toe.
- The second web space is located between the second and third toes.
- The third web space is located between the third and fourth toes.
- The fourth web space is located between the fourth and fifth (little) toes.
- The nerves that give sensation to part of your toes are called the medial and lateral plantar nerves. These nerves travel along the bottom of your foot and branch out as they near the toes.
- The nerve branches in the forefoot at the level of the web space are called common digital plantar nerves.
- In the web space, the rounded ends of the metatarsal bones are connected to each other by ligaments called transverse metatarsal ligaments. The common digital plantar nerves on the bottom of your foot pass underneath these ligaments in the web space.
Description
This condition is frequently referred to as a Morton's neuroma, though your physician or other sources may also refer to this condition as an interdigital neuroma, Morton metatarsalgia, interdigital neuritis, or a plantar neuroma.
Morton's neuromas are around 8 times more common in women than men and typically affect people between the ages of 30 and 60, though they can occur outside of this age range as well.
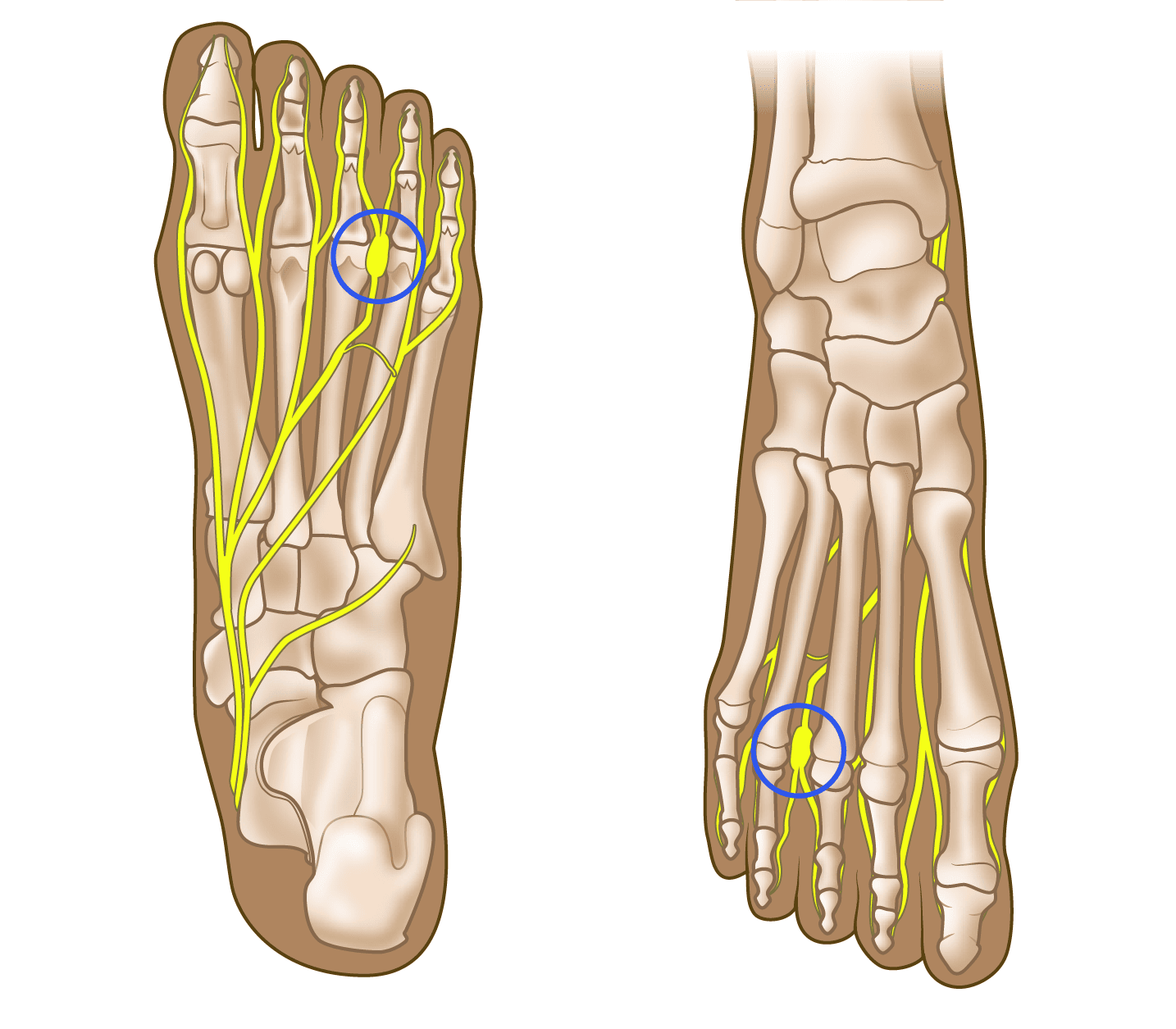
- Morton's neuroma most frequently develops in the area between the third and fourth toes — the third web space — usually in response to irritation, trauma, or excessive pressure.
- A Morton's neuroma can also develop in the second web space (the area between the base of the second and third toes), though this happens less often.
The most common symptom is pain or discomfort in the ball of the foot (the area between the arches and toes on the bottom of the foot).
Cause
The exact cause of a Morton's neuroma is not known, but current research suggests it is likely the result of entrapment (i.e., compression or squeezing) of the common digital plantar nerves. Compression of the nerve in the web space may trigger swelling and cause abnormal tissue to form in and around the nerve.
Symptoms
Normally, there are no outward signs of a Morton's neuroma, such as a lump or skin discoloration.
