Diseases & Conditions
Heel Pain
Every mile a person walks puts 60 tons of stress on each foot. Feet can handle a heavy load, but too much stress pushes them over their limits. The result is often heel pain — the most common problem affecting the foot.
Anatomy
The bones of the feet are commonly divided into three parts:
- The hindfoot (back of the foot)
- The midfoot (middle of the foot)
- The forefoot (front of the foot)
The heel bone is the largest bone in the foot. It lies at the back of the foot (hindfoot).
- The Achilles tendon extends down from the calf muscle and attaches to the back of the heel.
- The plantar fascia is a thick band of tissue that runs along the bottom of the foot and attaches to the plantar surface of the heel bone.
Both of these attachments — the places where soft tissues attach to bone — can become inflamed and be the source of heel pain.
Cause
Heel pain can have many causes, which generally fall into two categories.
Pain beneath the heel may be caused by:
- Stone bruise. Stepping on a hard object, such as a rock or stone, can bruise the fat pad on the underside of the heel. The bruised area may or may not look discolored.
- Plantar fasciitis. Too much running or jumping can inflame the tissue band (fascia) connecting the heel bone to the base of the toes. This inflammation can be worsened by performing these activities in older shoes with worn-out cushioning. Learn more: Plantar Fasciitis and Bone Spurs
- Heel spur. When plantar fasciitis goes untreated for a long time, a heel spur (calcium deposit) may form where the fascia tissue band connects to the heel bone. A heel spur is usually the result of the problem (long-standing plantar fasciitis) and not the cause of the pain.
- Calcaneus stress fracture. Repetitive stress to the calcaneus from high impact activities can eventually wear out and fracture the bone. Learn more: Stress Fractures of the Foot and Ankle
- Nerve entrapment. Repetitive impact activities can cause swelling and nerve inflammation underneath the heel bone.
- Calcaneus fracture. The calcaneus (heel bone) is most often fractured during a fall from a height or a motor vehicle collision. These fractures are uncommon, but when they do occur, they can be quite severe and often require surgery to reconstruct the normal anatomy of the heel and restore mobility. Learn more: Calcaneus (Heel Bone) Fractures
Pain behind the heel may be caused by:
- Retrocalcaneal bursitis. People who have pain behind their heel may have inflamed the area where the Achilles tendon inserts onto (attaches to) the heel bone. This can be the result of running too much, or wearing shoes that rub or cut into the back of the heel.
- Insertional Achilles tendinosis. This condition results from the breakdown of collagen in the Achilles tendon at the place where the tendon attaches to the heel bone. Over time, the tendon becomes thickened, causing pain.
Whatever the cause, continued impact on a sore heel will only worsen the pain and may lead to additional problems.
Symptoms
- Symptoms of heel pain often include swelling and tenderness.
- With plantar fasciitis, the pain is centered under the heel and may be mild at first. The pain flares up when taking first steps out of bed in the morning or when stepping out of a car after a long drive. Even getting up from a chair after sitting for awhile can cause pain.
- Pain behind the heel may build slowly over time, causing the skin to thicken, get red, and swell. The pain flares up when first starting an activity after resting. Wearing normal shoes often also causes pain.
- People with pain behind the heel may also develop a bump on the back of the heel that feels tender and warm to the touch. People born with this bump are more likely to experience heel pain as they get older.
Doctor Examination
Medical History and Physical Examination
During the appointment, your doctor will:
- Ask you about your heel pain and symptoms.
- Examine the bottom and back of your heel, looking and feeling for signs of tenderness and swelling that may indicate plantar fasciitis or retrocalcaneal bursitis.
- Possibly squeeze your heel to determine if you have a stress fracture.
- Possibly ask you to walk, stand on one foot, or do other physical tests to help your doctor pinpoint the cause of your pain.
- Check your range of motion and flexibility.
Imaging Tests
X-rays. When heel pain continues for a long time, your doctor may order X-rays to evaluate the root cause of the pain. X-rays can help your doctor diagnose heel pain due to plantar fasciitis, calcaneus stress fracture, insertional Achilles tendinosis, and other issues that cause heel pain.
Magnetic Resonance Imaging (MRI) Scan. An MRI is rarely needed to diagnose heel pain. However, if initial nonsurgical treatment is not effective, and X-rays do not reveal the cause of your heel pain, your doctor may order an MRI scan. An MRI can help your doctor better evaluate the Achilles tendon, or diagnose a calcaneus stress fracture, retrocalcaneal bursitis, plantar fasciitis, or other soft tissue-related sources of pain.
Treatment
If your heel hurts, see your doctor right away to determine why it hurts and get treatment.
Treatment will depend largely on the cause of the pain.
Nonsurgical Treatment
Heel pain rarely requires surgery. Conservative (nonsurgical) treatments include:
- Rest. Rest your foot as much as you can until the pain goes away. Heel pain that is the result of a stone bruise will gradually go away completely with rest.
- Icing. If your pain is located behind the heel, consider placing ice on the back of the heel to reduce inflammation. Apply ice 20 minutes on/20 minutes off. Do not apply ice directly to the skin; use an ice pack, or wrap the ice in a towel or cloth.
- Non-steroidal anti-inflammatory drugs (NSAIDs). Your doctor may recommend you take an NSAID, such as ibuprofen, to reduce swelling.
- Tape. Placing tape around the heel may help reduce pain and promote healing in patients with plantar fasciitis.
- Shoe inserts. Your doctor may recommend that you wear heel pads or heel cup inserts. Patients with a torn Achilles tendon may also want to wear open-backed shoes.
- Night splinting: Your doctor may prescribe a splint for you to wear at night, which can be effective in reducing pain first thing in the morning.
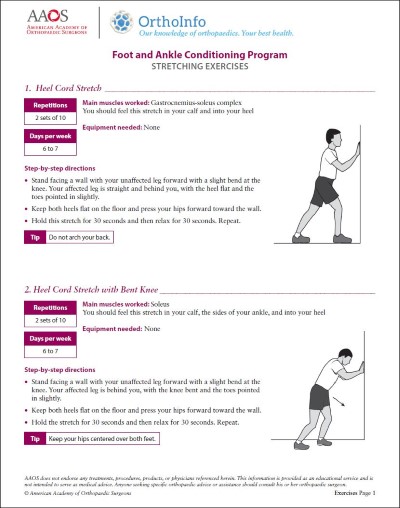
- Exercises. Your doctor may suggest special exercises. For example, leaning forward against a wall with your foot flat on the floor and heel elevated with the insert to stretch the Achilles tendon. Restoring flexibility in the calf muscle, Achilles tendon, and plantar fascia is a critical step in relieving heel pain and keeping symptoms from coming back.
Note: Heel pain that has been going on for a long time often requires a long time to improve. Your doctor will likely recommend several of these conservative treatments and explain that it may take several months of treatment before your symptoms improve.
Surgical Treatment
Most heel pain can be treated without surgery. If your heel paint has not improved after months of conservative treatment, your doctor may recommend surgery.
Surgical solutions target the anatomic source of the heel pain. Learn more about specific surgical treatment for:
- Insertional achilles tendinitis
- Plantar fasciitis
Conclusion
Heel pain is a common foot problem. There are multiple causes of pain on the back, side, or bottom of the heel.
Clinical evaluation with a thorough exam is needed to diagnose the root cause of heel pain and to determine an appropriate treatment plan.
A sore heel will usually improve on its own without surgery — if you avoid placing significant impact on the heel and perform exercises to improve the damaged tissue.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.