Diseases & Conditions
Hammer Toe: Comprehensive Guide
A hammer toe is a deformity of the second, third, or fourth toes. In this condition, the toe is bent at the middle joint, so that it resembles a hammer.
Initially, hammer toes are flexible and can be corrected with simple measures; however, if left untreated, they can become fixed and require surgery.
Anatomy
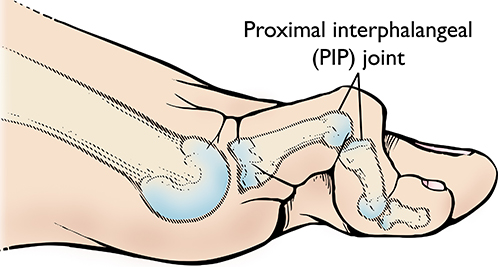
The forefoot is made up of five toes. Each toe has three joints — except for the first (big) toe, which usually has only two joints.
In hammer toe, the affected toe is bent at the middle joint, which is called the proximal interphalangeal (PIP) joint.
Cause
Hammer toe is the result of a muscle imbalance that puts pressure on the toe tendons and joints. Muscles work in pairs to straighten and bend the toes. If the toe is bent in one position long enough, the muscles and joints tighten and cannot stretch out.
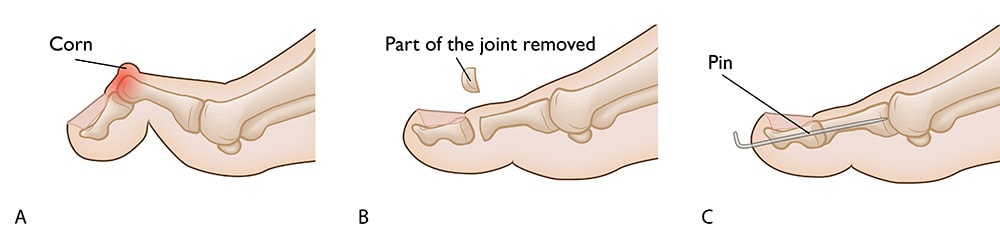
Wearing shoes that do not fit properly is a common cause of this imbalance. Shoes that narrow toward the toe push the smaller toes into a flexed (bent) position. The toes rub against the shoe, leading to the formation of corns and calluses, which further aggravate the condition. Shoes with a higher heel force the foot down and push the toes against the shoe, increasing the pressure and the bend in the toe. Other times, some of the small muscles in the foot can weaken over time and cause an imbalance. Eventually, the toe muscles can no longer straighten the toe.
Symptoms
A hammer toe is painful, especially when the patient is moving it or wearing shoes. Other symptoms may include:
- Swelling or redness
- Inability to straighten the toe
- Difficulty walking
- A corn or callus on the top of the middle joint of the toe or on the tip of the toe
Doctor Examination
Physical Examination
Your doctor will perform a physical examination to determine whether the toe joint is flexible or rigid. This information will help the doctor determine the appropriate treatment.
Tests
X-rays. X-rays provide images of dense structures, such as bone. Your doctor may order an X-ray of your foot to confirm the diagnosis.
Other tests. Patients who have diabetes or decreased sensation in their feet may require further testing to determine whether a neurological condition is the cause of the tendon imbalance.
Treatment
Nonsurgical Treatment
In the early stages of hammer toe — when the joint is still flexible — treatment typically consists of simple measures.
Changes in footwear. Your doctor will recommend that you avoid wearing tight, narrow, high-heeled shoes. Shoes should be one-half inch longer than your longest toe — which, for many people is the second toe — and have a soft, roomy toe box (the toe box is the part of the shoe that covers and protects your toes).
You may also be able to find a shoe with a deep toe box that makes room for the hammer toe. A shoe repair shop may be able to stretch a toe box so that it bulges out around the toe. Wearing sandals may help, if they do not pinch or rub other areas of the foot.
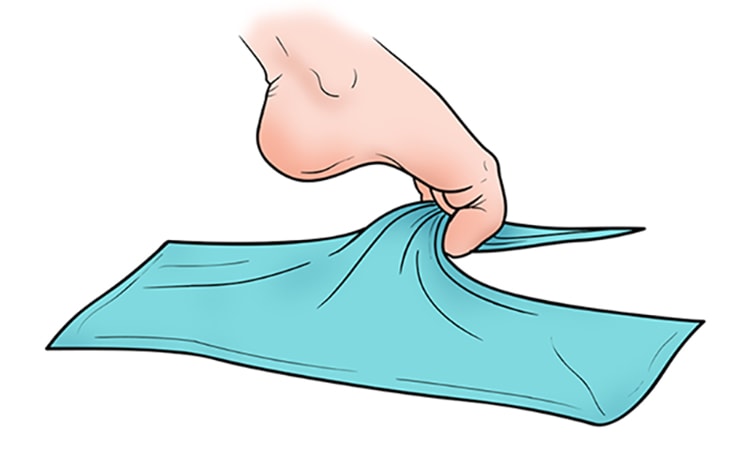
Exercises. Specific exercises can help stretch and strengthen the muscles in your foot. Your doctor may recommend gently stretching your toes manually (using your hands) or using your toes to pick things up off the floor. They may also recommend doing “towel curls” to strengthen the toes. To perform a towel curl, place a towel flat under your foot and use your toes to crumple (scrunch) it.
Over-the-counter remedies. Using commercially available straps, cushions or nonmedicated corn pads can help relieve pain. If you have diabetes, poor circulation, or a lack of feeling in your feet, talk to your doctor before attempting any self-treatment.
Surgical Treatment
If the toe joint is rigid and no longer moveable, or if nonsurgical treatment does not relieve your symptoms, your doctor may recommend surgery.
Surgery is typically performed on an outpatient basis using a local anesthetic. The actual procedure will depend on the type and extent of the deformity.
Tendon lengthening. For patients with a flexible toe joint, the condition can often be treated by lengthening the tendons that are causing the joint imbalance.
Tendon transfer. Some patients with a flexible toe joint may benefit from treatment that involves transferring tendons from the bottom of the toe to the top of the toe to help pull the joint into a straight position.
Arthrodesis (joint fusion). Patients who have a rigid toe joint may undergo tendon lengthening in combination with arthrodesis. In this procedure, your doctor will remove a small part of a bone in the toe joint to ensure that the toe can extend fully. He or she will then insert an external wire or pin and/or internal plate to hold the bones in place while the bones fuse together.
Recovery
After surgery, you may experience some stiffness, swelling and redness in your toe for up to 4 to 6 weeks.
Although you will be able to put pressure on the foot immediately after surgery, you should try to limit your activity while the toe heals. Elevating your foot as much as possible will help speed up healing and reduce pain.
Once healed, your toe may be slightly longer or shorter than it was before and will not be able to bend at the fused joint.
Contributed and/or Updated by
Peer-Reviewed by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.