These are the most common symptoms:
- Persistent burning or sharp pain in the ball of the foot may radiate (spread out) into the toes, especially during weightbearing activities like running or walking. Night pain is rare.
- Patients frequently describe the sensation of having a pebble or marble under their forefoot as they walk.
- Pain is typically between the base of the third and fourth toes, but it can occur between the second and third toes as well.
- There may be numbness or an unpleasant tingling in the toes.
- Sprinters may feel pain as they push off from the starting block.
- Problems with shoe wear are common.
- High-heeled shoes, which put the foot in a similar position to the sprinter’s push-off, can aggravate the condition.
- Tight, narrow shoes also aggravate this condition by compressing the toe bones and pinching the nerve.
You should seek evaluation from an orthopaedic surgeon if you have continued pain or discomfort in your forefoot.
Doctor Evaluation
Your doctor will talk with you about your general health and medical history, and ask questions about the location, nature, severity, and duration of your symptoms. It is important to also discuss specific activities you have noticed that bring on the pain, as well as things that provide relief (e.g., rest, changing shoes).
Your doctor will then perform a physical exam, including:
- Evaluating the skin of the foot and ankle for signs of excessive pressure points (areas that are painful to the touch).
- Checking the position of the toes and foot for common deformities that may also cause pain in the forefoot.
- Putting pressure on the spaces between the toes to try to pinpoint the specific site of the pain.
- Assessing range of motion of the toe joints, as well as other joints, to see if there is irritation that may suggest arthritis or joint inflammation as a cause of the pain.
- Possibly squeezing your foot to check for a click between your toes — called a "Mulder’s click" — that is sometimes present with a Morton's neuroma.
X-rays may be required to rule out a stress fracture or arthritis of the joints that join the toes to the foot. Advanced imaging, such as an MRI, may be necessary in certain cases, but this is often not needed.
Nonsurgical Treatment
Initial management of a Morton’s neuroma typically involves one or more of the following:
- Changes in footwear. Avoid high heels and tight, narrow shoes; choose wider shoes (i.e., a wide toe box) with lower heels and a soft sole. This enables the bones to spread out and may reduce pressure on the nerve, giving it time to heal.
- Orthoses. Custom shoe inserts and metatarsal pads/bars can be added to your shoes. These may help relieve irritation by changing the location of forces on the forefoot and separating the bones, which reduces the pressure on the neuroma.
- Injection. One or more injections of a corticosteroid (steroid) medication can reduce the swelling and inflammation of the nerve, bringing some relief. This may be done in the orthopaedic clinic, or you may be referred to an ultrasound specialist who will perform the injection under guidance. Another type of injection is nerve ablation, which involves injecting a medication that permanently stops the nerve from sending out pain signals.
- Alternative therapies. Treatments such as extracorporeal shockwave therapy, radiofrequency ablation, and other non-steroid injections may be discussed, but current data on the effectiveness of these treatments is inconclusive.
Studies have shown that many people can achieve lasting relief with a combination of shoe wear modifications, orthoses, anti-inflammatory medications (e.g., ibuprofen or naproxen), and/or corticosteroid injections.
Surgical Treatment
If your symptoms do not improve, or if they come back after nonsurgical treatment, your surgeon may recommend surgery to either:
- Remove the diseased portion of the nerve, or
- Release tissue around the nerve
Surgery is often considered to be the most reliable form of treatment for a Morton's neuroma, with many studies showing an 80 to 95% success rate.
There are several surgical techniques to treat Morton's neuromas, and they have been shown to produce similar results. Your orthopaedic surgeon will discuss your options with you.
To access the nerve, the surgeon can make an incision on either the top or bottom of the foot over the web space. After accessing the nerve, your surgeon may remove the swollen portion of the nerve or release tissues around the nerve to decompress it. Which approach your surgeon uses depends on many factors, and you should discuss the specifics of the procedure with your surgeon.
The recovery period after surgery for Morton's neuroma is short. Protocols differ, and you should follow the specific instructions of your operating surgeon.
- In general, you will be allowed to walk on your foot in a stiff-soled shoe, also known as a post-op shoe, though you may be asked to put all your weight on your heel if an incision was made on the bottom of your foot.
- You should avoid heavier activities (running, jumping, etc.) and putting your foot underwater (such as in a bathtub or swimming pool) until your surgical wounds are completely healed — usually until at least 2 to 3 weeks after surgery.
Patients are commonly allowed to return to normal shoe wear by 4 weeks after the procedure.
Outcomes
- Conservative measures, such as changes in footwear, activity modification, and the addition of orthoses, may provide some degree of relief in up to about 50% of patients.
- Corticosteroid injections seem to provide successful relief from Morton’s neuroma about 50% of the time.
- Chemical nerve ablation and radiofrequency ablation also have a good success rate, with 70 to 80% of patients noting improvement after these interventions.
- Surgical intervention with neurectomy (removal of part of the nerve) or decompression of the nerve has the highest success rate, with most studies reporting an 80 to 95% success rate.
Even after successful surgical treatment, it is possible for a Morton's neuroma to come back. Approximately 5 to 20% of patients may have symptoms return and need additional treatment. Fortunately, a repeat surgery for Morton's neuroma recurrence has a similar success rate to the initial surgery (80 to 95%).
Summary
If you are experiencing any of the symptoms described above, you may benefit from an evaluation by an orthopaedic surgeon. Morton's neuromas can be quite bothersome, but it is often possible to get relief. These noncancerous nerve tumors typically respond well to current therapies such as orthoses, injections, or surgery.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.