Diseases & Conditions
Fibrous Dysplasia
Fibrous dysplasia is a benign (noncancerous) bone condition in which abnormal fibrous tissue develops in place of normal bone. As these areas of fibrous tissue grow and expand over time, they can weaken the bone — causing it to fracture or become deformed.
Some patients with fibrous dysplasia experience few or no symptoms. In other cases, however, multiple bones are affected and the condition is more severe. These patients may need surgery to remove the affected areas of bone and prevent or repair any fractures or deformity.
Description
Fibrous dysplasia is rare, accounting for just about 7% of all benign bone tumors. It can affect any bone in the body, but most often occurs in the:
- Femur (thighbone)
- Tibia (shinbone)
- Ribs
- Skull
- Humerus (upper arm bone)
- Pelvis
Fibrous dysplasia has been linked to a gene mutation that causes bone cells to make an abnormal type of fibrous bone. Although the abnormal bone begins to form before birth, its presence is often not discovered until childhood, adolescence or even adulthood.
The condition is generally divided into two types:
- Monostotic fibrous dysplasia — Only a single bone is affected. This is the most common form of the condition.
- Polyostotic fibrous dysplasia — More than one bone is involved. It can affect more than one bone within the same limb or multiple bones throughout the body. This form of the condition is usually more severe. For this reason, it is typically discovered earlier in life.
Fibrous dysplasia is a chronic disorder and is often progressive. Although the lesions may stabilize and stop growing, they do not disappear. Individual lesions may progress more rapidly in the polyostotic form of the condition and in growing children.
In patients with fibrous dysplasia, the same abnormality that occurs in the bone cells can also occur in the body's gland cells, leading to hormonal abnormalities. Although this is rare, it can occur in severe forms of polyostotic fibrous dysplasia.
Fibrous dysplasia may occur as part of a larger disorder. For example, McCune-Albright syndrome is characterized by polyostotic fibrous dysplasia that occurs with hormonal abnormalities and areas of darkened skin ("café au lait" spots).
It is very rare for areas of fibrous dysplasia to become malignant or cancerous. This occurs in less than 1% of patients and is more likely to happen in patients with the polyostotic form of the condition or in patients with McCune-Albright syndrome.
Cause
The cause of the gene mutation is unknown. It is not inherited and is not known to be caused by diet or environmental factors. The mutation occurs equally in males and females of all races.
Symptoms
In some cases, lesions are painless and do not cause symptoms. When this happens, the condition may be found unexpectedly when X-rays or tests are performed for an unrelated injury or medical condition. When symptoms do occur, they reflect the size and severity of the lesion.
Pain
As fibrous bone tissue grows and expands, the affected area can become weak and painful. Pain is more likely to occur if the bone affected is one of the weight-bearing bones of the leg or pelvis.
Pain caused by fibrous dysplasia generally begins as a dull ache that worsens with activity and lessens with rest. It can get progressively worse over time.
Fracture
Fibrous bone is very weak when compared to normal bone. It can sometimes break or fracture through the weakened area causing sudden and severe pain. A fracture often occurs after a period of dull pain — although it may also happen suddenly with no prior pain at all.
Bone Deformity
In patients who experience repeated fractures, poor healing can lead to bone deformity. If this deformity occurs in the facial bones or results in curving of the leg bones, it can become very noticeable.
Severe deformity in the facial bones can lead to loss of vision or hearing. If the legs or pelvis are involved, the patient may have trouble walking or may develop arthritis in nearby joints.
Hormonal Disturbances
Patients with hormonal abnormalities can experience a number of symptoms.
Young patients with hormonal abnormalities may develop early puberty. This problem is more common in girls than boys and is caused by hyperactivity of the ovaries. Hyperactivity may also occur in other glands of the body, including the:
- Thyroid gland (causing anxiety, weight loss, and abnormal sweating)
- Adrenal glands (causing weight gain and diabetes)
- Pituitary gland (causing milk production in women, gigantism, and a hormonal disorder called acromegaly)
- Parathyroid glands (causing high levels of calcium in the blood)
Females may experience increased pain during pregnancy or their menstrual cycle as the elevated hormone levels during these times can accelerate the growth of fibrous dysplasia.
Skin Discoloration
Pigmented skin spots (referred to as "café au lait" spots) are often seen in patients with hormonal abnormalities and fibrous dysplasia.
Changes in Symptoms
Very rarely, areas of fibrous dysplasia can become cancerous. When this occurs, warning signs may include a rapid increase in swelling or growth of a lesion. Patients may also experience increasing pain — especially pain that awakens them at night or does not go away with rest.
Doctor Examination
Physical Examination
During the exam your doctor will talk with you about your general health and medical history and ask about your symptoms.
Tests
X-rays and other tests will help your doctor confirm the diagnosis of fibrous dysplasia or determine the extent of the disorder.
