Diseases & Conditions
Hemangiomas and Vascular Malformations
A hemangioma is a benign (noncancerous) tumor made up of blood vessels. There are many types of hemangiomas, and they can occur throughout the body, including in skin, muscle, bone, and internal organs.
Most hemangiomas occur on the surface of the skin or just beneath it. They often develop on the face and neck, and they can vary greatly in color, shape, and size.
Because hemangiomas very rarely become cancerous, most do not require any medical treatment. However, some hemangiomas can be disfiguring, and many people seek a doctor's care for cosmetic reasons.
In most cases of hemangioma, treatment does not involve surgery. Instances when surgery may be necessary include:
- For tumors that are deep in muscle or bone
- For tumors on the skin that cause problems with vision, breathing, or eating
Description - Hemangiomas
A hemangioma occurs when small blood vessels begin to multiply at an abnormal rate and form a mass or lump. It is possible to have more than one hemangioma.
There are several types of hemangioma. Some of the more common types include:
- Capillary hemangioma. This is the most common type of hemangioma. It is made up of small capillaries that are normal in size and diameter, but high in number. These capillaries form a tightly packed group held together by thin, connective tissue. When it develops in the skin, a capillary hemangioma is often referred to as "superficial." Due to their proximity (closeness) to the surface of the skin, capillary hemangiomas are typically bright red in color. They can vary in size and may be flat to the skin, raised, or stick out as a nodule. Some appear as a spongy mass that covers an entire arm or leg (these are called "diffuse hemangioma" or "angiomatosis").
- Cavernous hemangioma. In contrast with a capillary hemangioma, a cavernous hemangioma is made up of larger blood vessels that are dilated (widened). The blood vessels are not as closely packed as in a capillary hemangioma, and the spaces (or "caverns") between them are filled with blood. When they develop in the skin, cavernous hemangiomas are often referred to as "deep," and sometimes first appear as a bluish swelling underneath the skin. Like capillary hemangiomas, this type also varies greatly in size and can occur throughout the body.
- Compound hemangioma. Some hemangiomas are a mix of the capillary and cavernous types.
- Lobular capillary hemangioma (pyogenic granuloma). These small, red bumps often appear on the hands, face, and arms. Because they contain so many blood vessels, they bleed easily — often with just mild contact. This type of hemangioma is also sometimes referred to as a "pregnancy tumor" because they often appear during pregnancy, typically in the nose and mouth.
Infantile Hemangioma
Hemangiomas of the skin are common in infants — hence, people will call them "stork bites." They are sometimes present at birth, but most typically appear within the first weeks or months of life. Girls are affected slightly more often than boys.
Most infant hemangiomas are capillary hemangiomas, although cavernous and compound types do occur.
Common infantile hemangiomas follow the same growth pattern: a period of rapid growth, often during the first year, followed by a period of tumor shrinkage (called involution or regression).
- Most infantile hemangiomas will completely regress (shrink) on their own and require no treatment. The timeframe for rapid growth and then involution varies greatly, but most infantile hemangiomas have finished involution by the time the child reaches puberty.
- However, some hemangiomas can cause problems with vital functions like breathing, eating, and seeing, and therefore require some form of treatment. Because these tumors can grow to be large and often appear on the face, neck, and scalp, a child's emotional needs must be considered when determining treatment options.
Hemangiomas that are present at birth (called congenital hemangioma), follow a different growth pattern. These hemangiomas are fully grown at birth and either:
- Completely involute (shrink) during a baby's first year (called rapidly involuting congenital hemangioma), or
- Do not involute at all (called non-involuting congenital hemangioma)
Hemangiomas in Muscle, Bone, and Internal Organs
Although not as common as hemangiomas of the skin, hemangiomas do develop in other tissues, including muscle and bone.
Intramuscular hemangioma. Hemangiomas in muscle tissue can develop at any age, but they most often occur in young adults. Capillary hemangiomas are more common in muscle than cavernous and compound types. Any muscle can be involved.
Because they are located within the muscle, these hemangiomas often show no visible signs, although some may cause swelling and pain that increase with activity. These tumors are often painful and require treatment.
Bone hemangioma. The hemangiomas that occur in bones typically occur in the skull or spine and are most common in people who are 50 to 70 years of age. Capillary and cavernous types are the most common hemangiomas found in bone. They can grow on the surface or deeper into the center canal of a bone. Because they typically do not cause symptoms, these tumors are often found incidentally (by chance) when an X-ray or MRI image is obtained for another purpose.