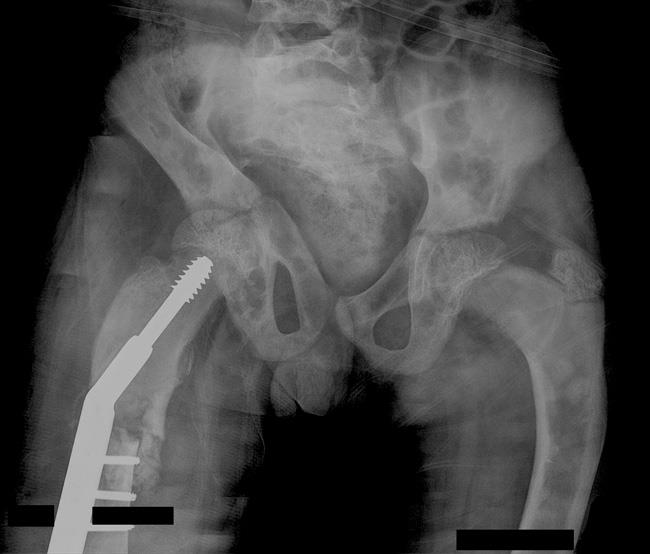
X-rays. X-rays provide images of dense structures such as bone. In a patient with fibrous dysplasia, an X-ray may show:
- An abnormal area of bone that has an appearance similar to that of ground glass
- Expansion of the involved area of bone
- Deformity of the bone, such as bowing or an abnormal curvature
Other imaging studies. Your doctor may order a magnetic resonance imaging (MRI) scan or computerized tomography (CT) scan to further evaluate the lesion. An MRI will more clearly show how much of the bone is involved and can be helpful in determining whether or not a lesion has become cancerous.
Although a fracture can generally be seen on an X-ray and/or MRI scan, a CT scan can sometimes help your doctor see the fracture better and determine the quality of the bone.
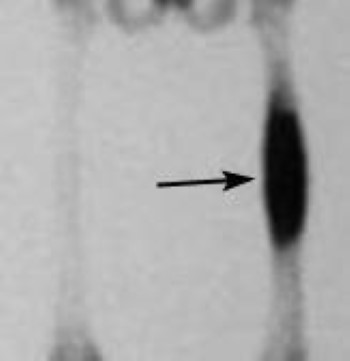
Bone scan. Your doctor may order a bone scan to look for additional lesions throughout your entire skeleton. During this test, a very small amount of radioactive dye is injected into the body intravenously. The scan will show a hot spot — an increased uptake of the radioactive material — in areas of abnormal bone.
Laboratory tests. When fibrous dysplasia lesions are actively growing, blood tests may show elevated levels of the enzyme alkaline phosphatase. Urine tests tend to show elevated levels of hydroxyproline. However, these abnormalities are not specific to fibrous dysplasia and are not always present. They can sometimes be seen in other medical conditions that involve bone growth — and can even be seen in normal bone growth.
Biopsy. A biopsy may be necessary to confirm the diagnosis of fibrous dysplasia. In a biopsy, a tissue sample from the lesion is taken and examined under a microscope.
A biopsy can be performed under local anesthesia with a needle or as a small open operation.
Treatment
Nonsurgical Treatment
Observation. If your lesions do not cause symptoms, your doctor may recommend observation and monitoring them to see if they progress. During this time, you may need periodic X-rays or other tests.
Medications. Bisphosphonates are medications that decrease the activity of cells that dissolve bone. They are available in easy-to-take pill form or intravenous (IV) infusions. Studies of bisphosphonates have shown some relief of the pain and decreased frequency of the fractures associated with the disorder.
Bracing. In some cases, bracing may be used to prevent fracture in weakened bones. However, bracing has not been shown to be effective in preventing progression of deformity.
Surgical Treatment
In patients with fibrous dysplasia, surgery is often necessary to remove a growth or to fix or prevent bone fractures. Your doctor may recommend surgery if you have:
- Symptomatic lesions that have not responded to nonsurgical treatment
- Displaced fractures — a break in which the pieces of bone have significantly separated from each other
- Small cracks in the bone that do not heal with casting or bracing
- Progressive deformity of the bone
- Lesions that have become cancerous
- Large lesions that could potentially cause a fracture
Curettage. Curettage is a surgical procedure commonly used to treat fibrous dysplasia. In curettage, the tumor is scraped out of the bone.
Bone graft. After curettage, the doctor may fill the cavity with a bone graft to help stabilize the bone. A bone graft is bone taken from a donor (allograft) or from another bone in your body (autograft) — most often the hip. Synthetic bone material can also be used to fill the cavity.
In some cases, the bone graft placed in the cavity can be resorbed and the fibrous dysplasia can recur.
Internal fixation. Metal rods or plates and screws may be used to fix a fracture or deformity, prevent bone breakage before it occurs, or stabilize the bone.
Research on the Horizon
Ongoing genetic research may lead to a better understanding of the exact gene mutation involved in fibrous dysplasia. Doctors may then be able to develop more effective nonsurgical treatments.
Newer generations of medications, including bisphosphonates and denosumab, are now easier to take and have fewer side effects. More experience with these medications may allow for more effective treatment of fibrous dysplasia as well.
Contributed and/or Updated by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.