Internal organ hemangioma. Although uncommon, hemangiomas can develop in internal organs, most often the liver and intestines. Like hemangiomas found in bone, hemangiomas in internal organs are often found by chance during tests for another purpose. Unless they are causing symptoms, these hemangiomas do not require any treatment.
Description - Vascular Malformations
Hemangiomas are often confused with vascular malformations, which are clusters of blood vessels that develop in arteries, veins, capillaries, or lymphatic vessels. Common types of vascular malformations include arteriovenous malformations (AVMs) and vascular ectasias.
Vascular malformations occur during fetal development. Although present at birth, some types of vascular malformations may not cause symptoms until adulthood.
Vascular malformations differ from infantile hemangiomas in that they slowly grow along with the child and become more apparent with age. Because they do not shrink or go away on their own, many types of vascular malformations in children require treatment.
Fibroadipose Vascular Anomalies (FAVA)
Fibroadipose vascular anomalies (FAVA) are rare, painful vascular anomalies that invade muscle with tough, fibrous, and fatty tissue. They are most commonly found in children and teens.
FAVA lesions were previously grouped in the same family as intramuscular AVMs (arteriovenous malformations). With advances in pathology and genetic analysis, these tumors are now seen as a unique diagnosis. It has been discovered that FAVA tumors often have a mutation in the PIK3CA gene – though, the tumors do not appear to be inherited (passed along in families).
FAVA lesions can lead to:
- Severe pain
- Contractures (shortening and/or tightening of muscle fibers)
- Disability
Initial (conservative) treatment may include:
- Compression garments
- Bracing
- Physical therapy
- Sclerotherapy (blocking the blood vessels that feed the tumor)
- Cryoablation (freezing the tumor)
- Medications (sirolimus — a medication that works on the PIK3CA gene pathway)
However, FAVA lesions often do not respond to typical conservative treatment options. As a result, many patients with a FAVA tumor may require surgery.
Cause
Different types of hemangiomas are associated with different causes, although exactly why hemangiomas develop is not well understood. For example:
- Infantile hemangiomas are caused by errors in the development of the vascular system that occur during fetal development but, in many cases, the event that caused the error cannot be identified.
- Some hemangiomas develop after an injury, but whether an injury can cause a hemangioma has not been proven.
- Some hemangiomas develop with pregnancy and resolve (go away on their own) after delivery.
- Some hemangiomas are associated with genetic abnormalities (for example, cavernous hemangiomas in von Hippel-Lindau disease).
There has been no proven connection between the development of hemangiomas and any particular occupation or exposure to chemicals or radiation. In addition, no known food, medication, or activity during pregnancy is known to cause a hemangioma in an infant.
Symptoms
Hemangiomas are:
- Usually painless, red to blue colored lesions on the skin, lips, or inside the mouth
- Often soft to the touch
- Most often flush with the skin or slightly elevated, but sometimes they grow from a stalk
Superficial lesions may bleed or turn into sores, particularly if bumped or injured.
Deep hemangiomas in muscle may cause pain, as well as swelling around the hemangioma that increases with activity.
Hemangiomas in bones may cause pain and enlargement of the bone.
Doctor Examination
Hemangiomas can be confused with other vascular malformations. Because treatment may vary considerably depending on whether the lesion is a hemangioma or other type of malformation, a thorough doctor's examination is recommended.
Medical History and Physical Examination
Before a physical examination, your doctor will talk with you about your general health and current condition — or that of your child's, if you are a parent or family member. To get a good understanding of the lesion and its history, the doctor may ask:
- How long the mass or lesion has been present
- Whether/how the mass or lesion has changed — including any changes in size — over time
- Whether other symptoms — such as swelling and pain — are associated with the lesion, when those symptoms began, and which activities make the symptoms better or worse
During the physical examination, the doctor will inspect and palpate (feel) any mass, noting exactly where it is located, what it feels like, and perhaps any surrounding changes in the skin.
Tests
Although doctors can often diagnose hemangiomas based on medical history and physical examination alone, imaging tests can be helpful.
X-rays and computerized tomography (CT) scans. Although plain X-rays and CT scans are better for creating pictures of dense structures like bone, these imaging tests may show a cavernous hemangioma if it has calcifications (areas that have become hard, like stone; in fact, these calcifications are called phleboliths, which means "stone in the blood vessel" in Greek).
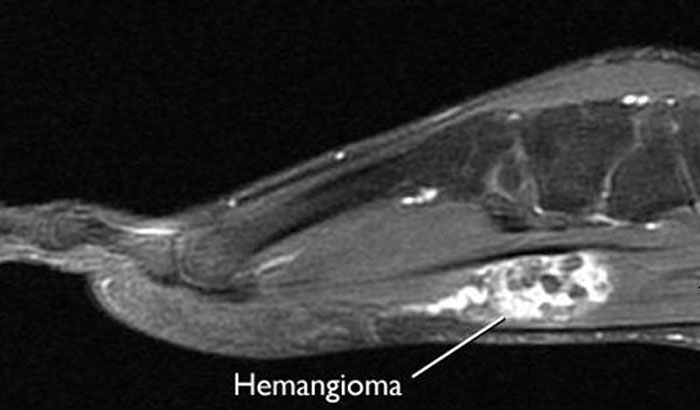
Magnetic resonance imaging (MRI) scans. MRI scans can create clear images of soft structures like a hemangioma. Hemangiomas in an MRI scan are often described as a "bag of worms" due to the way the blood vessels pack around one another.
Angiogram. In this test, dye is injected into the surrounding blood stream making the hemangioma show up in an X-ray image.
Biopsy. At times, it may be difficult to tell hemangiomas apart from other tumors, and a biopsy may be needed to confirm a diagnosis of hemangioma. In a biopsy, a tissue sample is taken from the tumor and examined under a microscope. Looking at the tissue under a microscope may be the best way to tell if the tumor is indeed a hemangioma and, if so, which subtype it is.
During the biopsy, your doctor may give you a local anesthetic to numb the area and take a sample using a needle. Biopsies can also be performed with a small incision.
Blood tests. If there are multiple tumors or if your symptoms are concerning for a specific disease pattern, your doctor may recommend blood tests for genetic analysis.
Differential Diagnosis
The imaging and tissue tests help your doctor tell hemangioma apart from other types of vascular malformations and soft-tissue tumors.
It is very important in planning treatment to distinguish hemangioma from more aggressive, cancerous vascular tumors like angiosarcoma.
Treatment
Treatment varies slightly by hemangioma subtype.
Nonsurgical Treatment
Observation. Although a hemangioma may not require any treatment, it is important to visit your doctor regularly to monitor any changes in the tumor.
Beta blocker medication. Beta blockers are a medication that may be recommended depending on the type and size of a hemangioma. For certain types, such as superficial and infantile hemangiomas, beta blockers (a pill medication) may be given with the goal of slowing the lesion’s growth.
Anti-inflammatory medication. If a hemangioma is growing near vital structures, such as the nose, lips, or eyelids, your doctor may recommend steroid medication. Steroids are often used to slow down the growth of the tumor. The drugs may be injected directly into the hemangioma or given orally (by mouth).
Compression. Intermittent pneumatic compression is a treatment that uses inflatable sleeves or leggings to apply pressure to the tumor. It can help decrease the swelling associated with a hemangioma. It will not, however, make the hemangioma go away.
Embolization or sclerotherapy. In these procedures, the blood supply to the tumor is closed off.
- Embolization is a minimally invasive procedure where small particles are injected into the blood vessels to block them off.
- Sclerotherapy is a similar procedure where chemical agents are used to close off the vessels.
These procedures can be very helpful in shrinking the tumor and decreasing pain. Often, however, the tumor will regrow its blood supply over time after these procedures. Embolization is also sometimes used before surgery to reduce the risk of heavy blood loss.
Laser treatment. For some patients, lasers can be helpful in removing a tumor, preparing a tumor for other treatments, or decreasing pain and other unwanted symptoms. Depending on the size of the tumor and its location, multiple laser treatments may be needed. Laser treatment is typically reserved for hemangiomas involving the skin.
Surgical Treatment
Surgery may be recommended for a cavernous hemangioma if the lesion is destroying the healthy tissues surrounding it. In some cases, a hemangioma can cause painful symptoms severe enough to consider surgical treatment.
Procedure. The procedure to surgically remove a hemangioma is called an excision. After general anesthesia is used to put you to sleep, your doctor will make an incision in your skin and cut the tumor out.
Recovery. You will likely have stitches, which your doctor will remove within a few weeks. Your doctor will wrap the area with a compressive bandage and provide you with specific instructions about activity restrictions to guide your recovery.
Complications. The most common complications of surgery to remove a hemangioma are blood loss and local recurrence (the tumor grows back).
Research
There is currently a great deal of research attempting to learn more about unregulated vascular proliferation, including hemangiomas.
The development of anti-angiogenesis inhibitors or anti-angiogenic agents — medications that halt the development of the blood vessels that feed tumors and enable them to grow — is an exciting area of research for many types of tumors.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.